CASE 39 PCI Versus Medical Therapy for Stable Angina
Case presentation
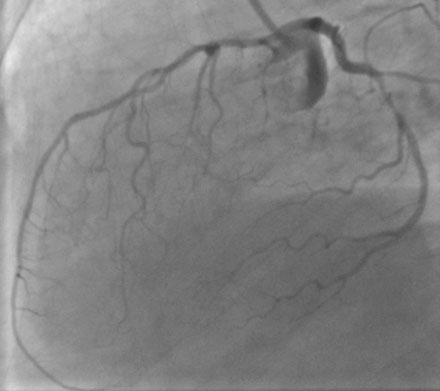
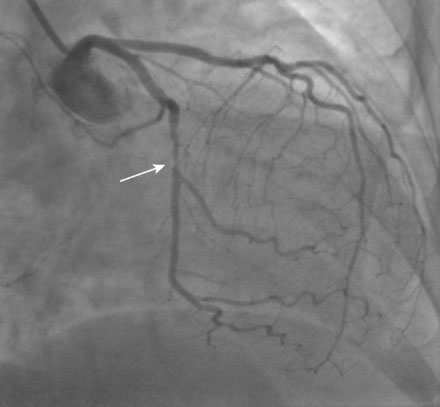
A 73-year-old woman with a past medical history of poorly controlled hypertension, hyperlipidemia, hypothyroidism, and gastroesophageal reflux disease and a family history of coronary artery disease presented with exertional chest and arm discomfort and shortness of breath. She underwent an exercise stress thallium test during which she exercised 6 minutes in a standard Bruce protocol, achieved 73% of her age-predicted heart rate, and reached a maximum blood pressure of 200/90 mmHg. The test was terminated secondary to fatigue. Nuclear imaging revealed no convincing evidence of ischemia. Due to continued symptoms, she underwent cardiac catheterization. The right coronary artery was dominant, with minimal disease (Figure 39-1). The left coronary showed minimal disease of the left anterior descending artery and a severe stenosis in the mid-circumflex artery (Figures 39-2, 39-3 and Video 39-1). After her physician discussed the risks and benefits of percutaneous intervention versus optimal medical therapy, she chose medical management. Her medical regimen was maximized and included an angiotensin-receptor blocker, a calcium-channel blocker, aspirin, a beta-blocker, long-acting nitrates, and a statin. However, despite this therapy, she continued to experience exertional chest pressure and shortness of breath that significantly limited her physical activity. Thus, 3 months later she decided to pursue percutaneous intervention of the circumflex artery.
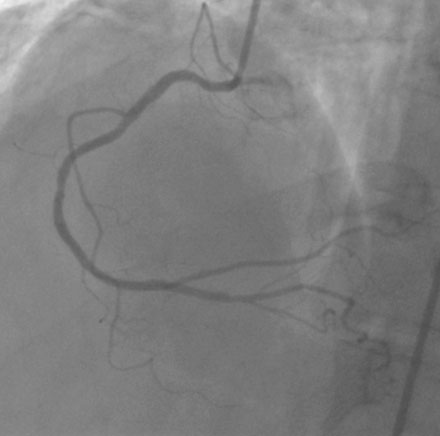
FIGURE 39-1 Right coronary angiogram, demonstrating a dominant right coronary artery with minimal disease.
Cardiac catheterization
The lesion appeared unchanged by angiography. Anticoagulation was achieved with a bolus and infusion of bivalirudin. A 0.014 inch floppy-tipped guidewire was advanced into the circumflex artery beyond the lesion. The lesion was successfully predilated with a 2.0 mm diameter by 20 mm long compliant balloon. A 2.5 mm diameter by 24 mm long drug-eluting stent was then deployed (Figure 39-4 and Video 39-2). Hemostasis was achieved with a vascular closure device and she was discharged the next morning after an uncomplicated overnight stay.
Discussion
In the United States, over 1 million coronary interventions are performed annually. The majority of percutaneous coronary interventions (PCI) are performed electively in patients with stable coronary artery disease, with only about 15% being performed in the setting of an acute coronary syndrome.1,2 It has been clearly demonstrated that PCI in the setting of an acute coronary syndrome can provide benefit in terms of death and myocardial infarction.3,4 This same benefit, however, does not appear to be present when PCI is performed for stable coronary disease.5,6 Until recently, however, little was known about the benefits of PCI for stable syndromes in patients receiving optimal medical therapy. The COURAGE trial is the largest and most recent trial investigating whether PCI in addition to optimal medical therapy can reduce cardiovascular events compared to optimal medical therapy alone in this lower-risk population. Similar to previous trials, the addition of PCI added no benefit in terms of death, myocardial infarction, or stroke over an average follow-up of 4.6 years. However, similar to the case shown here, there was significant crossover of the medical therapy group to PCI because of ongoing symptoms despite medical therapy; in addition, the PCI group demonstrated a greater freedom from angina throughout most of the follow-up period.7
Current ACC/AHA guidelines recommend an initial approach of optimal medical therapy, lifestyle intervention, and risk factor reduction in the population with stable coronary artery disease. PCI is advocated only with failure of this strategy.8,9 Much debate, however, still exists as to the proper management of this population. Argument can certainly be made for both strategies. Initial medical therapy mitigates the risk of a potentially unnecessary procedure. However, for many medically treated patients, symptoms may not improve significantly, or, they may note significant side effects from the medications, including fatigue from beta blockers or headaches from long-acting nitrates. In patients with ongoing angina, lifestyle strategies such as exercise, may be difficult, if not impossible to achieve. Further, clinical depression may coexist in patients who are significantly limited in daily activities. A strategy of initial PCI may return patients to routine activities and work more quickly than medical therapy alone. Therefore, while PCI provides no benefit in terms of death or myocardial infarction in a stable population, a better understanding of the psychosocial outcomes of the two strategies is needed.
1 Lloyd-Jones D., Adams R., Carnethon M., et al. Heart disease and stroke statistics – 2009 update. A report from the American Heart Association Statistics Committee and Stroke Statistics Committee. Circulation. 2009;119:e1-e161.
2 Feldman D.N., Gade C.L., Slotwiner A.J., et al. Comparison of outcomes of percutaneous coronary interventions in patients of three age groups. Am J Cardiol. 2006;98:1334-1339.
3 Keeley E.C., Boura J.A., Grines C.L. Primary angioplasty versus intravenous thrombolytic therapy for acute myocardial infarction: a quantitative review of 23 randomized trials. Lancet. 2003;361:13-20.
4 Mehta S.R., Cannon C.P., Fox K.A., et al. Routine versus selective invasive strategies in patients with acute coronary syndromes: a collaborative meta-analysis of randomized trials. J Am Med Assoc. 2005;293:2908-2917.
5 Pitt B., Waters D., Brown W.V., et al. Aggressive lipid lowering therapy compared with angioplasty in stable coronary artery disease. N Engl J Med. 1999;341:70-76.
6 Henderson R.A., Pocock S.J., Clayton T.C., et al. Seven-year outcomes in the RITA-2 trial: coronary angioplasty versus medical therapy. J Am Coll Cardiol. 2003;42:1161-1170.
7 Boden W.E., O’Rourke R.A., Teo K.K., et al. Optimal medical therapy with or without PCI for stable coronary disease. N Engl J Med. 2007;356:1-14.
8 Smith S.C.Jr, Feldman T.E., Hirshfeld J.W.Jr, et al. ACC/AHA/SCAI 2005 guideline update for percutaneous coronary intervention. Circulation. 2006;113:156-175.
9 King S.B., Smith S.C., Hirshfeld J.W., et al. 2007 Focused Update of the ACC/AHA/SCAI 2005 guideline update for percutaneous coronary intervention. Circulation. 2008;117:261-295.