Procedure 37 Duplicated Thumb Reconstruction
![]() See Video 31: Duplicated Thumb Reconstruction
See Video 31: Duplicated Thumb Reconstruction
Indications
 The goal of thumb reconstruction is to restore an acceptable appearance without compromising existing function. Although a child with thumb duplication can function perfectly without reconstruction, the stigma associated with an uncorrected deformity may be unacceptable for the child or the parents, or both.
The goal of thumb reconstruction is to restore an acceptable appearance without compromising existing function. Although a child with thumb duplication can function perfectly without reconstruction, the stigma associated with an uncorrected deformity may be unacceptable for the child or the parents, or both.
 Reconstruction should be considered at about 12 months of age, before the development of significant deviation deformity and because of the ease of general anesthesia. Furthermore, dissection of anatomic structures is easier compared with younger ages, and the development of pinch grasp occurs at about 12 months.
Reconstruction should be considered at about 12 months of age, before the development of significant deviation deformity and because of the ease of general anesthesia. Furthermore, dissection of anatomic structures is easier compared with younger ages, and the development of pinch grasp occurs at about 12 months.
Examination/Imaging
Clinical Examination
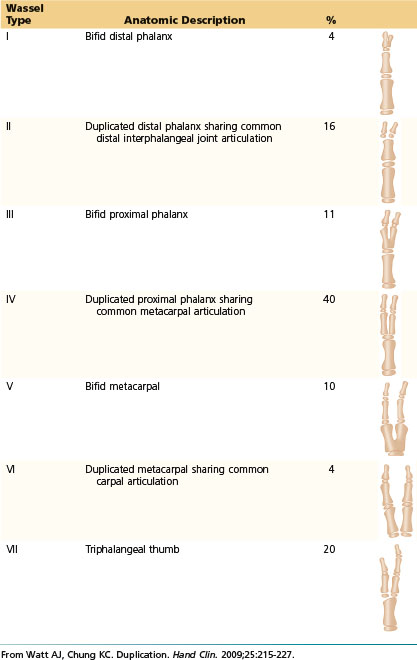
 The classification of duplicated thumb is based on the level of duplication, which ranges from type I, which is partial split of the distal phalanx, to type VII, which is complete split of the metacarpal (Table 37-1). The type corresponds to the number of abnormal skeletal elements present. For example, type III has three abnormal bones (two distal phalanges and a partially split proximal phalanx). Wassel type IV is the most common type (Fig. 37-1).
The classification of duplicated thumb is based on the level of duplication, which ranges from type I, which is partial split of the distal phalanx, to type VII, which is complete split of the metacarpal (Table 37-1). The type corresponds to the number of abnormal skeletal elements present. For example, type III has three abnormal bones (two distal phalanges and a partially split proximal phalanx). Wassel type IV is the most common type (Fig. 37-1).
 Genetic counseling is usually not necessary except for type VII, which is associated with other congenital anomalies and is inherited in an autosomal dominant pattern.
Genetic counseling is usually not necessary except for type VII, which is associated with other congenital anomalies and is inherited in an autosomal dominant pattern.
 The duplicated elements are abnormal in size and shape, and the radial duplicate is typically smaller in size. The surgeon should examine the thumb for the level of duplication, the degree of hypoplasia of each component, stability of the involved joints, and position of the thumb with respect to the bony axis and first web space.
The duplicated elements are abnormal in size and shape, and the radial duplicate is typically smaller in size. The surgeon should examine the thumb for the level of duplication, the degree of hypoplasia of each component, stability of the involved joints, and position of the thumb with respect to the bony axis and first web space.
Table 37-1 Classification of Thumb Duplication
Imaging
 Preoperative radiographs are indicated to identify the size and number of duplicated skeletal elements and to determine whether the elements are attached (bifid) or separated (duplicate) (Fig. 37-2).
Preoperative radiographs are indicated to identify the size and number of duplicated skeletal elements and to determine whether the elements are attached (bifid) or separated (duplicate) (Fig. 37-2).
 The osseous anatomy is abnormal, with varying degrees of bony hypoplasia as well as widening and angulation of the articular surfaces.
The osseous anatomy is abnormal, with varying degrees of bony hypoplasia as well as widening and angulation of the articular surfaces.
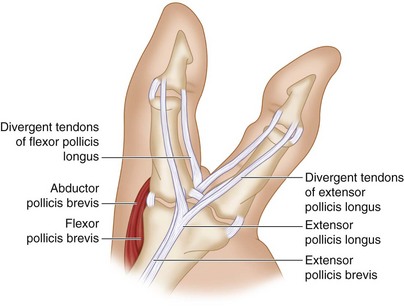
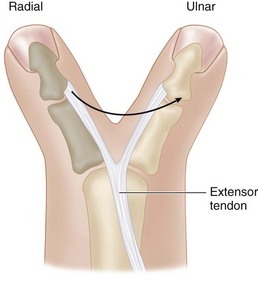
Surgical Anatomy
 The flexor and extensor tendons are split and insert eccentrically. An abnormal connection between the flexor and extensor tendons on the radial aspect of the thumb often exists as well. The origins and insertions of the thenar musculature, particularly the opponens pollicis (OP), are aberrant in cases of proximal duplication. The abductor pollicis brevis (APB) and flexor pollicis brevis (FPB) insert into the proximal phalanx of the radial duplicate, whereas the OP inserts into the radial metacarpal. The net effect of the long flexor tendons is to pull the distal phalanges into convergence while the thenar insertions create divergence at the proximal phalangeal level, creating a zigzag deformity (Fig. 37-3).
The flexor and extensor tendons are split and insert eccentrically. An abnormal connection between the flexor and extensor tendons on the radial aspect of the thumb often exists as well. The origins and insertions of the thenar musculature, particularly the opponens pollicis (OP), are aberrant in cases of proximal duplication. The abductor pollicis brevis (APB) and flexor pollicis brevis (FPB) insert into the proximal phalanx of the radial duplicate, whereas the OP inserts into the radial metacarpal. The net effect of the long flexor tendons is to pull the distal phalanges into convergence while the thenar insertions create divergence at the proximal phalangeal level, creating a zigzag deformity (Fig. 37-3).
 The arterial supply of the duplicated thumb most commonly consists of a single digital artery located on the ulnar side of the ulnar and radial duplicates, in 74% of cases. Twelve percent of patients exhibit three digital arteries, located on the radial and ulnar sides of the ulnar duplicate and the ulnar side of the radial duplicate. Ten percent of patients exhibit four digital arteries, and 5% maintain a single digital artery associated with the ulnar duplicate.
The arterial supply of the duplicated thumb most commonly consists of a single digital artery located on the ulnar side of the ulnar and radial duplicates, in 74% of cases. Twelve percent of patients exhibit three digital arteries, located on the radial and ulnar sides of the ulnar duplicate and the ulnar side of the radial duplicate. Ten percent of patients exhibit four digital arteries, and 5% maintain a single digital artery associated with the ulnar duplicate.
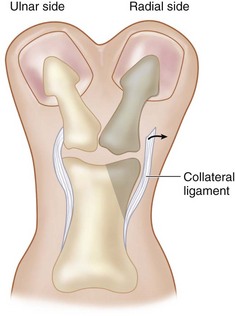
 Stability of the thumb is maintained by the ulnar collateral ligament, and typically the ulnar thumb is retained to preserve this structure.
Stability of the thumb is maintained by the ulnar collateral ligament, and typically the ulnar thumb is retained to preserve this structure.
Positioning
 The procedure is conducted under general anesthesia with the patient placed supine on the operating room table. The entire upper extremity is prepared and draped after a tourniquet is applied.
The procedure is conducted under general anesthesia with the patient placed supine on the operating room table. The entire upper extremity is prepared and draped after a tourniquet is applied.
 Intraoperative fluoroscopy is often required, and the operative table is positioned to allow easy access for the C-arm.
Intraoperative fluoroscopy is often required, and the operative table is positioned to allow easy access for the C-arm.
Exposures
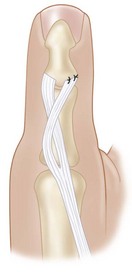
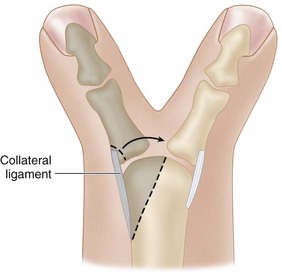
 When removing the radial thumb, one must retain a periosteal flap from the radial collateral ligament of the resected thumb to reconstruct the radial collateral ligament of the retained thumb. The extensor tendon from the resected thumb can be transferred to the ulnar side of the retained thumb for tendon.
When removing the radial thumb, one must retain a periosteal flap from the radial collateral ligament of the resected thumb to reconstruct the radial collateral ligament of the retained thumb. The extensor tendon from the resected thumb can be transferred to the ulnar side of the retained thumb for tendon.
 We describe the reconstruction of a type III and type IV thumb duplication.
We describe the reconstruction of a type III and type IV thumb duplication.
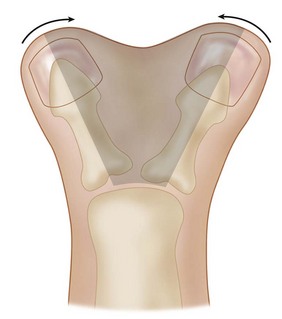
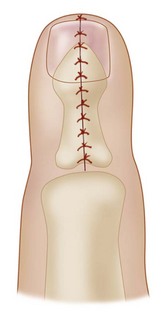
Pearls
The Bilhaut-Cloquet procedure attempts to combine both thumbs into a single unit by removing the central portion of both thumbs to create a single thumb (Figs. 37-4 and 37-5). While conceptually appealing, it is exceedingly difficult to create an aesthetically pleasing thumb. A mismatch of the nail fold is common, and the cleft in the central combined thumb can be noticeable. It is preferable to accept a smaller thumb and use the soft tissue from the resected thumb to augment the size of the retained one.
Procedure
Reconstruction of a Type III Thumb Duplication
Step 1
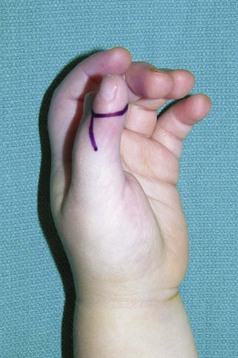
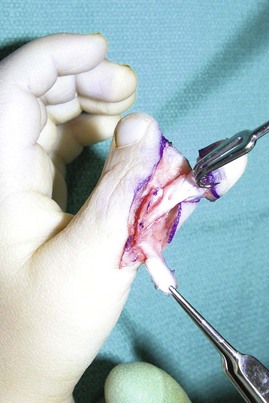
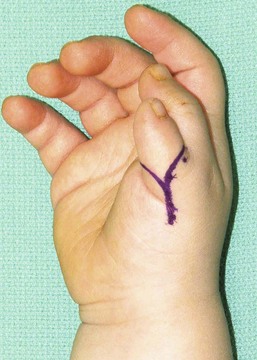
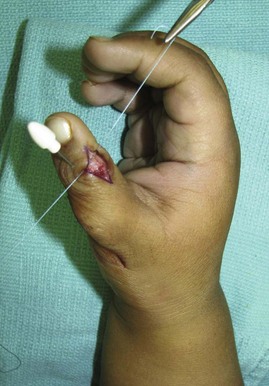
 The radial digit is selected for removal. A curvilinear, Y-shaped incision is made over the radial digit (Figs. 37-6 to 37-8).
The radial digit is selected for removal. A curvilinear, Y-shaped incision is made over the radial digit (Figs. 37-6 to 37-8).
 The soft tissues are dissected to the level of the radial aspect of the interphalangeal joint.
The soft tissues are dissected to the level of the radial aspect of the interphalangeal joint.
 The distal insertions of the flexor tendon, extensor tendon, and radial collateral ligament are carefully elevated off from the base of the distal phalanx of the radial duplicate.
The distal insertions of the flexor tendon, extensor tendon, and radial collateral ligament are carefully elevated off from the base of the distal phalanx of the radial duplicate.
Step 3
Step 5
Procedure
Reconstruction of Type IV Thumb Duplication
Step 1
 The radial digit is selected for removal, and the skin incisions are designed as described previously (Figs. 37-15 and 37-16). The skin flaps are elevated sharply to expose the radial aspect of the metacarpophalangeal joint.
The radial digit is selected for removal, and the skin incisions are designed as described previously (Figs. 37-15 and 37-16). The skin flaps are elevated sharply to expose the radial aspect of the metacarpophalangeal joint.
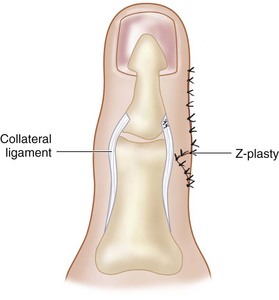
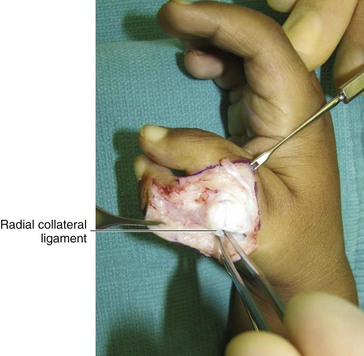
 The insertion of the APB is detached, and the radial collateral ligament is elevated off the base of the radial duplicate on a longitudinal periosteal flap (Fig. 37-17).
The insertion of the APB is detached, and the radial collateral ligament is elevated off the base of the radial duplicate on a longitudinal periosteal flap (Fig. 37-17).
 The extensor and flexor tendons going to the duplicate thumb are divided distally at the level of the interphalangeal joint.
The extensor and flexor tendons going to the duplicate thumb are divided distally at the level of the interphalangeal joint.
Step 2
Step 3
 A partial osteotomy of the radial portion of the head of the metacarpal is done to reduce its prominence. This osteotomy is easily performed using the knife blade with a back-and-forth motion over the unossified metacarpal (Figs. 37-19 and 37-20). Care should be taken to preserve the origin of the radial collateral ligament during this osteotomy.
A partial osteotomy of the radial portion of the head of the metacarpal is done to reduce its prominence. This osteotomy is easily performed using the knife blade with a back-and-forth motion over the unossified metacarpal (Figs. 37-19 and 37-20). Care should be taken to preserve the origin of the radial collateral ligament during this osteotomy.
Step 4
Step 5
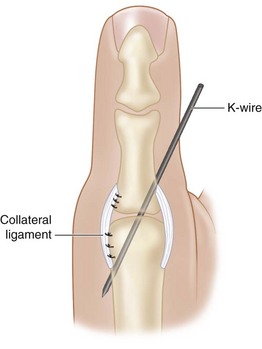
 The periosteal flap carrying the radial collateral ligament and the APB insertion is sutured to the radial base of the proximal phalanx using nonabsorbable braided suture. Additional sutures may be needed to reinfoirce the origin of the radial collateral liagment at the head of the metacarpal (Fig. 37-22).
The periosteal flap carrying the radial collateral ligament and the APB insertion is sutured to the radial base of the proximal phalanx using nonabsorbable braided suture. Additional sutures may be needed to reinfoirce the origin of the radial collateral liagment at the head of the metacarpal (Fig. 37-22).
Baek GH, Gong HS, Chung MS, et al. Modified Bilhaut-Cloquet procedure for Wassel type-II and III polydactyly of the thumb: surgical technique. J Bone Joint Surg [Am]. 2008;90:74-86.
Goldfarb CA, Patterson JM, Maender A, Manske PR. Thumb size and appearance following reconstruction of radial polydactyly. J Hand Surg [Am]. 2008;33:1348-1353.
Horii E, Hattori T, Koh S, Majima M. Reconstruction for Wassel type III radial polydactyly with two digits equal in size. J Hand Surg [Am]. 2009;34:1802-1807.
Ogino T, Ishii S, Takahata S, Kato H. Long-term results of surgical treatment of thumb polydactyly. J Hand Surg [Am]. 1996;21:478-486.