CASE 39
History: A 20-year-old man presents with a rectal discharge.
1. Which of the following should be included in the differential diagnosis of the imaging finding shown? (Choose all that apply.)
A. Familial adenomatous polyposis
2. Which polyposis syndrome is associated with osteomas and cortical hyperostosis?
A. Familial adenomatous polyposis
3. Several of the colonic polyposis syndromes have an autosomal dominant pattern of inheritance. Which of the following is the exception?
A. Familial adenomatous polyposis
4. The patient imaged also has a rash, alopecia, and diarrhea. What is the likely diagnosis?
A. Familial adenomatous polyposis (FAP)
ANSWERS
CASE 39
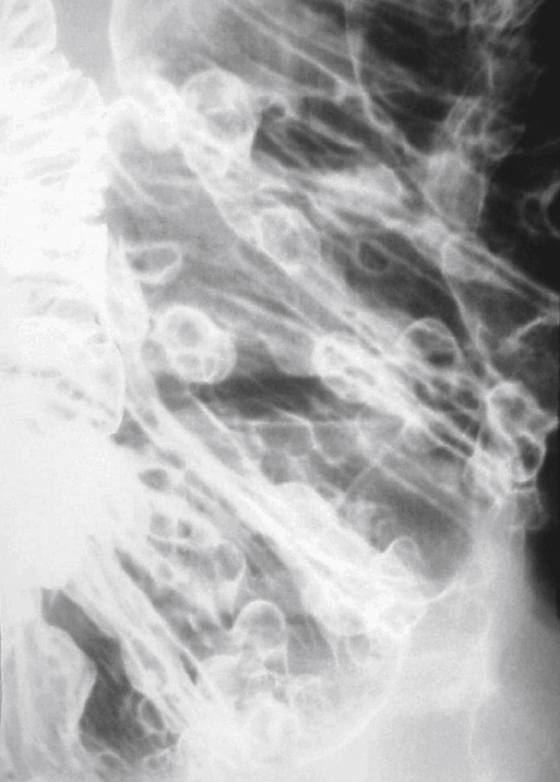
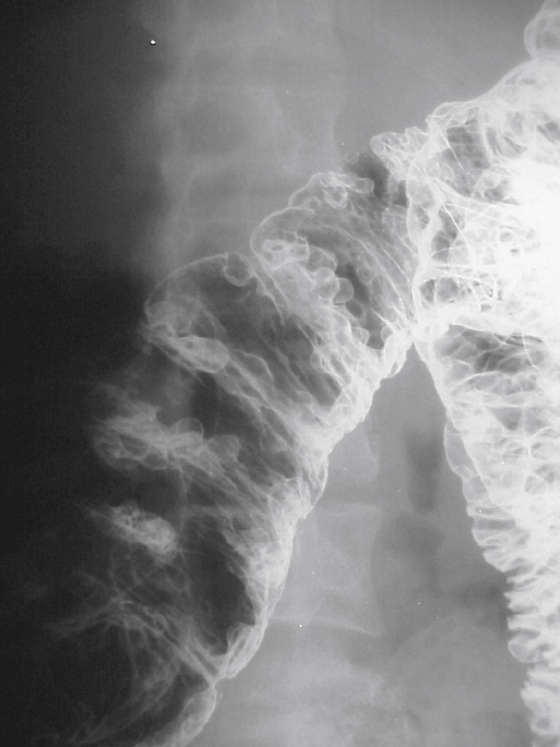
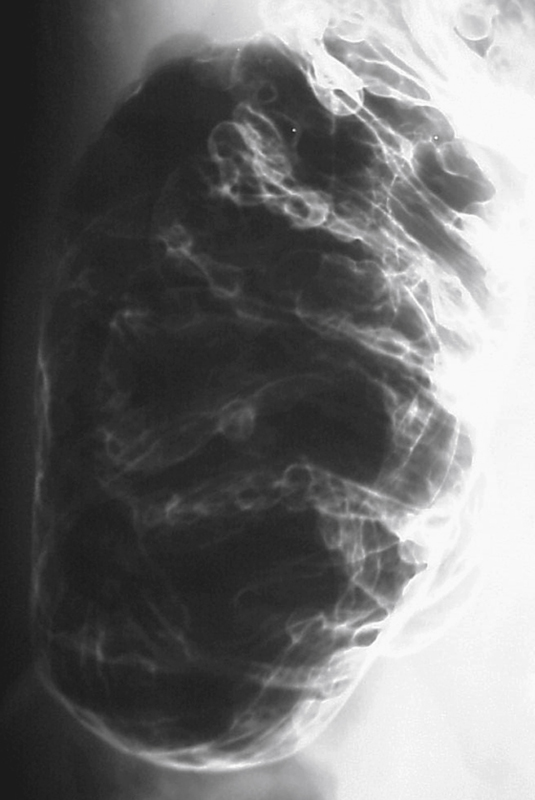
Colonic Polyposis
1. A, B, C, and D
2. A
3. B
4. B
Reference
Buck JL, Harned RK. Polyposis syndromes. In: Gore RM, Levine MS, eds. Textbook of Gastrointestinal Radiology. 2nd ed Philadelphia: WB Saunders; 2000:1075–1088.
Cross-Reference
Gastrointestinal Imaging: THE REQUISITES, 3rd ed, p 284.
Comment
Innumerable adenomatous polyps of the colon, particularly in a young adult, usually indicate a polyposis syndrome. For years, these adenomatous polypoid conditions were classified as familial polyposis coli or (when fewer polyps) Gardner’s syndrome. Patients with Gardner’s syndrome were believed to develop the extracolonic manifestations. These conditions are inherited as autosomal dominant traits and cause the formation of numerous adenomatous colonic polyps. Many now believe that these two conditions represent variable penetrance of the same genetic defect and classify these entities as familial adenomatous polyposis syndrome (FAPS).
In patients with FAPS, polyps are seen primarily in the colon but can occur outside the colon, usually in the stomach or small bowel. There is also an associated increase of nonadenomatous polyps present in both colon and stomach. These growths usually are hyperplastic polyps or so-called fundic gland polyps. Adenomas also occur with slightly increased incidence in the stomach and duodenum, and there is an increased incidence of periampullary carcinoma (the second most common malignancy after colon carcinoma) among these patients. In some studies the incidence of small bowel adenomas has been notably increased.
Extraintestinal manifestations include bone abnormalities. Osteomas, although classically associated with Gardner’s syndrome, occur in up to 50% of patients. There also is an increased incidence of cortical hyperostosis and dental abnormalities associated with FAPS. Epidermal cysts have been described, as have pigmented lesions of the retina. The incidence of thyroid carcinoma also is believed to be increased, particularly in women. Large intra-abdominal fibrous tumors, mesenteric fibromatosis, and desmoid tumors occur sporadically. Some believe that there is a slight increase in the incidence of pancreatic carcinoma and benign liver tumors. Tumors of the central nervous system (glioblastomas and medulloblastomas) are generally associated with Turcot’s syndrome, but many claim that Turcot’s is just another, more deadly, variation of FAPS.