CHAPTER 38
Ulnar Collateral Ligament Sprain
Definition
The ulnar collateral ligament (UCL) complex includes the ulnar proper collateral ligament and the ulnar accessory collateral ligament [1]. These ligaments are located deep to the adductor aponeurosis of the thumb and stabilize the first metacarpophalangeal (MCP) joint. Tears can occur if a valgus force is applied to an abducted first MCP joint [2]. A lesion of the UCL is commonly called skier’s thumb.
Acute injuries can occur when the strap on a ski pole forcibly abducts the thumb. In the United States, estimates for skiing injuries are 3 or 4 per 1000 skier-hours; thumb injuries account for about 10% of skiing injuries [3]. A study of downhill skiing found that thumb injuries accounted for 17% of skiing injuries, second only to knee injuries [4]. Three fourths of the thumb injuries were UCL sprains. UCL injury in football players may be related to falls or blocking. Other sports involving ball handling or equipment with repetitive abduction forces to the thumb, like basketball or lacrosse, can cause injury to the UCL.
UCL injuries may be accompanied by avulsion fractures. Complete tears can fold back proximally when they are ruptured distally and become interposed between the adductor aponeurosis [1]. This injury is known as the Stener lesion and has been described as a complication of complete UCL tears, with a frequency ranging from 33% to 80% [5].
Chronic ligamentous laxity is more common in occupational conditions associated with repetitive stresses to the thumb. The term gamekeeper’s thumb was coined in the mid-1950s to describe an occupational injury of Scottish gamekeepers [6]. The term is also used for acute injuries to the UCL.
Rupture of the thumb MCP joint UCL represents one of the most common ligamentous injuries of the hand. Failure to recognize these injuries or to treat them appropriately can lead to instability, pain, and weakness of the joint [7].
Symptoms
Patients report pain and instability of the thumb joint. In the acute injury setting, patients can often recall the instant of injury. If the UCL is ruptured, patients report swelling and hematoma formation; pain may be minimal with complete tears. When pain is present, it can cause thumb weakness and reduced function. Numbness and paresthesias are not typical findings.
Physical Examination
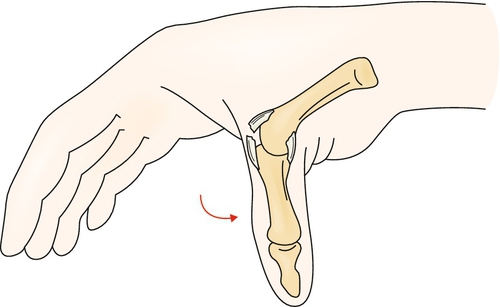
The physical examination begins with the uninvolved thumb, noting the individual’s normal range of motion and stability. Palpate to determine the point of maximal tenderness, assessing for distal tenderness; if the ligament is torn, it tears distally off the proximal phalanx. Initially, the examiner may be able to detect a knot at the site of ligament disruption. Laxity of the UCL is the key finding on examination. Ligament injuries are graded as follows: grade I sprains, local injury without loss of integrity; grade II sprains, local injury with partial loss of integrity, but end-feel is present; and grade III sprains, complete tear with loss of integrity and end-feel (Fig. 38.1). Passive abduction can be painful, especially in acute grade I and grade II sprains.
The UCL should be tested with the first MCP joint in extension and flexion to evaluate all bands. The excursion is compared with the uninjured side. Testing for disruption of the ulnar proper collateral ligament is done with the thumb flexed to 90 degrees [1]. With the thumb in extension, a false-negative finding may result. The stability of the joint will not be impaired even if the ulnar proper collateral ligament is torn because of the taut ulnar accessory ligament in extension.
To avoid a false interpretation, the examiner must prevent MCP rotation by grasping the thumb proximal to the joint. If there is more than 30 degrees of laxity (or 15 degrees more laxity than on the noninjured side), rupture of the proper collateral ligament is likely. The thumb is then positioned in extension for repeated valgus stress testing. If valgus laxity is less than 30 degrees (or 15 degrees less than on the noninjured side), the accessory collateral ligament is intact. If valgus laxity is greater than 30 degrees (or 15 degrees more than on the noninjured side), the accessory collateral ligament is also ruptured [8].
A displaced fracture is a contraindication to stress testing. The fracture is manifested with swelling or discoloration on the ulnar side of the first MCP joint and tenderness along the base of the proximal phalanx. Some authors recommend that conventional radiographs be obtained before stressing of the UCL to determine whether a large undisplaced fracture is present because stress testing could cause displacement [9]. More than 3 mm of volar subluxation of the proximal phalanx indicates gross instability. The patient may be unable to pinch. Pain may limit the complete examination and lead to underestimation of injury extent. Infiltration of local anesthetic around the injury site can reduce discomfort and improve the accuracy of the examination [10].
Avulsion fracture represents a special class of collateral ligament injury. It cannot be graded I to III because technically the ligament is not torn. However, it still deserves mention because fracture can compromise the bone-ligament-bone stabilization complex and lead to chronic symptoms [11].
Functional Limitations
Individuals describe difficulty with pinching activities (e.g., turning a key in a lock). Injuries affecting the dominant hand can have an impact on many fine motor manipulations, such as buttoning or retrieving objects from one’s pocket. Injuries affecting the nondominant hand can impair bilateral hand activities requiring stabilization of small objects. Sports performance can be reduced with dominant hand injuries, and skiing, ball handling, or equipment use may be contraindicated in the acute stage of injury or on the basis of the extent of injury. In the setting of high-level or professional sports competition, the clinical decision to allow an athlete to compete with appropriate splinting or casting is based on severity of symptoms, with the caveat that the potential for worsening of the injury exists.
Diagnostic Studies
Whereas clinical examination is the mainstay of diagnosis, imaging studies are useful in the setting of uncertain diagnosis [12]. A plain radiograph is essential to rule out an avulsion fracture of the base of the ulnar side of the proximal phalanx. A stress film with the thumb in abduction is occasionally useful and should be compared with the uninjured side. UCL rupture presents with an angle greater than 35 degrees. Magnetic resonance imaging has greater than 90% sensitivity and specificity for UCL tears but is expensive and not always required [13].
Ultrasonography has been used as a less expensive means for diagnosis of UCL tears, but controversy exists as to whether it is useful or fraught with pitfalls [12,14–16]. However, a retrospective review of ultrasound studies from 17 surgically proven displaced full-thickness UCL tears identified the following ultrasound criteria for 100% accuracy in the diagnosis of a displaced full-thickness UCL tear: lack of UCL fibers and presence of a heterogeneous mass-like abnormality proximal to the MCP joint of the thumb. Such displaced UCL tears were most often located proximal to the leading edge of the adductor aponeurosis rather than superficially. Standardized ultrasound technique, which includes dynamic imaging, should be a consideration when the ultrasound examination is performed for this diagnosis [17].
Treatment
Initial
Pain and edema are managed with ice, nonsteroidal anti-inflammatory drugs, and rest. Initial treatment of a first-degree (grade I) UCL sprain is taping for activity. Initial treatment of an incomplete (grade II) UCL sprain involves immobilization in a thumb spica cast for 3 to 6 weeks with the thumb slightly abducted. Injuries involving nondisplaced or small avulsion fractures associated with an incomplete UCL tear can also be managed nonsurgically and may require a longer course of immobilization. The cast may be extended to include the wrist for greater stability [18]. An alpine splint allows interphalangeal flexion while prohibiting abduction and extension of the first MCP joint [19]. A study of 63 cases of nonoperative and postsurgical patients compared short arm plaster cast immobilization with functional splinting that prevented ulnar and radial deviation of the thumb; there was no difference between the two groups in regard to stability, thumb range of motion or strength, and length of sick leave after an average follow-up of 15 months [20]. Even slightly displaced avulsion fractures without complete UCL rupture tended to do well with immobilization in a study of 30 patients; those with larger bone fragments and larger initial rotation of the fragment were more likely to have residual symptoms [21].
Grade III injuries require surgical repair unless surgery is contraindicated for other reasons. Prompt referral for surgical consultation is recommended to maximize ligament positioning for reattachment. Failure to refer promptly or misdiagnosis of a complete tear can result in a less favorable outcome, including a Stener lesion [5].
Rehabilitation
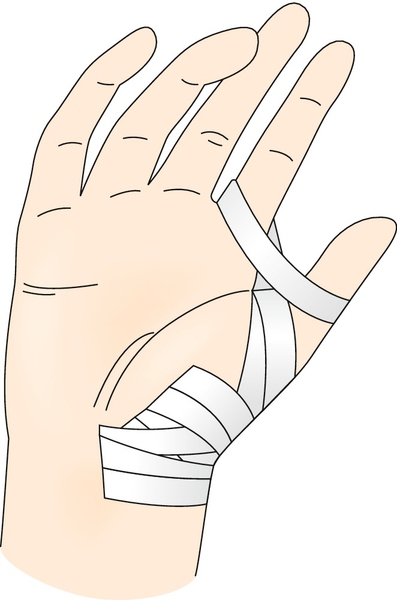
Physical or occupational therapy is important in the rehabilitation management of UCL sprains. Therapists who have completed special training and are certified hand therapists (often called CHTs) can be great resources. Range of motion of the unaffected joints of the arm, especially the interphalangeal joint of the thumb, must be maintained. In the setting of a grade I sprain, after a short course of relative rest and taping, therapy may be required to restore strength to the preinjury level. In grade II sprains, a volar splint replaces the cast after 3 to 6 weeks. Splints may be custom molded by the therapist. They can be removed for daily active range of motion exercises. Passive range of motion and isometric strength training are initiated once pain at rest has resolved, and the patient is progressed to concentric exercise after about 8 weeks for nonsurgical lesions and 10 to 12 weeks for postsurgical lesions. Prophylactic taping is appropriate for transitioning back to sports-specific activity (Fig. 38.2). Postsurgical rehabilitation is less aggressive, with avoidance of strengthening, especially a power pinch, for 8 weeks postoperatively [22]. Protected early postoperative range of motion is indicated [23]. Full activity after grade II tears with or without nondisplaced avulsion fractures begins at 10 to 12 weeks compared with 12 to 16 weeks for surgically repaired injuries [24].
Procedures
There are no specific nonsurgical procedures performed for this injury.
Surgery
Early direct repair is required in the setting of a ruptured UCL (grade III) injury. Grade II and grade III injuries resulting in severe instability, displaced fractures, or intra-articular fragments are also surgical candidates. Surgery is indicated in the setting of gross instability [25]. Surgery is also indicated if the thumb is unstable in extension (more than 30 degrees of laxity or 15 degrees more laxity than on the noninjured side), which indicates a complete rupture, and ligament displacement is likely [8]. Tension wiring is used to fixate avulsions; open reduction may be required for large displaced avulsion defects. Surgical approaches that improve stability are the focus of new techniques [26,27]. However, postoperative immobilization is being reconsidered. A cadaver study concluded that a controlled active motion therapy protocol after suture anchor repair of a ruptured UCL is safe from a biomechanical point of view [28]. Reconstruction may be necessary for a chronic tear, including bone-retinaculum-bone reconstruction [29].
The techniques for reconstruction of chronic UCL injuries or gamekeeper’s thumb involve either dynamic or static procedures. Dynamic procedures use musculotendinous units to stabilize the MCP joint by pulling the proximal phalanx ulnarward. Static procedures use free tendon grafts through bone tunnels or pull-out sutures to reconstruct the proper and accessory collateral ligaments. Static procedures have gained in popularity as they allow ligament reconstruction and preservation of existing thumb function, whereas dynamic procedures require the removal of existing muscle units and do not restore the anatomy of the ulnar collateral ligament [30].
Potential Disease Complications
Disease complications include chronic laxity with associated functional limitations, pain, and inability to pinch [31]; premature arthritis and persistent pain in the first MCP joint; and decreased range of motion of the thumb.
Potential Treatment Complications
Analgesics and nonsteroidal anti-inflammatory drugs have well-known side effects that most commonly affect the gastric, renal, and hepatic systems. Prolonged splinting can lead to loss of range of motion of the joint and weakness and atrophy of the surrounding joints, depending on the extent of the injury and the length of time spent in a splint. Surgical risks include nonunion of avulsed fragments and the typical infrequent surgical complications, such as infection and bleeding. Surgery can result in persistent numbness on the ulnar aspect of the thumb. A neurapraxia secondary to injury of the radial sensory nerve from either swelling or intraoperative traction is the most common nerve injury and usually resolves spontaneously [8,32].







