Procedure 38 Reconstruction for Congenital Thumb Hypoplasia
Congenital thumb hypoplasia can vary from mild size discrepancy to complete absence. The Blauth classification is useful for categorizing the degree of development (Table 38-1). It is critical to assess the stability of the thumb carpometacarpal (CMC) joint to determine the appropriate surgical treatment for thumb hypoplasia. The goal of surgical intervention for children with a stable CMC joint (Blauth types I, II, and IIIA) is preservation of the existing thumb and augmentation of the deficient soft tissue elements. Conversely, if the CMC joint is unstable or absent (Blauth types IIIB, IV, and V), any remnants of the existing thumb should be ablated, and reconstruction should proceed by pollicizing the index finger. This chapter focuses on the reconstruction of Blauth types I, II, and IIIA hypoplasia.
Table 38-1 Blauth Classification of Thumb Hypoplasia and Treatment Options
| Type | Features | Treatment Options |
|---|---|---|
| I | Mild hypoplasia with all elements present | No treatment |
| II | Narrow first web, ulnar collateral ligament insufficiency, and absence of thenar intrinsic muscles | No treatment Z-plasty of first web, UCL strengthening/reconstruction, and opponensplasty |
| III | Type II plus extrinsic tendon deficiencies and/or skeletal deficiency | |
| IIIA | Stable CMC joint | Same as type II |
| IIIB | Unstable CMC joint | Pollicization |
| IV | Absent metacarpal and rudimentary phalanges “Pouce flottant” |
Pollicization |
| V | Total absence | Pollicization |
Indications
 Congenital thumb hypoplasia is seen with a stable CMC joint with varying degrees of soft tissue deficiency (Blauth types I, II, and IIIA). The important soft tissue deficiencies are the following:
Congenital thumb hypoplasia is seen with a stable CMC joint with varying degrees of soft tissue deficiency (Blauth types I, II, and IIIA). The important soft tissue deficiencies are the following:
 Reconstructive procedures for thumb hypoplasia (Blauth types I, II, and IIIA) can be performed at a later age (2 to 4 years) because the child can use the thumb for activities without developing maladaptive compensation patterns. However, it is preferable to correct these deformities before the child enters school to avoid any stigma from an uncorrected deformity.
Reconstructive procedures for thumb hypoplasia (Blauth types I, II, and IIIA) can be performed at a later age (2 to 4 years) because the child can use the thumb for activities without developing maladaptive compensation patterns. However, it is preferable to correct these deformities before the child enters school to avoid any stigma from an uncorrected deformity.
Examination/Imaging
Clinical Examination
 The child should be examined to assess the degree of first web narrowing, opposition function of the thumb, and stability of the thumb MCP joint (Fig. 38-1). Serial examination of a child is required to differentiate between Blauth types IIIA and IIIB. A newborn child uses digital grasp and begins to use the thumb in grasp at about 1 year of age. If the child uses the thumb in manipulating objects, this suggests that a type IIIA deficiency is present. If the child prefers to grasp objects between the index and long finger web space, this web space appears wider because the index finger is pronated toward the thumb. This suggests type IIIB hypoplasia because the child is incapable of using the unstable thumb for effective pinch.
The child should be examined to assess the degree of first web narrowing, opposition function of the thumb, and stability of the thumb MCP joint (Fig. 38-1). Serial examination of a child is required to differentiate between Blauth types IIIA and IIIB. A newborn child uses digital grasp and begins to use the thumb in grasp at about 1 year of age. If the child uses the thumb in manipulating objects, this suggests that a type IIIA deficiency is present. If the child prefers to grasp objects between the index and long finger web space, this web space appears wider because the index finger is pronated toward the thumb. This suggests type IIIB hypoplasia because the child is incapable of using the unstable thumb for effective pinch.
 The entire upper extremity should be examined for other elements of radial deficiency, and patients should be examined for systemic manifestations of associated hematologic and cardiac syndromes such as Holt-Oram, thrombocytopenia-absent-radius (TAR) syndrome, VACTERL (i.e., vertebral abnormalities, anal atresia, cardiac abnormalities, tracheoesophageal fistula and/or esophageal atresia, renal agenesis and dysplasia, and limb defects), and Fanconi anemia.
The entire upper extremity should be examined for other elements of radial deficiency, and patients should be examined for systemic manifestations of associated hematologic and cardiac syndromes such as Holt-Oram, thrombocytopenia-absent-radius (TAR) syndrome, VACTERL (i.e., vertebral abnormalities, anal atresia, cardiac abnormalities, tracheoesophageal fistula and/or esophageal atresia, renal agenesis and dysplasia, and limb defects), and Fanconi anemia.
Surgical Anatomy
 The anatomic deficiencies associated with thumb hypoplasia are detailed in Figure 38-3. The ulnar collateral ligament spans the MCP joint of the thumb and is lax in type II and type III thumbs.
The anatomic deficiencies associated with thumb hypoplasia are detailed in Figure 38-3. The ulnar collateral ligament spans the MCP joint of the thumb and is lax in type II and type III thumbs.
 The intrinsic muscles of the thumb (abductor pollicis brevis [APB], opponens pollicis [OP], flexor pollicis brevis [FPB], and adductor pollicis [AP]) are deficient in types II and III and absent in types IV and V.
The intrinsic muscles of the thumb (abductor pollicis brevis [APB], opponens pollicis [OP], flexor pollicis brevis [FPB], and adductor pollicis [AP]) are deficient in types II and III and absent in types IV and V.
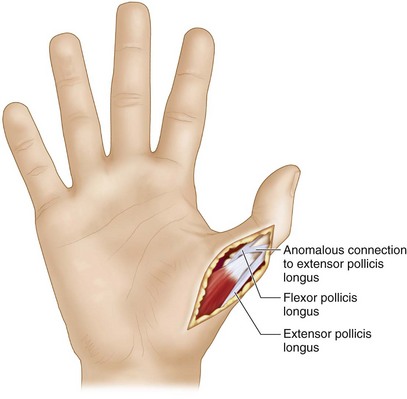
 The flexor pollicis longus (FPL) and extensor pollicis longus (EPL) are hypoplastic in type III thumbs. Often, there may be an anomalous connection between the FPL and the EPL at the level of the MCP joint, known as pollex abductus. This connection can attenuate the UCL over time and prevent active interphalangeal joint motion.
The flexor pollicis longus (FPL) and extensor pollicis longus (EPL) are hypoplastic in type III thumbs. Often, there may be an anomalous connection between the FPL and the EPL at the level of the MCP joint, known as pollex abductus. This connection can attenuate the UCL over time and prevent active interphalangeal joint motion.
Exposures
 The authors use a four-flap Z-plasty to widen the first web space and perform a transfer of the abductor digiti minimi (Huber transfer) for opponensplasty (Fig. 38-4), and a reefing combined with an adductor advancement for strengthening the UCL and stabilizing the MCP joint. All patients may not need all three procedures, and incisions should be planned appropriately.
The authors use a four-flap Z-plasty to widen the first web space and perform a transfer of the abductor digiti minimi (Huber transfer) for opponensplasty (Fig. 38-4), and a reefing combined with an adductor advancement for strengthening the UCL and stabilizing the MCP joint. All patients may not need all three procedures, and incisions should be planned appropriately.
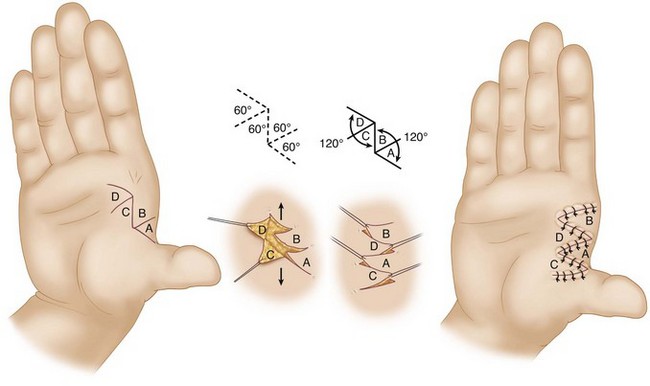
 The four-flap Z-plasty is designed by drawing a line along the first web space from the base of the thumb to the base of the index finger (Fig. 38-5). A dorsal limb is added along the dorsum of the thumb MCP joint at 120 degrees to the previous line. Similarly, a palmar limb is added along the palmar aspect of the index finger MCP joint at 120 degrees to the line (see Fig. 38-5). The dorsal limb of the Z-plasty is usually sufficient for exposure of the UCL. However, if a Z-plasty is not required, a 2-cm curvilinear incision can be made over the ulnar aspect of the base of the thumb MCP joint (Fig. 38-6).
The four-flap Z-plasty is designed by drawing a line along the first web space from the base of the thumb to the base of the index finger (Fig. 38-5). A dorsal limb is added along the dorsum of the thumb MCP joint at 120 degrees to the previous line. Similarly, a palmar limb is added along the palmar aspect of the index finger MCP joint at 120 degrees to the line (see Fig. 38-5). The dorsal limb of the Z-plasty is usually sufficient for exposure of the UCL. However, if a Z-plasty is not required, a 2-cm curvilinear incision can be made over the ulnar aspect of the base of the thumb MCP joint (Fig. 38-6).
 A 2-cm chevron incision is marked over the radial aspect of the thumb MCP joint to expose the APB tendon (Fig. 38-7).
A 2-cm chevron incision is marked over the radial aspect of the thumb MCP joint to expose the APB tendon (Fig. 38-7).
 A curvilinear incision is marked from 1 cm proximal and ulnar to the pisiform, along the radial aspect of the hypothenar eminence, to the ulnar aspect of the base of the small finger to expose the hypothenar muscles for thumb abductorplasty (see Fig. 38-7).
A curvilinear incision is marked from 1 cm proximal and ulnar to the pisiform, along the radial aspect of the hypothenar eminence, to the ulnar aspect of the base of the small finger to expose the hypothenar muscles for thumb abductorplasty (see Fig. 38-7).
Pearls
The radial limb of the four-flap Z-plasty should be designed dorsally, and the ulnar limb should be designed in a palmar direction. This will allow exposure of the thumb MCP joint and UCL through the radial limb incision.
The incision for exposure of the abductor digiti minimi (ADM) should not be along the ulnar border of the hand but slightly palmar, so that the scar is not compressed when the hand is resting.
Procedure
Step 1: Elevation of Four-Flap Z-Plasty Flaps
Step 3: Pinning of Thumb MCP Joint
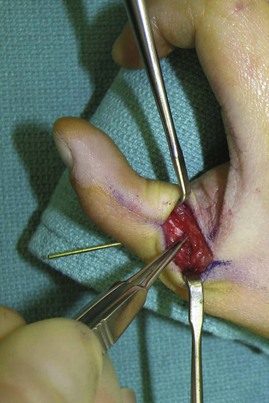
 A single 0.045-inch K-wire is passed obliquely from radial to ulnar through the MCP joint to maintain the MCP joint in neutral position (Fig. 38-8).
A single 0.045-inch K-wire is passed obliquely from radial to ulnar through the MCP joint to maintain the MCP joint in neutral position (Fig. 38-8).
Step 5: Transposition of Four-Flap Z-Plasty Flaps
 The Z-plasty flaps are transposed and sutured using 4-0 chromic catgut.
The Z-plasty flaps are transposed and sutured using 4-0 chromic catgut.
 Figure 38-5 shows the arrangement of the flaps before and after transposition.
Figure 38-5 shows the arrangement of the flaps before and after transposition.
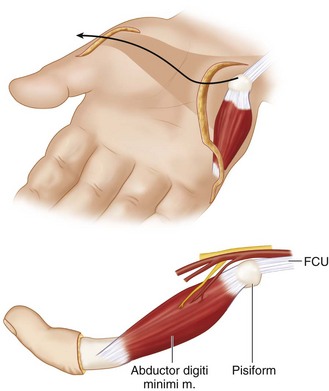
Step 7: Exposure of the ADM
 The skin is incised in line with the previously marked incision. The ADM is identified in the midportion of the hypothenar eminence and is the most ulnar and superficial of the hypothenar muscles in this location. More proximally, the palmaris brevis overlies the ADM, but it can be differentiated by the transverse orientation of its fibers.
The skin is incised in line with the previously marked incision. The ADM is identified in the midportion of the hypothenar eminence and is the most ulnar and superficial of the hypothenar muscles in this location. More proximally, the palmaris brevis overlies the ADM, but it can be differentiated by the transverse orientation of its fibers.
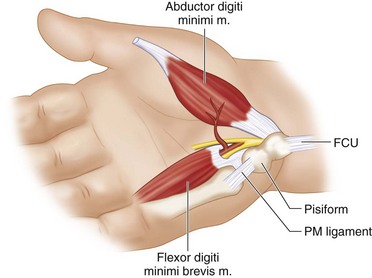
 The ADM is separated from the other hypothenar muscles, including the opponens digiti minimi and the flexor digiti minimi, which are deeper and more radial (Fig. 38-10).
The ADM is separated from the other hypothenar muscles, including the opponens digiti minimi and the flexor digiti minimi, which are deeper and more radial (Fig. 38-10).
Step 7 Pitfalls
Care must be taken to identify and protect the digital nerve to the ulnar side of the small finger. This nerve will pass obliquely superficial to the ADM in the distal half of the incision.
The palmaris brevis should be divided to mobilize the proximal portion of the ADM. Care must be taken to protect motor branches of the ulnar nerve during proximal mobilization of the ADM.
Step 8: Division of the Insertion of the ADM
Step 9: Elevation of the ADM
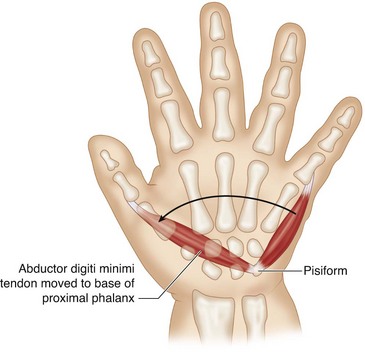
 The ADM is elevated to its origin from the pisiform. The neurovascular bundle to the ADM enters the muscle on the dorsoradial aspect, and care must be taken during proximal elevation of the muscle to prevent injury to the pedicle (Fig. 38-13). The pedicle does not need to be visualized during the harvest. The muscle is dissected to its insertion at the pisiform.
The ADM is elevated to its origin from the pisiform. The neurovascular bundle to the ADM enters the muscle on the dorsoradial aspect, and care must be taken during proximal elevation of the muscle to prevent injury to the pedicle (Fig. 38-13). The pedicle does not need to be visualized during the harvest. The muscle is dissected to its insertion at the pisiform.
Step 10: Creation of a Subcutaneous Tunnel
Step 11: Transfer of the ADM
 The elevated ADM is turned 180 degrees like the page of a book, rather than rotating it 90 degrees, to prevent twisting of the pedicle (Fig. 38-14).
The elevated ADM is turned 180 degrees like the page of a book, rather than rotating it 90 degrees, to prevent twisting of the pedicle (Fig. 38-14).
 A hemostat passed from the incision at the radial aspect of the thumb through the subcutaneous tunnel is used to bring the ADM to the radial aspect of the thumb MCP joint.
A hemostat passed from the incision at the radial aspect of the thumb through the subcutaneous tunnel is used to bring the ADM to the radial aspect of the thumb MCP joint.
 The ADM tendon reaches the APB insertion with sufficient tension, and overcorrection is unnecessary.
The ADM tendon reaches the APB insertion with sufficient tension, and overcorrection is unnecessary.
 The ADM tendon is passed under the APB insertion and anchored with 4-0 Ethibond mattress sutures (Fig. 38-15).
The ADM tendon is passed under the APB insertion and anchored with 4-0 Ethibond mattress sutures (Fig. 38-15).
Postoperative Care and Expected Outcomes
 The child is maintained in a thumb spica splint for 4 weeks. The K-wire is removed at 4 weeks and a thermoplastic splint fashioned to maintain the position of the thumb.
The child is maintained in a thumb spica splint for 4 weeks. The K-wire is removed at 4 weeks and a thermoplastic splint fashioned to maintain the position of the thumb.
 At 4 weeks, children are started on range-of-motion and strengthening exercises and are weaned off the splint gradually over a period of 2 to 4 weeks.
At 4 weeks, children are started on range-of-motion and strengthening exercises and are weaned off the splint gradually over a period of 2 to 4 weeks.
 The results of surgery for thumb hypoplasia are good, and almost all patients have improvements in thumb function.
The results of surgery for thumb hypoplasia are good, and almost all patients have improvements in thumb function.
Abdel-Ghani H, Amro S. Characteristics of patients with hypoplastic thumb: a prospective study of 51 patients with the results of surgical treatment. J Pediatr Orthop. 2004;13:127-138.
Fraulin FO, Thomson HG. First webspace deepening: comparing the four-flap and five-flap Z-plasty. Which gives the most gain? Plast Reconstr Surg. 1999;104:120-128.