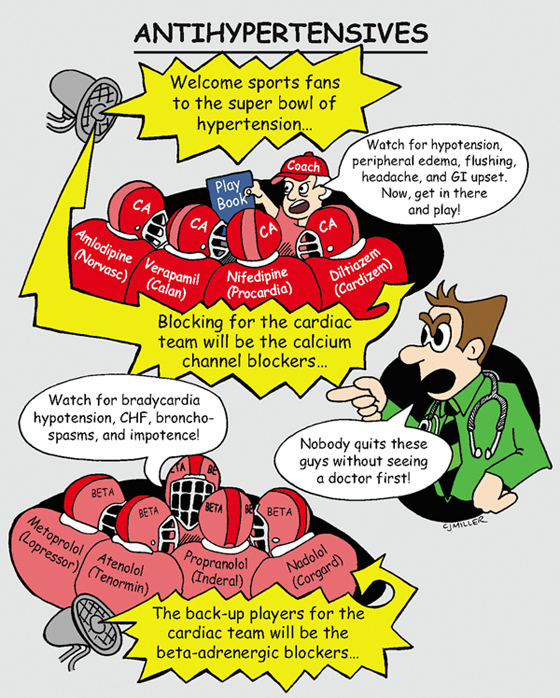
Antihypertensives
ACTIONS
Antihypertensive drugs act on the vascular, cardiac, renal, and sympathetic nervous systems. They also act to lower blood pressure (BP), cardiac output, and peripheral vascular resistance.
USES
• Control mild-to-severe hypertension
CONTRAINDICATIONS
• Cerebrovascular insufficiency
PRECAUTIONS
• Uncontrolled congestive heart failure, thyrotoxicosis
• Beta blockers can mask symptoms of hypoglycemia in patients with diabetes
• Hepatic and renal dysfunctions
SIDE EFFECTS
• **Hypotension, sedation, sexual dysfunction**
• Calcium channel blockers—bradycardia, peripheral edema, constipation
• Beta blockers—bradycardia, decreased atrioventricular (AV) conduction, reduced cardiac contractility, †bronchoconstriction†
NURSING IMPLICATIONS
2. ‡Teach patients about orthostatic hypotension for initial dosing (e.g., get up slowly) and other lifestyle changes—weight reduction, sodium restriction, and daily exercise.‡
3. *Monitor electrolyte, hepatic, and renal serum blood studies.*
4. *Avoid abrupt withdrawal of drug; may cause rebound phenomenon of excessive rise in BP.*
5. *Methyldopa (Aldomet) is the drug of choice for hypertension in pregnancy.*
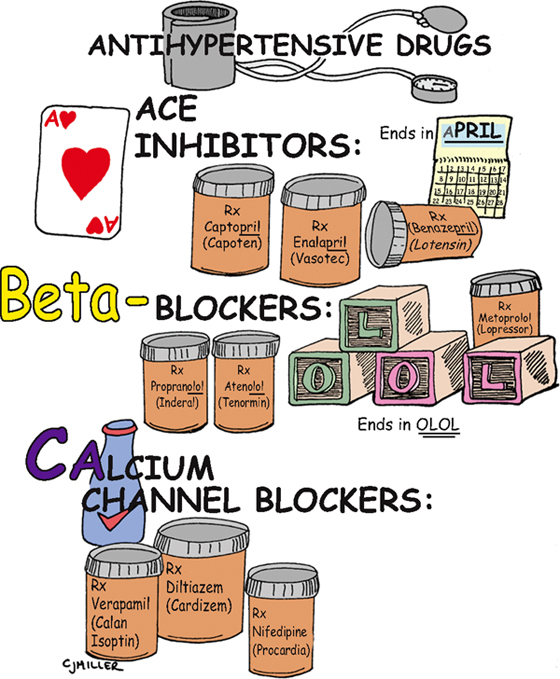
Antihypertensive Drugs
CLASSIFICATION
Blood pressure is regulated by cardiac output (CO) and peripheral vascular resistance (PVR). Medications that influence either one of these systems lead to blood pressure control. Antihypertensive drugs that influence these systems to lower the blood pressure are angiotensin-converting enzyme (ACE) inhibitors, beta-adrenergic blockers, and calcium channel blockers (CCBs).
ACTIONS
• A—ACE inhibitors block the conversion of angiotensin I to angiotensin II, a vasoconstrictor. This block causes vasodilation and therefore decreases PVR, resulting in a decrease in blood pressure. Aldosterone is also blocked, causing a decrease in sodium and water retention.
USES
• Mild-to-moderate essential hypertension
• Either as separate drugs or frequently in combination with another drug
NURSING IMPLICATIONS
1. *Initial drug selection starts with a thiazide diuretic, typically followed by a beta-adrenergic blocker or an ACE inhibitor or CCB.*
2. ‡Take medication as prescribed; do not stop abruptly.‡
3. ‡Teach patient never to double-up on doses if a dose is missed.‡
4. ‡Change positions slowly; watch for postural hypertension.‡
5. ‡Avoid over-the-counter medications.‡
6. ‡Take caution in hot weather, hot showers, hot tub baths, or prolonged sitting or standing because these may aggravate low blood pressure.‡
7. ‡Teach patients about multidrug therapy; instruct them not to discontinue a previous antihypertensive medication when another medication is started.‡
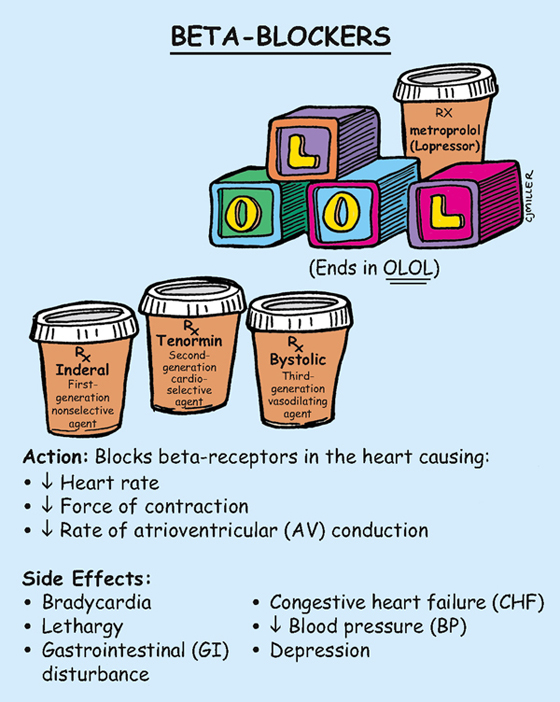
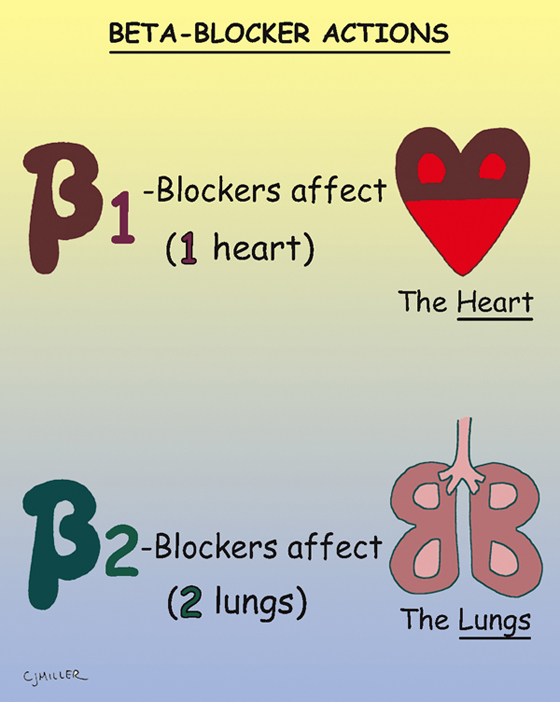
Beta-Blockers
ACTIONS
Beta1 action is primarily on the heart—decreases rate, decreases force of contraction, and delays impulse conduction. Beta2 action is primarily on the heart, but it also blocks receptors in the lungs and can cause bronchoconstriction.
USES
• Uncomplicated hypertension, dysrhythmias; angina
CONTRAINDICATIONS
• Bradydysrhythmias, atrioventricular (AV) block
• Beta2 in chronic respiratory problems
PRECAUTIONS
• Hepatic and renal dysfunction, diabetes
• History of depression, heart failure
SIDE EFFECTS
• Headache, flushing, dizziness, **fatigue, weakness,** bradycardia
• Postural hypotension, †bronchospasm, bronchoconstriction†
• Decreased cardiac output, †congestive heart failure (CHF)†
NURSING IMPLICATIONS
1. Assess for symptoms of heart failure.
2. ‡Instruct the patient to report any weakness, dizziness, or fainting.‡
3. *Before giving, evaluate the patient’s blood pressure and pulse for significant changes. Hold if systolic blood pressure is below 90 mm Hg.*
4. *Monitor patients with diabetes, because tachycardia (a symptom of hypoglycemia) is often masked as a result of the beta1 blockade.*
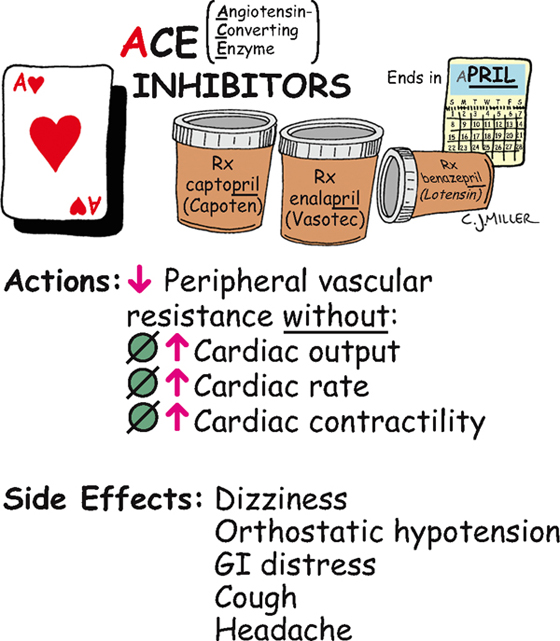
Angiotensin-Converting Enzyme (ACE) Inhibitors
ACTION
Suppress formation of angiotensin II from the renin-angiotensin-aldosterone system, reduce peripheral resistance, and improve cardiac output.
USES
CONTRAINDICATIONS
• Second- and third-trimester pregnancies
PRECAUTIONS
• Renal impairment, collagen vascular disease
SIDE EFFECTS
• Headache, dizziness, **postural hypotension (especially the first dose)**
• **Altered sense of taste, hyperkalemia**
• **Nagging, nonproductive cough**
NURSING IMPLICATIONS
1. Regularly *monitor blood pressure,* especially for 2 hours after the first dose, because severe first-dose hypotension often develops.
2. ‡Teach patient to rise slowly from a lying to a sitting position to reduce postural hypotensive effects.‡
3. *Before administering, assess the patient for history or presence of renal impairment.*
4. *Administer on an empty stomach for best absorption.*
5. ‡Teach patient to notify health care provider if cough develops.‡
6. ‡Teach patient to avoid potassium supplements or potassium-containing salt substitutes.‡
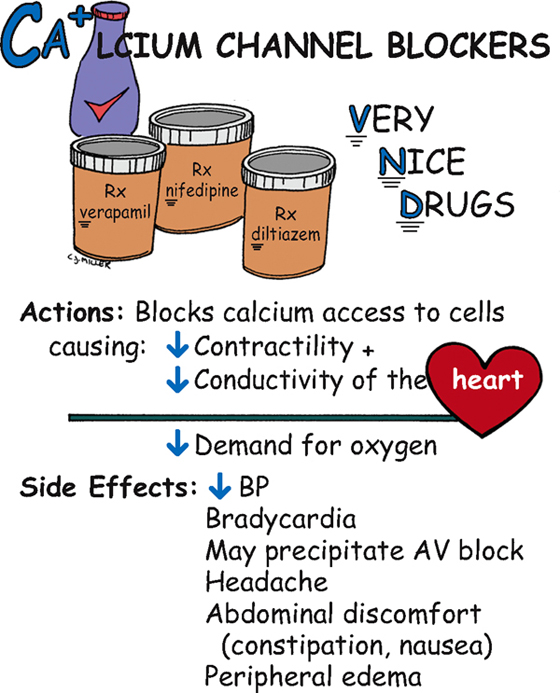
Calcium Channel Blockers
ACTION
Block calcium access to the cells, causing decreased heart contractility and conductivity and leading to a decreased demand for oxygen.
USES
• Angina, hypertension, and dysrhythmias (verapamil and diltiazem)
CONTRAINDICATIONS
• nifedipine: hypersensitivity
PRECAUTIONS
• Renal or hepatic insufficiency may develop.
• Avoid giving verapamil or diltiazem with beta blockers and digoxin.
SIDE EFFECTS
• Decreased blood pressure, **edema of the extremities,** headache
• Constipation (verapamil), nausea, skin flushing, †dysrhythmias†
NURSING IMPLICATIONS
1. Administer before meals; may be taken with food if needed; *do not crush or allow patient to chew sustained-release medication preparations.*
2. *Monitor vital signs and watch for low blood pressure.*
3. ‡Teach about postural hypotension.‡
4. Check liver and renal function studies.
5. *Weigh patient; report any peripheral edema or weight gain.*
6. ‡Teach patient to avoid grapefruit.‡
7. ‡Teach patient that constipation can be minimized by increasing dietary fiber and fluid.‡
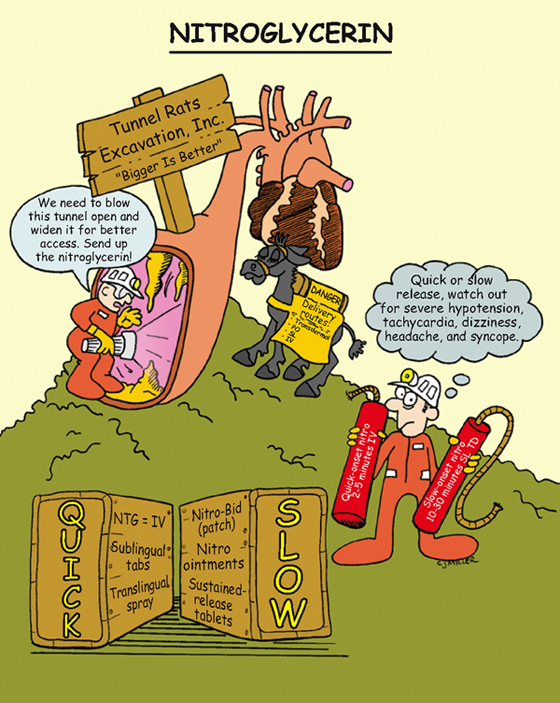
Nitroglycerin
ACTIONS
Nitrate vasodilator relaxes vascular (arterial and venous) system with more prominent effects on veins, which decreases preload. Arteriolar relaxation reduces systemic vascular resistance, which decreases afterload.
USES
• In conjunction with beta blockers or calcium channel blockers to suppress tachycardia
CONTRAINDICATIONS AND PRECAUTIONS
• Hypersensitive patients, severe anemia
• Erectile dysfunction medications (Viagra)
• Severe hepatic or renal disease and use of other vasodilators
• Beta blockers, verapamil, diltiazem
SIDE EFFECTS
• Orthostatic **hypotension,** headaches, tachycardia, dry mouth, blurred vision
NURSING IMPLICATIONS
1. ‡Patients with angina pectoris should carry nitrates with them at all times.‡
2. ‡Teach proper storage for freshness (tingling, fizzle sensation under tongue). Discard unused medication after 24 months.‡
3. ‡Teach patient to call 9-1-1 if pain is not relieved within 5 minutes of taking. May take one tablet every 5 minutes for a total of three tablets while waiting for emergency care.‡
4. Avoid alcoholic beverages during nitrate therapy.
5. Avoid swallowing or chewing sustained release tablets to help drug reach gastrointestinal system. ‡Place buccal tablets between cheek and gum.‡
6. *Rotate transdermal patches and remove after 12 to 14 hours to have a “patch free” interval of 10 to 12 hours daily.*
7. *In hospitalized patients, check BP before administering.*
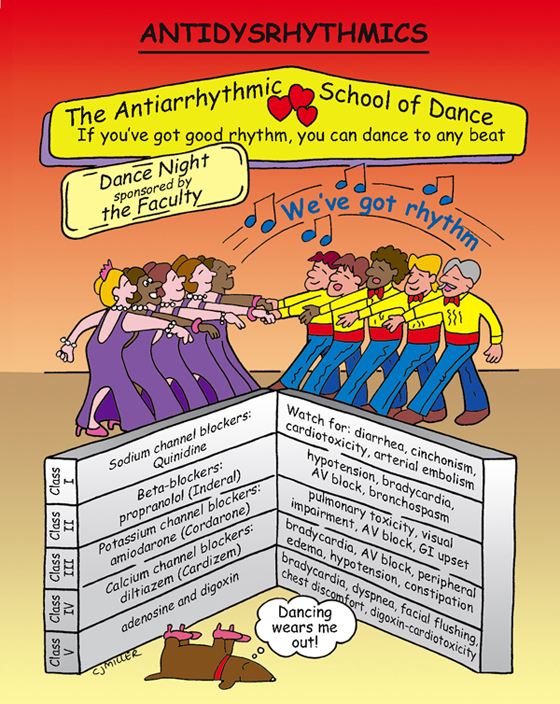
Antidysrhythmics
ACTIONS
• Sodium channel blockers block sodium, slowing the impulse in the atria, ventricles, and nodal and Purkinje systems (Quinidine, Procainamide).
USES
• Tachydysrhythmia: supraventricular tachycardia, paroxysmal atrial tachycardia, atrial fibrillation
CONTRAINDICATIONS
• Quinidine: AV block, bradycardia, cardiac failure, digitalis toxicity
SIDE EFFECTS
• Quinidine: cinchonism effects—tinnitus, headaches, nausea, vomiting, **dizziness**
• Hypotension, fatigue, **bradycardia**
• Amiodarone—†pulmonary toxicity,† visual impairment
NURSING IMPLICATIONS
1. *Monitor cardiac rhythm, particularly during initial dose for effectiveness; report apical pulse rate <60 beats/min.*
2. *Report dysrhythmias or hypotension.*
3. ‡Instruct patient to take all prescribed doses and not to catch up on missed doses.‡
4. ‡Instruct patient to report shortness of breath and irregular, fast, or slow heart beats.‡
Digitalis
ACTIONS
Affects the mechanical and electrical actions of the heart, which increase myocardial contractility and increase cardiac output. Alters the electrical activity in noncontractile tissue and ventricular muscle (e.g., automaticity, refractoriness, impulse conduction). Inhibits Na-K ATPase. Is classified as a cardiac glycoside.
USES
• Heart failure—to improve cardiac output
• Atrial fibrillation and flutter
CONTRAINDICATIONS AND PRECAUTIONS
• Hypersensitivity; ventricular tachycardia
SIDE EFFECTS
• Dizziness, headache, malaise, **fatigue**
• Muscle weakness, visual disturbances, **anorexia**
• **Hypokalemia** (most common reason for digoxin-related dysrhythmias is diuretic-induced hypokalemia), †dysrhythmias,† **bradycardia**
NURSING IMPLICATIONS
1. *Monitor digoxin serum levels; check for toxicity (2 ng/ml is considered toxic).*
2. *Monitor pulse,* and ‡teach patients to take their pulse.‡ *Report a pulse rate below 60 for adults and 100 for pediatric patients, hold the dose, and notify a primary health care provider.*
3. *Administer intravenous (IV) doses slowly over 5 minutes.*
4. *Do not double up with missed doses.*
5. ‡Teach patients to recognize early signs of hypokalemia (muscle weakness) and digitalis toxicity (nausea, vomiting, diarrhea, blurred or yellow visual disturbances), and notify a primary health care provider.‡
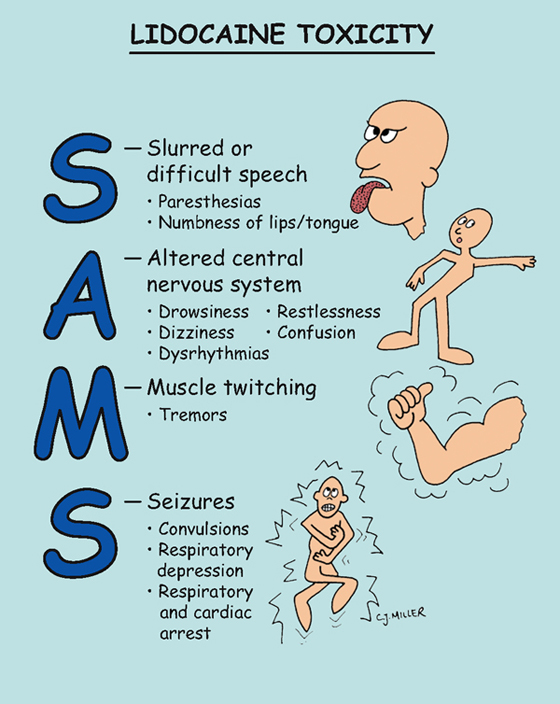
Lidocaine Toxicity
PATHOPHYSIOLOGY
Lidocaine is rapidly metabolized by the liver. If administered orally, the dose would be inactivated on the first pass through the liver. It is therefore given by intravenous (IV) infusion. Plasma drug levels are easily controlled. Its therapeutic range is 1.5 to 5.0 mcg/ml. In higher doses and at toxic levels, the central nervous and respiratory systems will be affected.
EFFECTS ON HEART AND ELECTROCARDIOGRAM (ECG)
• Blocks sodium channels and slows conduction
• Reduces automaticity in ventricles and bundle of His–Purkinje system
SIGNS AND SYMPTOMS OF TOXICITY
• **Drowsiness, confusion, paresthesias**
• Toxic doses—†seizure, heart block, cardiac and respiratory arrest†
TREATMENT
• Equipment for resuscitation (crash cart)
• Diazepam or phenytoin to be used for seizures
NURSING IMPLICATIONS
1. *Assess level of consciousness and orientation.*
2. Perform pulse checks, and assess for paresthesia.
3. *Protect for possible seizure activity.*
4. *Check vital signs frequently.*
5. *Monitor ECG, and report unusual activity.*
6. *Assess respiratory system, ventilation, and gas exchange (oxygen saturation).*
7. †Lidocaine preparations that contain epinephrine must never be administered intravenously (IV); doing so can cause severe hypertension and life-threatening dysrhythmias.† *Lidocaine used for local anesthesia often contains epinephrine.*
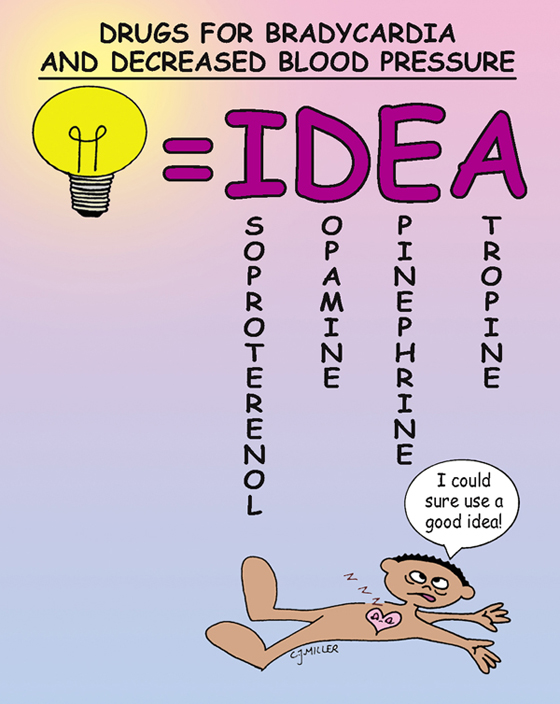
Drugs for Bradycardia and Decreased Blood Pressure
ISOPROTERENOL (ISUPREL)—Sympathomimetic, catecholamine
Actions
Increases heart rate and cardiac output, and causes bronchodilation.
Adverse Effects
**Tachycardia and angina;** can cause hyperglycemia in diabetics.
DOPAMINE—Sympathomimetic, catecholamine
Actions
At low doses, causes renal vasodilation. Moderate doses increase cardiac contractility, stroke volume, and cardiac output. Higher doses increase peripheral resistance, blood pressure, and renal vasoconstriction.
Adverse Effects
**Tachycardia,** †dysrhythmias,† anginal pain, †vasoconstriction leading to tissue necrosis with extravasation†
EPINEPHRINE (ADRENALIN)—Adrenergic agonist, catecholamine
Actions
Causes vasoconstriction, and increases heart rate; bronchodilator; is the treatment of choice for anaphylactic reactions.
Adverse Effects
**Hypertension,** †dysrhythmias,† **anginal pain, restlessness**
ATROPINE—Anticholinergic, antidysrhythmic
Actions
Acts on smooth muscle of the heart and increases cardiac rate.
Adverse Effects
**Tachycardia,** palpitations, **dry mouth, drowsiness, urinary hesitancy**
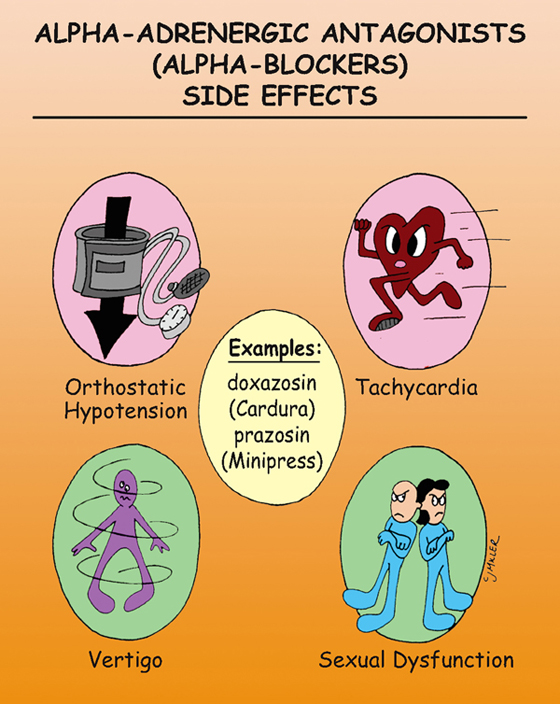
Alpha-Adrenergic Antagonists (Alpha-Blockers)
EXAMPLES
doxazosin (Cardura), prazosin (Minipress)
ACTIONS
Stimulate central alpha receptors, which decreases sympathetic outflow from the central nervous system, causing a decrease in peripheral vascular resistance and a slight decrease in cardiac output.
USES
• Mild-to-moderate hypertension
CONTRAINDICATIONS
• Hypersensitivity to drug and sulfites
PRECAUTIONS
• Patients with liver disease, blood dyscrasias, and pheochromocytoma
SIDE EFFECTS
• **Orthostatic hypotension,** tachycardia, **vertigo**
• Sexual dysfunction, nasal congestion, dry mouth
NURSING IMPLICATIONS
1. *Watch for orthostatic hypotension, which is intensified with prolonged standing, hot baths or showers, hot weather, alcohol use, and strenuous exercise.*
2. Patient should consume no more than four cups of caffeinated coffee, tea, or cola per day.
3. ‡Patient should take at bedtime to avoid drowsiness during the day.‡
4. *Discontinue slowly to avoid rebound hypertension.*
5. ‡Teach patient about first dose effect of severe orthostatic hypotension and to avoid hazardous activities and driving for 12 to 24 hours after initial dose. To decrease risk, instruct patient to take first dose at bedtime.‡
Beta-Blockers (Beta-Adrenergic Antagonists)
ACTIONS
Beta1 blockers (cardioselective) have a predominant effect on the heart by decreasing rate and contractility and decreasing velocity of impulse conduction at the atrioventricular (AV) node. Beta2 blockers (nonselective) have the same actions as beta1 blockers; however, they also affect the lungs, causing bronchoconstriction, and they block blood vessel receptors, causing vasoconstriction. Other beta blockers are vasodilating and may be cardioselective or nonselective.
EXAMPLES
• Beta1 (cardioselective)—metopropol (Lopressor, Toprol XL) used for angina and hypertension
• Vasodilating—nebivolol (Bystolic) cardioselective; carvedilol (Coreg) nonselective
CONTRAINDICATIONS
• Beta1 and beta2: bradycardia or cardiac block, hypotension
• Beta2: chronic obstructive pulmonary problems
PRECAUTIONS
• Diabetes—may interact with hypoglycemic agents; heart failure
SIDE EFFECTS
• Beta1: orthostatic hypotension, **bradycardia,** decreased libido, drowsiness
• Beta2: bronchoconstriction, **bronchospasm,** hypotension, **bradycardia,** dizziness, impotence
NURSING IMPLICATIONS
1. *Assess blood pressure and heart rate before and after initial dose.*
2. ‡Instruct patient regarding orthostatic hypotension.‡
3. *Delay the dose and notify the health care provider when the patient’s systolic blood pressure is less than 90 mm Hg or a significant decrease in pulse rate (bradycardia) occurs.*
4. *Medications are used with extreme caution in patients with heart failure; however, carvedilol (Coreg) may be used to treat heart failure.*
5. *Beta1 blockers may mask tachycardia, a primary sign of hypoglycemia.*
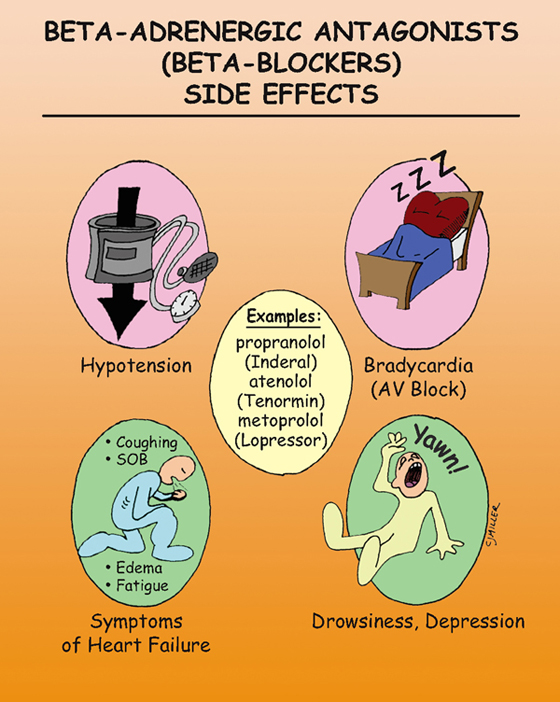
Beta-Adrenergic Antagonists (Beta-Blockers)
EXAMPLES
propranolol (Inderal), atenolol (Tenormin), metoprolol (Lopressor), nadolol (Corgard)
ACTIONS
Block sympathetic nervous system catecholamines, resulting in reduced renin and aldosterone release and fluid balance. Vasodilation of arterioles leads to a decrease in pulmonary vascular resistance and blood pressure.
USES
• Hypertension, antianginal agents in long-term treatment of angina
• Dysrhythmias—to suppress sinus and atrial tachydysrhythmias
CONTRAINDICATIONS
• Atrioventricular (AV) block, bradydysrhythmias
PRECAUTIONS
• Can cause bronchoconstriction; use with caution in patients with diabetes, cerebrovascular insufficiency, renal or hepatic dysfunction.
• History of depression, heart failure
SIDE EFFECTS
• Postural hypotension, †bradycardia,† **drowsiness,** depression, †symptoms of congestive heart failure†
• †Bronchospasm, bronchoconstriction,† malaise, **lethargy**
NURSING IMPLICATIONS
1. *Assess vital signs; monitor closely if given with a calcium channel blocker.*
2. ‡Report any weakness, dizziness, bradycardia, or fainting.‡
3. ‡Take medication before meals.‡
4. ‡Report any edema or difficulty breathing.‡
5. *Monitor patients with diabetes; tachycardia (a symptom of hypoglycemia) is often masked because of the beta1 blockade.*
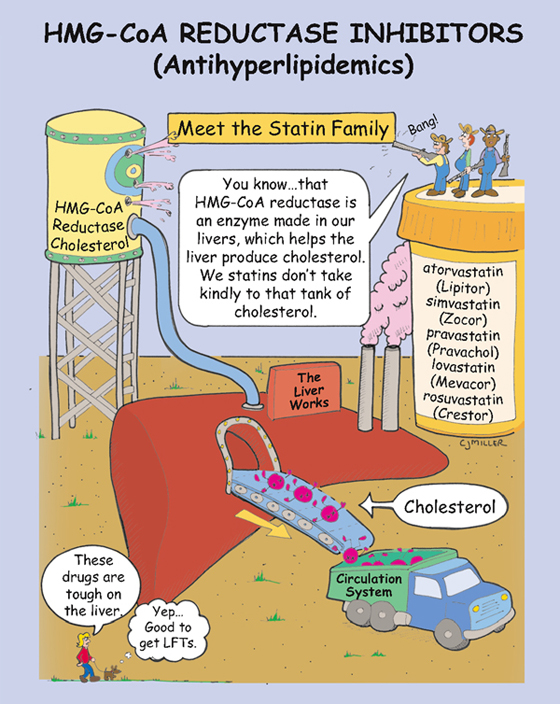
HMG-CoA Reductase Inhibitors (Statins)
EXAMPLES
atorvastatin (Lipitor), simvastatin (Zocor), pravastatin (Pravachol), lovastatin (Mevacor), rosuvastatin (Crestor)
ACTION
Lower cholesterol levels by inhibiting the formation of HMG-CoA reductase, which is an enzyme that is required for the liver to synthesize cholesterol.
USES
• Primary and secondary prevention of cardiovascular events
• Patients with type 2 diabetes and coronary heart disease
CONTRAINDICATIONS
PRECAUTIONS
SIDE EFFECTS
• Myopathy—rhabdomyolysis (severe form)
• Hepatotoxicity—liver injury with increases in serum transaminases
NURSING IMPLICATIONS
1. ‡Instruct patient to report unexplained muscle pain or tenderness.‡
2. *Monitor liver function studies.*
3. ‡Inform women of childbearing age about the potential for fetal harm should they become pregnant.‡
4. *Administer medication in the evening without regard to meals.*
5. ‡Instruct patient about dietary changes to reduce weight and cholesterol.‡