Procedure 39 Pollicization for Congenital Thumb Hypoplasia
Indications
 Hypoplastic thumb exists with inadequate carpometacarpal joint (Blauth types IIB, IV, and V).
Hypoplastic thumb exists with inadequate carpometacarpal joint (Blauth types IIB, IV, and V).
 Pollicization should be considered at about 12 to 18 months of age because at this age general anesthesia is safer and surgical dissection of critical structures is technically easier. In addition, this allows for preliminary correction of any associated radial deficiencies.
Pollicization should be considered at about 12 to 18 months of age because at this age general anesthesia is safer and surgical dissection of critical structures is technically easier. In addition, this allows for preliminary correction of any associated radial deficiencies.
Examination/Imaging
Clinical Examination
 The Blauth classification of thumb hypoplasia is useful in determining treatment options. Types IV (floating thumb) (Fig. 39-1) and V (absent thumb) (Fig. 39-2) are straightforward to identify clinically. However, it can be challenging to differentiate type IIIA (stable carpometacarpal [CMC] joint) from type IIIB (unstable CMC joint), and the trapezium and trapezoid are ossified only at 5 to 6 years of age, making radiographs less useful in decision making.
The Blauth classification of thumb hypoplasia is useful in determining treatment options. Types IV (floating thumb) (Fig. 39-1) and V (absent thumb) (Fig. 39-2) are straightforward to identify clinically. However, it can be challenging to differentiate type IIIA (stable carpometacarpal [CMC] joint) from type IIIB (unstable CMC joint), and the trapezium and trapezoid are ossified only at 5 to 6 years of age, making radiographs less useful in decision making.
 Serial examination of a child is required to differentiate between types IIIA and IIIB. A newborn uses digital grasp, and the infant begins to use the thumb in grasp at about 1 year of age. If the child uses the thumb in manipulating objects, this suggests that a type IIIA deficiency is present. If the child prefers to grasp objects between the index and long finger web space, this web appears wider, and the index finger is pronated toward the thumb. This suggests type IIIB hypoplasia.
Serial examination of a child is required to differentiate between types IIIA and IIIB. A newborn uses digital grasp, and the infant begins to use the thumb in grasp at about 1 year of age. If the child uses the thumb in manipulating objects, this suggests that a type IIIA deficiency is present. If the child prefers to grasp objects between the index and long finger web space, this web appears wider, and the index finger is pronated toward the thumb. This suggests type IIIB hypoplasia.
 The index finger may be stiff and hypoplastic to varying degrees in children with type IV and type V hypoplasia, which will affect the result of pollicization.
The index finger may be stiff and hypoplastic to varying degrees in children with type IV and type V hypoplasia, which will affect the result of pollicization.
 The child should be examined for signs of other systematic abnormalities, such as VACTERL (i.e., vertebral abnormalities, anal atresia, cardiac abnormalities, tracheoesophageal fistula and/or esophageal atresia, renal agenesis and dysplasia, and limb defects), Fanconi anemia, and Holt-Oltram syndrome, before considering surgical reconstruction.
The child should be examined for signs of other systematic abnormalities, such as VACTERL (i.e., vertebral abnormalities, anal atresia, cardiac abnormalities, tracheoesophageal fistula and/or esophageal atresia, renal agenesis and dysplasia, and limb defects), Fanconi anemia, and Holt-Oltram syndrome, before considering surgical reconstruction.
Imaging
 Radiographs of the hands, wrists, and forearms are useful in determining the degree of metacarpal and phalangeal hypoplasia of the thumb and index finger. They can also identify other associated upper extremity anomalies, such as radial deficiency.
Radiographs of the hands, wrists, and forearms are useful in determining the degree of metacarpal and phalangeal hypoplasia of the thumb and index finger. They can also identify other associated upper extremity anomalies, such as radial deficiency.
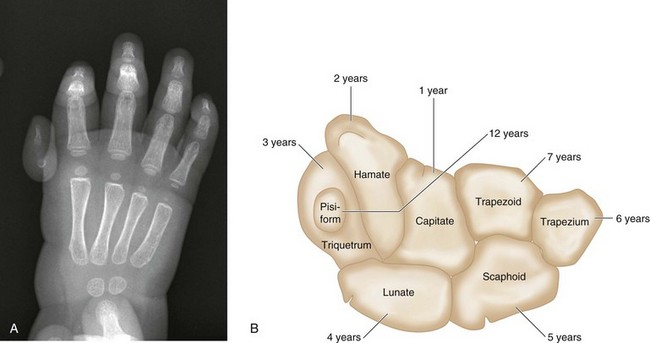
 The number of carpal bones seen on the radiograph gives a rough estimate of the age of the child (Fig. 39-3A). The order of ossification of carpal bones is detailed in Figure 39-3B. About one center appears per year from the age of 1 year to 7 years.
The number of carpal bones seen on the radiograph gives a rough estimate of the age of the child (Fig. 39-3A). The order of ossification of carpal bones is detailed in Figure 39-3B. About one center appears per year from the age of 1 year to 7 years.
 The presence of a tapered metacarpal without a base confirms type IIIB hypoplasia. Type IIIA hypoplasia is associated with full length of the metacarpal (Fig. 39-4).
The presence of a tapered metacarpal without a base confirms type IIIB hypoplasia. Type IIIA hypoplasia is associated with full length of the metacarpal (Fig. 39-4).
Surgical Anatomy
 After pollicization, the common digital artery to the index and long fingers is the primary blood supply to the transposed digit. The radial digital artery to the index finger may be absent, but the ability to perform index pollicization is not contingent on the presence of the radial digital artery when the main blood supply comes from the ulnar digital artery.
After pollicization, the common digital artery to the index and long fingers is the primary blood supply to the transposed digit. The radial digital artery to the index finger may be absent, but the ability to perform index pollicization is not contingent on the presence of the radial digital artery when the main blood supply comes from the ulnar digital artery.
Positioning
 The procedure is conducted under general anesthesia with the patient placed supine on the operating room table. The entire upper extremity is prepared and draped after a tourniquet is applied.
The procedure is conducted under general anesthesia with the patient placed supine on the operating room table. The entire upper extremity is prepared and draped after a tourniquet is applied.
 The limb is exsanguinated fully to permit a completely bloodless field. A well-fitted, small tourniquet is essential because blood in the operative field will jeopardize the operation by obscuring the small structures in the pediatric hand.
The limb is exsanguinated fully to permit a completely bloodless field. A well-fitted, small tourniquet is essential because blood in the operative field will jeopardize the operation by obscuring the small structures in the pediatric hand.
Exposures
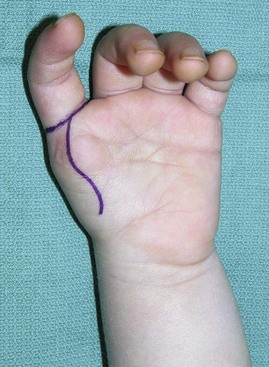
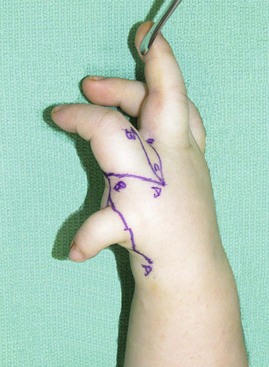
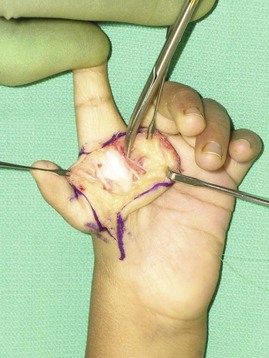
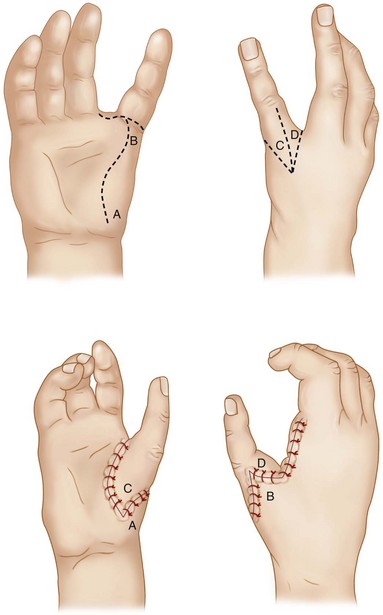
 A longitudinal curvilinear incision is marked over the palmar aspect of the index finger metacarpal (Fig. 39-5). A V-shaped incision is marked over the dorsum of the index finger metacarpal such that the apex is at the level of the neck of the metacarpal (Figs. 39-6 and 39-7). The dorsal and palmar incisions are connected at the base of the finger. A longitudinal incision is marked over the dorsum of the proximal phalanx, extending from the proximal interphalangeal (PIP) joint to the apex of the V.
A longitudinal curvilinear incision is marked over the palmar aspect of the index finger metacarpal (Fig. 39-5). A V-shaped incision is marked over the dorsum of the index finger metacarpal such that the apex is at the level of the neck of the metacarpal (Figs. 39-6 and 39-7). The dorsal and palmar incisions are connected at the base of the finger. A longitudinal incision is marked over the dorsum of the proximal phalanx, extending from the proximal interphalangeal (PIP) joint to the apex of the V.
Procedure
Step 1
 The palmar skin incisions are made first, and thick skin flaps are raised.
The palmar skin incisions are made first, and thick skin flaps are raised.
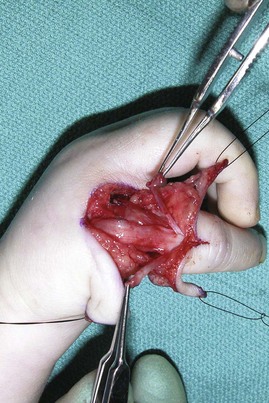
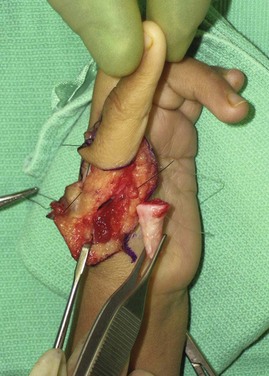
 The radial neurovascular bundle along the index finger is identified and isolated (Fig. 39-10). The common digital artery to the second web space is then identified. The dissection continues distally to isolate the ulnar digital artery to the index finger and the radial digital artery to the middle finger (Fig. 39-11).
The radial neurovascular bundle along the index finger is identified and isolated (Fig. 39-10). The common digital artery to the second web space is then identified. The dissection continues distally to isolate the ulnar digital artery to the index finger and the radial digital artery to the middle finger (Fig. 39-11).
 The radial digital artery to the long finger is ligated using 6-0 Prolene suture distal to the bifurcation. Dissection of these fine structures will require use of a microscope or loupes with 3.5× or greater magnification. This will allow mobilization of the index finger based on the radial digital artery and the common digital artery. The vessels are mobilized proximally to the level of the superficial arch.
The radial digital artery to the long finger is ligated using 6-0 Prolene suture distal to the bifurcation. Dissection of these fine structures will require use of a microscope or loupes with 3.5× or greater magnification. This will allow mobilization of the index finger based on the radial digital artery and the common digital artery. The vessels are mobilized proximally to the level of the superficial arch.
 Intraneural dissection of the common digital nerve is done to separate the fibers of the ulnar digital nerve to the index finger from the fibers of the radial digital nerve to the middle finger. This dissection is carried proximally to the superficial arch as well.
Intraneural dissection of the common digital nerve is done to separate the fibers of the ulnar digital nerve to the index finger from the fibers of the radial digital nerve to the middle finger. This dissection is carried proximally to the superficial arch as well.
Step 2
Step 3
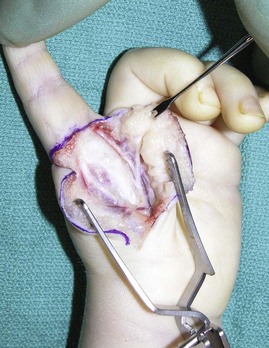
 The dorsal skin incisions are made, and flaps are raised. It is important to raise thin flaps, identify the dorsal veins, and protect them (Fig. 39-14).
The dorsal skin incisions are made, and flaps are raised. It is important to raise thin flaps, identify the dorsal veins, and protect them (Fig. 39-14).
 The juncturae tendineae between the index and long finger extensor tendons are divided.
The juncturae tendineae between the index and long finger extensor tendons are divided.
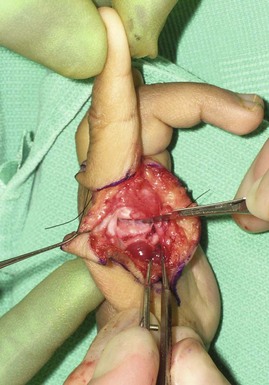
 The first dorsal and palmar interossei are elevated off the radial and ulnar aspects of the metacarpal shaft, respectively. Only the proximal portion of these muscles originating from the base of the metacarpal is left intact. The tendons of these two muscles are carefully separated from the metacarpophalangeal (MCP) joint capsule and divided distally along with a small portion of the extensor hood (Fig. 39-15).
The first dorsal and palmar interossei are elevated off the radial and ulnar aspects of the metacarpal shaft, respectively. Only the proximal portion of these muscles originating from the base of the metacarpal is left intact. The tendons of these two muscles are carefully separated from the metacarpophalangeal (MCP) joint capsule and divided distally along with a small portion of the extensor hood (Fig. 39-15).
Step 4
 The skin flaps over the proximal phalanx are raised, and the extensor hood is identified (Fig. 39-16). The radial and ulnar lateral bands are identified on either side of midproximal phalanx.
The skin flaps over the proximal phalanx are raised, and the extensor hood is identified (Fig. 39-16). The radial and ulnar lateral bands are identified on either side of midproximal phalanx.
Step 5
 The index finger metacarpal shaft is shortened by performing two osteotomies.
The index finger metacarpal shaft is shortened by performing two osteotomies.
 The distal osteotomy is done beyond the neck of the metacarpal through the physis (Fig. 39-17 and 39-18). The physis is soft, and a blade can be used for this osteotomy.
The distal osteotomy is done beyond the neck of the metacarpal through the physis (Fig. 39-17 and 39-18). The physis is soft, and a blade can be used for this osteotomy.
 The proximal osteotomy is done at the base of the metacarpal using a bone cutter (Fig. 39-19).
The proximal osteotomy is done at the base of the metacarpal using a bone cutter (Fig. 39-19).
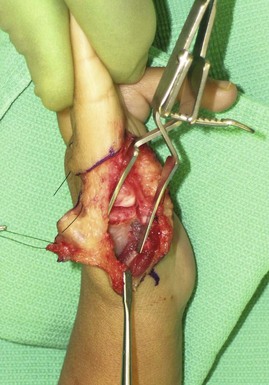
 The index finger is now freely mobile and attached only by the dorsal veins, radial and ulnar neurovascular bundles, and flexor and extensor tendons (Fig. 39-20).
The index finger is now freely mobile and attached only by the dorsal veins, radial and ulnar neurovascular bundles, and flexor and extensor tendons (Fig. 39-20).
Step 5 Pearls
The tip of the pollicized index finger should reach the PIP joint of the middle finger to achieve optimal length. However, it is more common for a pollicized finger to be too long rather than too short. Although the metacarpal shaft is removed, the insertion of the flexor carpi radialis and extensor carpi radialis longus proximally and the origin of the collateral ligaments distally must be spared.
Step 6
 At this point, the index finger is positioned over the base of the index metacarpal. The index MCP joint will now function as the new thumb CMC joint. It is positioned in about 45 degrees of abduction and 100 to 120 degrees of pronation to recreate the position of the thumb. The position should be such that the pulp of the index finger is in contact with the radial aspect of the PIP joint and the proximal phalanx of the middle finger (Fig. 39-21).
At this point, the index finger is positioned over the base of the index metacarpal. The index MCP joint will now function as the new thumb CMC joint. It is positioned in about 45 degrees of abduction and 100 to 120 degrees of pronation to recreate the position of the thumb. The position should be such that the pulp of the index finger is in contact with the radial aspect of the PIP joint and the proximal phalanx of the middle finger (Fig. 39-21).
Step 6 Pearls
The normal index finger MCP joint can hyperextend to 20 to 30 degrees beyond neutral. However, this hyperextension is not desirable at the new thumb CMC joint. To prevent further hyperextension, the MCP joint is held in maximal hyperextension, and the dorsal capsule is sutured to the physis with 4-0 nonabsorbable suture to maintain this position.
The index finger metacarpal should be positioned at 45 degrees of abduction relative to the base. An oblique osteotomy of the metacarpal base can be created to improve the position of the thumb.
Step 7
Step 8
 The first dorsal interosseus tendon is attached to the radial lateral band at the level of midproximal phalanx to provide abduction of the pollicized index finger. The first palmar interosseus tendon is attached to the ulnar lateral band and functions as the thumb adductor.
The first dorsal interosseus tendon is attached to the radial lateral band at the level of midproximal phalanx to provide abduction of the pollicized index finger. The first palmar interosseus tendon is attached to the ulnar lateral band and functions as the thumb adductor.
 The extensor and flexor tendons are left attached and will shorten over time. The new anatomic functions of the index finger joints and muscle units are detailed in Table 39-1. The extensor digitorum communis will function as the abductor pollicis longus. The extensor indicis proprius will act as the extensor pollicis longus. The first palmar interosseus will function as the adductor pollicis, and the first dorsal interosseus will function as the abductor pollicis. The index finger distal interphalangeal joint will become the interphalangeal joint; the PIP joint will become the metaphalangeal (MP) joint, and the index finger MP joint will become the pollicized digit CMC joint.
The extensor and flexor tendons are left attached and will shorten over time. The new anatomic functions of the index finger joints and muscle units are detailed in Table 39-1. The extensor digitorum communis will function as the abductor pollicis longus. The extensor indicis proprius will act as the extensor pollicis longus. The first palmar interosseus will function as the adductor pollicis, and the first dorsal interosseus will function as the abductor pollicis. The index finger distal interphalangeal joint will become the interphalangeal joint; the PIP joint will become the metaphalangeal (MP) joint, and the index finger MP joint will become the pollicized digit CMC joint.
| Unit | New Function |
|---|---|
| Skeletal Units | |
| Distal interphalangeal joint | Interphalangeal joint |
| Proximal interphalangeal joint | Metacarpophalangeal joint |
| Metacarpophalangeal joint | Carpometacarpal joint |
| Musculotendinous Units | |
| Extensor indicis proprius | Extensor pollicis longus |
| Extensor digitorum communis (index) | Abductor pollicis longus |
| First palmar interosseous | Adductor pollicis |
| First dorsal interosseus | Abductor pollicis brevis |
Step 9
 The skin flaps are transposed into position and held with a few tagging 4-0 chromic catgut sutures (Figs. 39-22 and 39-23).
The skin flaps are transposed into position and held with a few tagging 4-0 chromic catgut sutures (Figs. 39-22 and 39-23).
 Figure 39-24 illustrates the movement of the different flaps.
Figure 39-24 illustrates the movement of the different flaps.
Step 10
 The tourniquet is released, and the pollicized digit is inspected for capillary refill and any evidence of vascular compromise. Meticulous hemostasis is secured. The skin flaps are sutured using 4-0 chromic catgut (Figs. 39-25 and 39-26).
The tourniquet is released, and the pollicized digit is inspected for capillary refill and any evidence of vascular compromise. Meticulous hemostasis is secured. The skin flaps are sutured using 4-0 chromic catgut (Figs. 39-25 and 39-26).
Step 10 Pitfalls
The pollicized finger may appear pale after closure, which is usually due to vasospasm and is alleviated with warm soaks. If the perfusion does not improve within 15 to 20 minutes, any constricting closing sutures can be removed and the residual raw area skin grafted. However, persistent failure of perfusion demands exploration of the digital vessels.
Postoperative Care and Expected Outcomes
 A long-arm thumb spica cast is applied with the elbow in flexion, and the arm is kept elevated to promote venous drainage.
A long-arm thumb spica cast is applied with the elbow in flexion, and the arm is kept elevated to promote venous drainage.
 The cast is removed 4 weeks postoperatively, and therapy is initiated to focus on thumb mobility, pinch, and grasp. The patient is transitioned to a short-arm thumb spica splint for protection and stability during this period.
The cast is removed 4 weeks postoperatively, and therapy is initiated to focus on thumb mobility, pinch, and grasp. The patient is transitioned to a short-arm thumb spica splint for protection and stability during this period.
 In general, outcomes following pollicization are directly related to the mobility of the index finger, and pollicization achieves about 30% of grip and pinch strength compared with the contralateral thumb. Figures 39-27 through 39-29 show the postoperative result at 1 year follow-up for the child shown in Figures 39-8 and 39-9.
In general, outcomes following pollicization are directly related to the mobility of the index finger, and pollicization achieves about 30% of grip and pinch strength compared with the contralateral thumb. Figures 39-27 through 39-29 show the postoperative result at 1 year follow-up for the child shown in Figures 39-8 and 39-9.
Aliu O, Netscher DT, Staines KG, et al. A 5-year interval evaluation of function after pollicization for congenital thumb aplasia using multiple outcome measures. Plast Reconstr Surg. 2008;122:198-205.
Buck-Gramcko D. Pollicization of the index finger: methods and results in aplasia and hypoplasia of the thumb. J Bone Joint Surg [Am]. 1971;53:1605-1617.
Manske PR, McCarroll HR. Index finger pollicization for a congenitally absent or nonfunctioning thumb. J Hand Surg [Am]. 1985;10:606-613.