CHAPTER 4 Fluids, Volume Regulation, and Volume Disturbances
1 Describe the functionally distinct compartments of body water, using a 70-kg patient for illustration
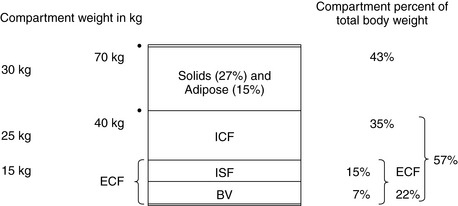
Accurate estimations are difficult because ordinarily ideal body weight (IBW) is used as a basis for calculation. Obesity is rampant in our society, making accurate estimations difficult. Figure 4-1 estimates body water compartments in a patient with an IBW of 70 kg.
2 Describe the dynamics of fluid distribution between the intravascular and interstitial compartments
3 How are body water and tonicity regulated?
 Hypothalamic osmoreceptors have an osmotic threshold of about 289 mOsm/kg. Above this level ADH release is stimulated.
Hypothalamic osmoreceptors have an osmotic threshold of about 289 mOsm/kg. Above this level ADH release is stimulated.5 List conditions that stimulate and inhibit release of antidiuretic hormone
TABLE 4-1 Conditions that Stimulate and Inhibit Release of Adrenocorticotropic Hormone
| Stimulates Adrenocorticotropic Hormone Release | Inhibits Adrenocorticotropic Hormone Release | |
|---|---|---|
| Normal physiologic states | Hyperosmolality | Hypo-osmolality |
| Hypovolemia | Hypervolemia | |
| Upright position | Supine position | |
| β-Adrenergic stimulation | α-Adrenergic stimulation | |
| Pain and emotional stress | ||
| Cholinergic stimulation | ||
| Abnormal physiologic states | Hemorrhagic shock | Excess water intake |
| Hyperthermia | Hypothermia | |
| Increased intracranial pressure | ||
| Positive airway pressure | ||
| Medications | Morphine | Ethanol |
| Nicotine | Atropine | |
| Barbiturates | Phenytoin | |
| Tricyclic antidepressants | Glucocorticoids | |
| Chlorpropamide | Chlorpromazine | |
| Results | Oliguria, concentrated urine | Polyuria, dilute urine |
7 List causes of diabetes insipidus
| Vasopressin Deficiency (Neurogenic Diabetes Insipidus) | Vasopressin Insensitivity (Nephrogenic Diabetes Insipidus) |
|---|---|
| Familial (autosomal-dominant) | Familial (X-linked recessive) |
| Acquired | Acquired |
| Idiopathic | Pyelonephritis |
| Craniofacial, basilar skull fractures | Postrenal obstruction |
| Craniopharyngioma, lymphoma, metastasis | Sickle cell disease and trait |
| Granuloma (sarcoidosis, histiocytosis) | Amyloidosis |
| Central nervous system infections | Hypokalemia, hypercalcemia |
| Sheehan’s syndrome, cerebral aneurysm, cardiopulmonary bypass | Sarcoidosis |
| Hypoxic brain injury, brain death | Lithium |
8 Discuss alternative treatments for diabetes insipidus
KEY POINTS: Fluids and Volume Regulation 
9 Define the syndrome of inappropriate antidiuretic hormone release. What is the primary therapy?
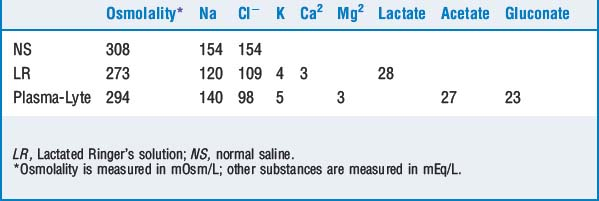
15 Review the composition of crystalloid solutions
Fluid resuscitation in the operating room is accomplished with isotonic fluids since intraoperative losses include both salts and water. Thus only relatively isotonic fluids are listed. Patients requiring replacement of maintenance fluids are usually treated with hypotonic fluids because their losses are predominantly free water, but this is uncommon intraoperatively. Although normal saline is the preferred crystalloid to dilute packed red blood cells, administering large quantities results in hyperchloremic metabolic acidosis caused by dilution of bicarbonate (Table 4-3).
16 Review the colloidal solutions that are available
Dextrans are water-soluble, polymerized glucose molecules. Two preparations are available (dextran 40 and 70), and the molecular weights of the respective solutions are 40 and 70 kilodaltons. Anaphylactic and anaphylactoid reactions and inhibition of platelet adhesiveness have been noted. Crossmatching of blood may be difficult (Table 4-4).
| Colloid | Benefits and Risks |
|---|---|
| Albumin (5% or 25%) | Expensive; allergic reactions; question its use where there is a loss of capillary integrity |
| Hetastarch | Currently constituted in either NS or RL; administer less than 20 ml/kg to avoid antiplatelet effects; renally excreted; increases serum amylase |
| Dextran (40 or 70) | Anaphylactic reactions; interferes with platelet function and crossmatching; increases hepatic transaminases |
LR, Lactated Ringer’s solution; NS, normal saline.
17 What is the normal range for serum osmolality?
where the values in the brackets are the concentrations of the substances (sodium in mEq/L, glucose and BUN in g/L).
1. Ellision D.H., Berl T. The syndrome of inappropriate antidiuresis. N Engl J Med. 2007;356:2064-2072.
2. Growcott M.P.W., Mythen M.G., Gan T.J. Perioperative fluid management and clinical outcomes in adults. Anesth Analg. 2005;100:1093-1106.
3. Nisanevich V., Felsenstein I., Almogy G., et al. Effect of intraoperative fluid management on outcome after intraabdominal surgery. Anesthesiology. 2005;103:25-32.