CASE 38 How to Assess Lesions of Intermediate Severity
FFR or IVUS?
Cardiac catheterization
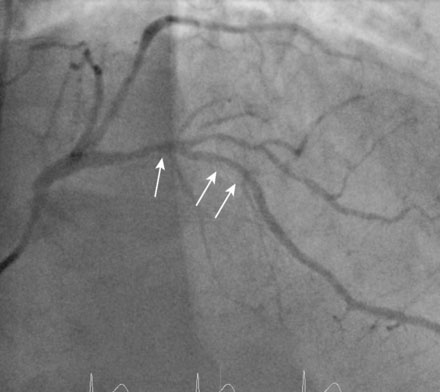
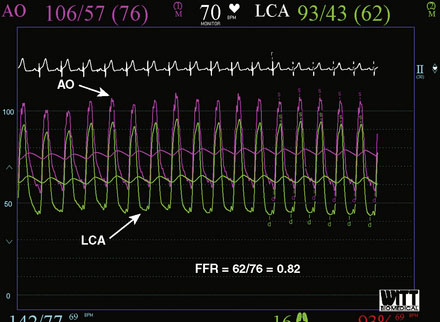
There was a severe stenosis of a small, distal branch of the right coronary artery, which appeared to represent the culprit lesion (Figure 38-1 and Video 38-1). The operator considered this artery too small and the lesion too distal for intervention. Atherosclerotic plaque without significant narrowing was seen in the mid-right coronary artery and the first obtuse marginal artery. A long, moderate stenosis affected the proximal to midsegment of the left anterior descending (LAD) artery at a bifurcation with a large diagonal branch (Figure 38-2 and Video 38-2). The left ventriculogram revealed normal function and no specific wall motion abnormalities. Concerned about the lesion of intermediate severity seen in the left anterior descending artery, the physician decided to assess the lesion’s significance by measuring fractional flow reserve, or FFR. Thus, a guide catheter was engaged in the left coronary artery and, after administering a bolus of 50 U/kg of unfractionated heparin, the operator advanced a pressure wire to the distal LAD. The wire transducer was placed distal to the LAD lesion and simultaneous distal coronary pressure and aortic pressure from the guide catheter tip were sampled after maximum coronary vasodilatation was achieved with 100 mcg of intracoronary adenosine (Figure 38-3). Fractional flow reserve was calculated as the ratio of the mean coronary pressure distal to the stenosis (62 mmHg) to mean pressure of the aorta at the guide catheter (76 mmHg) during maximal hyperemia. This ratio calculated to an FFR of 0.82. Thus, the lesion was determined to be a non–flow-limiting stenosis. Based on the results of the angiogram and the FFR determination, it was decided to treat him medically.
Discussion
Coronary angiography forms the basis for revascularization decisions in patients with coronary artery disease. When an artery appears normal or minimally diseased or if there is an obvious, severe stenosis, interpretation is easy and decision-making straightforward. However, angiography has well-known limitations, particularly for lesions of moderate or intermediate severity, arbitrarily defined as a 40% to 70% stenosis.1 In addition, lesions are often eccentric or may be within segments difficult to visualize clearly, leaving the physician with doubt as to the stenosis severity. In such circumstances, adjunctive testing helps the physician decide the significance of a lesion with greater confidence.
Assessment of an ambiguous lesion with intravascular ultrasound requires the identification of a “worse” segment (minimal luminal diameter) and quantification of the lumen. It is not appropriate to make a decision based on the observation that the IVUS “looks bad,” as it is the degree of anatomic lumen compromise that determines lesion significance, not the atherosclerotic plaque burden. In patients with intermediate stenoses of major epicardial arteries (excluding the left main stem), the following IVUS parameters are associated with “significant” lesions”: 1) minimal luminal cross-sectional area narrowing less than 4.0 mm2; 2) minimal luminal diameter less than 1.8 to 2.0 mm; and 3) percentage of area stenosis greater than 70%.2,3 Left main stem lesions are deemed significant if the minimal luminal area is less than 6 mm2 in one study4 and less than 7.5 mm2 in another.5 There are several important caveats to the use of IVUS for determination of lesion significance. First, IVUS parameters have been validated only in large, proximal arteries (average 3.0 mm). The absolute lumen values noted above do not apply to small or distal arteries. Second, disease involving a long segment or tandem proximal lesions may not narrow the lumen below the threshold diameter at any given slice, yet may still compromise flow. Finally, the IVUS catheter may cause spasm, leading to an artifactually small lumen.
Fractional flow reserve describes the ratio of the maximum achievable flow in the presence of a stenosis to the theoretical maximum flow in the same vessel in the absence of a stenosis. It is simple to perform, requiring the measurement of simultaneous aortic and distal coronary pressures using a special angioplasty guidewire outfitted with a micromanometer during maximal hyperemia. The mathematics, experimental basis, technique, limitations, and validation of FFR have been well-described.6–11 It can be calculated simply by the formula:
The unequivocal normal value of 1.0 is well accepted and has been firmly established in humans. The value below which a stenosis is deemed “significant” is of some debate. Multiple studies confirmed that lesions associated with ischemia have FFR <0.75. Lesions with FFR between 0.75 and 0.80 are generally recognized as “borderline” and may, in fact, represent significant lesions. In such cases, decisions regarding revascularization require clinical judgment. Importantly, there are numerous studies demonstrating that revascularization of lesions with FFR greater than 0.75 to 0.80 can safely be deferred, thereby establishing FFR as a valuable tool and important adjunct to angiography in clinical decision making.12–14
In the case presented here, the culprit vessel was clearly a distal branch of the right coronary artery and FFR was used to assess a lesion found incidentally on angiography. This scenario is very commonly encountered. Importantly, FFR was recently found to be superior to an angiography-guided strategy in determining which vessels need revascularization in patients with multivessel coronary disease.15 Recently published practice guidelines have established measurement of FFR as a Class IIa indication to determine whether PCI of a specific lesion is warranted and as an alternative to noninvasive functional testing such as stress testing for assessment of the effects of intermediate stenoses (30% to 70%) in patients with anginal syndromes.16
1. Fischer J.J., Samady H., McPherson J.A., Sarembock I.J., Powers E.R., Gimple L.W., Ragosta M. Comparison between visual assessment and quantitative angiography versus fractional flow reserve for native coronary narrowings of moderate severity. Am J Cardiol. 2002;90:210-215.
2. Briguori C., Anzuini A., Airoldi F., Gimelli G., Nishida T., Adamian M., Corvaja N., DiMario C., Colombo A. Intravascular ultrasound criteria for the assessment of the functional significance of intermediate coronary artery stenoses and comparison with fractional flow reserve. Am J Cardiol. 2001;87:136-141.
3. Abizaid A., Mintz G.S., Pichard A.D., Kent K.M., Satler L.F., Walsh C.L., Popma J.J., Leon M.B. Clinical, intravascular ultrasound, and quantitative angiographic determinants of the coronary flow reserve before and after percutaneous transluminal coronary angioplasty. Am J Cardiol. 1998;82:423-428.
4. Vasti V., Ivan E., Yalamanchili V., Wongpraparut N., Leesar M.A. Correlations between fractional flow reserve and intravascular ultrasound in patients with an ambiguous left main coronary artery stenosis. Circulation. 2004;110:2831-2836.
5. Fassa A.A., Wagatsuma K., Higano S.T., Mathew V., Barsness G.W., Lennon R.J., Holmes D.R., Lerman A. Intravascular ultrasound guided treatment for angiographically indeterminate left main coronary artery disease. A long term follow-up study. J Am Coll Cardiol. 2005;45:204-211.
6. Pijls N.H.J., van Son J.A.M., Kirkeeide R.L., De Bruyne B., Gould K.L. Experimental basis of determining maximum coronary, myocardial, and collateral blood flow by pressure measurements for assessing functional stenosis severity before and after percutaneous transluminal coronary angioplasty. Circulation. 1993;87:1354-1367.
7. Pijls N.H.J., Van Gelder B., Van der Voort P., Peels K., Bracke F.A.L.E., Bonnier H.J.R.M., El Gamal M.I.H. Fractional flow reserve: a useful index to evaluate the influence of an epicardial coronary stenosis on myocardial blood flow. Circulation. 1995;92:3183-3193.
8. De Bruyne B., Baudhuin T., Melin J.A., Pijls N.H., Sys S.U., Bol A., Paulus W.J., Heyndrickx G.R., Wijns W. Coronary flow reserve calculated from pressure measurements in humans: validation with positron emission tomography. Circulation. 1994;89:1013-1022.
9. De Bruyne B., Bartunek J., Sys S.U., Heyndrickx G.R. Relation between myocardial fractional flow reserve calculated from coronary pressure measurements and exercise-induced myocardial ischemia. Circulation. 1995;92:39-46.
10. Pijls N.H.J., De Bruyne B., Peels K., van der Voort P.H., Bonnier H.J.R.M., Bartunek J., Koolen J.J. Measurement of fractional flow reserve to assess the functional severity of coronary-artery stenoses. N Engl J Med. 1996;334:1703-1708.
11. Bishop A.H., Samady H. Fractional flow reserve: critical review of an important physiologic adjunct to angiography. Am Heart J. 2004;147:792-802.
12. Bech G.J.W., DeBruyne B., Bonnier H.J.R.M., Bartunek J., Wijns W., Peels K., Heyndrickx G.R., Koolen J.J., Pijls N.H.J. Long-term follow-up after deferral of percutaneous transluminal coronary angioplasty of intermediate stenosis on the basis of coronary pressure measurement. J Am Coll Cardiol. 1998;31:841-847.
13. Bech G.J., DeBruyne B., Pijls N.H., deMuinck E.D., Hoorntje J.C., Escaned J., Stella P.R., Boersma E., Bartunek J., Koolen J.J., Wijns W. Fractional flow reserve to determine the appropriateness of angioplasty in moderate coronary stenosis: a randomized trial. Circulation. 2001;103:2928-2934.
14. Pijls N.H.J., van Schaardenburgh P., Manoharan G., Boersma E., Bech J.W., van’t Veer M., Bar F., Hoorntje J., Koolen J., Wijns W., De Bruyne B. Percutaneous coronary intervention of functionally non-significant stenosis. 5 year follow-up of the DEFER study. J Am Coll Cardiol. 2007;49:2105-2111.
15. Tonino P.A.L., DeBruyne B., Pijls N.H.J., Siebert U., Ikeno F., van’t Veer M., Klauss V., Manoharan G., Engstrom T., Oldroyd K.G., Ver Lee P.N., MacCarthy P.A., Fearon W.F., FAME Study Investigators. Fractional flow reserve versus angiography for guiding percutaneous coronary intervention. For the N Engl J Med 2009;360:213-224.
16. Kushner F.G., Hand M., Smith S.C.Jr, King S.B.3rd, Anderson J.L., Antman E.M., Bailey S.R., Bates E.R., Blankenship J.C., Casey D.E.Jr, Green L.A., Hochman J.S., Jacobs A.K., Krumholz H.M., Morrison D.A., Ornato J.P., Pearle D.L., Peterson E.D., Sloan M.A., Whitlow P.L., Williams D.O. 2009 focused updates: ACC/AHA guidelines for the management of patients with ST-elevation myocardial infarction (updating the 2004 guideline and 2007 focused update) and ACC/AHA/SCAI guidelines on percutaneous coronary intervention (updating the 2005 guideline and 2007 focused update): a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2009;54:2205-2241.