CHAPTER 36
Median Neuropathy (Carpal Tunnel Syndrome)
Definition
Carpal tunnel syndrome (CTS), an entrapment neuropathy of the median nerve at the wrist, is the most common compression neuropathy of the upper extremity. This syndrome produces paresthesias, numbness, pain, subjective swelling, and, in advanced cases, muscle atrophy and weakness of the areas innervated by the median nerve. The condition is often bilateral, although the dominant hand tends to be more severely affected.
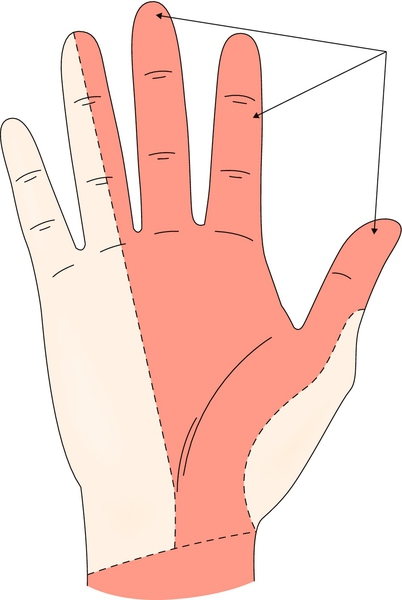
CTS is thought to result from a compression of the median nerve as it passes through the carpal tunnel. The clinical presentation is variable. Whereas there is some variation as to what should be included in this definition, CTS is most often thought to involve sensory changes in the radial 31⁄2 digits of the hand with burning, tingling, numbness, and a subjective sense of swelling. Those affected often first note symptoms at night. In the later stages, complaints include motor weakness in the thenar eminence.
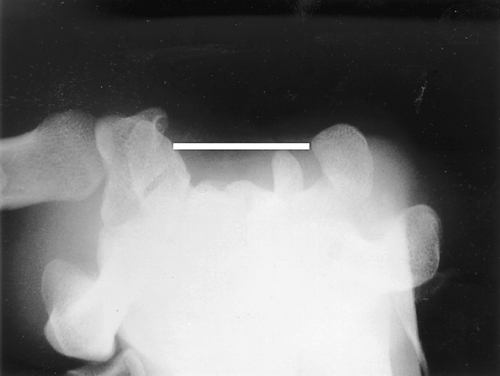
It is helpful to think of the carpal tunnel as a structure with four sides, three of which are defined by the carpal bones and the fourth, the “top” of the tunnel, by the transverse carpal ligament (Figs. 36.1 and 36.2). Passing through the tunnel are the median nerve and nine tendons with their synovial sheaths; these include the flexor pollicis longus, the four flexor digitorum superficialis, and the four flexor digitorum profundus tendons. None of the sides of the tunnel yields well to expansion of the fluid or structures within. Because of this, swelling will increase pressure within the tunnel and may result in compression of the median nerve. CTS occurs more commonly in women than in men, with a prevalence in the general adult population ranging from 2.7% to 5.8% [1,2]. It is most common in middle-aged persons between the ages of 30 and 60 years. The older adults may have objective clinical and electrophysiologic evidence of a more severe median nerve entrapment [3]. Most cases of CTS are idiopathic with congenital predisposition. Some focal or systemic conditions, such as wrist injury, arthritis, diabetes, thyroid disease, rheumatoid arthritis, and pregnancy, can increase pressure on the median nerve in the carpal tunnel and contribute to the development of CTS. Prolonged postures in extremes of wrist flexion or extension, repetitive use of the flexor muscles, and exposure to vibration are the primary exposures that have been reported [4–7]. The pathophysiologic mechanism of CTS involves a combination of mechanical trauma, increased pressure, and ischemic injury to the median nerve within the carpal tunnel [8].

Symptoms
The classic symptoms of CTS include numbness and paresthesias in the radial 31⁄2 fingers (Fig. 36.3). A typical early complaint is awakening in the night with numbness or pain in the fingers. Symptoms during the day are often brought out by activities placing the wrist in substantial flexion or extension or requiring repetitive motion of the structures that traverse the carpal tunnel. Many patients report symptoms outside the distribution of the median nerve as well [9]. Numbness and pain in the hand may also be accompanied by volar wrist pain and aching at the forearm. The patient may describe the symptoms as being positional, with symptoms relieved by the shaking of a hand, often referred to as the flick sign [10].
Patients may complain of a sense of swelling in the hands, often noting that they have difficulty wearing jewelry or watches, with this sensation fluctuating throughout the day or week. Some patients also report dry skin and cold hands. In the later stages of CTS, the numbness may become constant and motor disturbances more apparent, with complaints of weakness manifested by a functional decrease of strength. Patients may then report dropping objects.
Physical Examination
A two-point sensory discrimination test is thought to be the most sensitive of the bedside examination techniques. This involves a comparison of the two-point discriminating sensory ability of the median with that of the ulnar nerve distribution of the hand. Careful observation of the hands, comparing the affected side with the unaffected side and comparing the thenar and hypothenar eminences of the same hand, may reveal an increasing asymmetry. Weakness of the thenar intrinsic muscles of the hand can be tested with a dynamometer or clinically by testing abduction of the thumb against resistance. The more common special tests include the Phalen, the Tinel, and the nerve compression tests. The Phalen test involves a forced flexion at the wrist to 90 degrees for a period of 1 minute; a positive test result reproduces the symptoms of CTS (Fig. 36.4). The reverse Phalen maneuver is the same test completed with forced extension. The Tinel test involves tapping sharply over the volar aspect of the wrist just distal to the distal wrist crease. The test result is positive when a sensory disturbance radiates down the region of the distribution of the median nerve. The nerve compression test involves the placement of two thumbs over the roof of the carpal tunnel, with pressure maintained for 1 minute. The test result is positive if symptoms are reproduced in the area of the distribution of the median nerve. A review showed an overall estimate of 68% sensitivity and 73% specificity for the Phalen test, 50% sensitivity and 77% specificity for the Tinel test, and 64% sensitivity and 83% specificity for the carpal compression test [11]. Two-point discrimination and testing of atrophy or strength of the abductor pollicis brevis proved to be specific but not very sensitive. [11].

Functional Limitations
Functional limitations of CTS often include difficulty with sleep due to frequent awakenings by the symptoms. Because certain sustained or repetitive motions are difficult, tasks that often become more difficult include driving a car and sustained computer keyboard or mouse use at work. The later symptom of weakness in the thenar eminence may result in difficulty maintaining grip. Profound CTS may result in functional limitations, such as the inability to tie one’s shoes, to button shirts, and to put a key in a lock.
Diagnostic Studies
Whereas CTS is a syndrome rather than a singular finding, it is often suggested that the “gold standard” test of CTS is electrodiagnostic testing. Electromyography and nerve conduction studies can confirm the diagnosis, determine the severity (if any) of nerve damage, guide and measure the effect of treatment, and rule out other conditions such as radiculopathy and brachial plexopathy. Ultrasound studies, which reveal an enlarged median nerve, may assist with the diagnosis [12]. Typically, the ultrasound examination may show flattening of the nerve within the tunnel and enlargement of the nerve proximal and distal to the tunnel. Pooling of recent articles seems to confirm that sonography using cross-sectional area of the median nerve could not be an alternative to electrodiagnostic testing for diagnosis of CTS but could give complementary results. Ultrasound examination should be considered in doubtful cases or secondary cases of CTS [13].
Others have advocated the injection of corticosteroids or bupivacaine into the carpal tunnel. If the injection is accompanied by a relief of symptoms, it provides diagnostic evidence of CTS [14].
A wrist radiograph may be helpful if a fracture or degenerative joint disease is suspected.
Blood tests should be ordered if underlying rheumatologic disease or endocrine disturbance is suspected. These include fasting blood glucose concentration, erythrocyte sedimentation rate, thyroid function, and rheumatoid factor.
Treatment
Initial
Once the diagnosis is established, treatment should begin with conservative management in patients with mild disease. Nighttime wrist splinting (Fig. 36.5) in a neutral position may help reduce or completely relieve CTS symptoms. Wrist splinting in neutral position may be more effective than in 20-degree extension in the short term [15]. Full-time use, if tolerable, has been shown to provide greater improvement of symptoms and electrophysiologic measures than night-only use [16]. Compliance with full-time use is more difficult [16]. Most patients will achieve maximal symptom relief through splinting within 2 to 3 weeks. If current treatment fails to resolve symptoms within 2 to 7 weeks, another nonsurgical treatment or surgery is suggested [17]. Nonsteroidal anti-inflammatory drugs are frequently prescribed as an adjunct to wrist splinting. However, studies have demonstrated that nonsteroidal anti-inflammatory drugs, vitamin B6, and diuretics are often no more effective than placebo in relieving the symptoms of CTS [15].

The use of oral steroids (prednisone in doses of 20 mg daily for the first week and 10 mg daily for the second week [18], or prednisolone at 25 mg daily for 10 days [19]) has proved to be of some benefit, although not as impressive as the results noted through injection (see later) [19]. However, the effectiveness of oral or injected steroids was not maintained in the long term [15].
Underlying conditions, such as hypothyroidism, rheumatoid arthritis, or diabetes, should be treated. Frequent periods of rest of the wrist should be prescribed, especially when vocational activities involve sustained positioning or repetitive and forceful flexion or extension of the wrist. Ice after periods of use may be effective for symptom relief. Positioning of the body while a task is being performed should be reviewed to relieve unnecessary strain as necessary motions are performed.
Rehabilitation
Rehabilitation must address the patterns of hand use, which exacerbates the symptoms of CTS in many individuals. Lifestyle modifications, including decreasing repetitive activity and using ergonomic devices, have been traditionally advocated but have inconsistent evidence to support their effectiveness. Occupational therapists can be helpful in instructing flexion and extension stretching of the wrist and forearm. Although many therapists advocate strengthening as part of a treatment program, aggressive strengthening exercises should be avoided until symptom relief is nearly complete.
Icing after long periods of use has been advocated to reduce the pain and swelling. In addition, it is important that patients be instructed in a program of general physical conditioning; generalized deconditioning exacerbates the symptoms of CTS [20].
There is no evidence for the effectiveness of postoperative splinting [15]. It is suggested that the wrist not be immobilized postoperatively after routine carpal tunnel surgery [17]. Active motion of the hand and wrist should start immediately postoperatively to prevent joint stiffness and to ensure adequate glide of the tendons and median nerve in the carpal tunnel. Passive range of motion should be initiated at least 4 weeks postoperatively for mobilization of stiff joints and tendons. Strengthening is initiated at 3 to 4 weeks as wounds heal and inflammation resolves [21].
On average, postsurgical patients were able to return to driving in 9 days, to activities of daily living in 13 days, and to work in 17 days [22].
Procedures
The patient can also be treated with corticosteroid injections into the carpal tunnel. A number of authors have suggested various injection techniques to avoid direct injury to the median nerve [23–26].
For injection into the carpal tunnel (Fig. 36.6), 1 mL of steroid (triamcinolone, 40 mg/mL) can be injected under sterile conditions. For delivery, one should use a 5⁄8-inch, 27-gauge needle, placing the needle proximal to the distal wrist crease and ulnar to the palmaris longus tendon. The needle should be directed dorsally and angled at 30 degrees to a depth of about 5⁄8 inch (the length of the needle) or contact with a flexor tendon. Slowly inject 1 mL of the corticosteroid. Anesthetics are not typically used in this injection unless for diagnostic verification. In individuals lacking a palmaris longus tendon (about 2% to 20% of the population), the needle can be placed midpoint between the ulna and radial styloid process. The injection will increase the volume of fluid within the carpal tunnel and thus may exacerbate the discomfort for a few hours; relief is expected within the 24 to 48 hours after injection. Although effectiveness is primarily short term, corticosteroid injection may be particularly useful to control the pain and to reduce symptoms for patients wishing to delay surgical treatment.
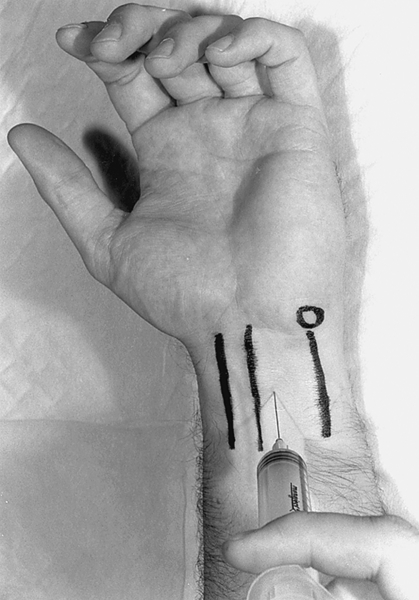
It has been reported that ultrasound-guided carpal tunnel injection improves the performance, clinical outcomes, and cost-effectiveness of injection of the carpal tunnel compared with conventional blind, palpation-guided injection in a single randomized controlled trial [27]. However, the exact role of ultrasound guidance for carpal tunnel injection is still arguable [28].
Surgery
Carpal tunnel release surgery should be considered in patients with symptoms that do not respond to conservative measures and for whom electrodiagnostic testing clearly confirms median neuropathy at the wrist. Surgery or another nonsurgical treatment is suggested when the current treatment fails to resolve symptoms within 2 to 7 weeks [17]. Six weeks to 3 months of conservative treatment is reasonable in patients with mild disease [29].
Early surgery is indicated when there are signs of atrophy or muscle weakness. The optimal timing of surgery in the natural history of CTS has not been established, although timing is an important factor for total recovery after surgery. A long-lasting compression could result in irreversible axonal damage, which would not improve despite surgical intervention [15]. Surgical treatment has been shown to lead to better outcome than nonsurgical treatment [30]. The primary reason for a poor result is an error in diagnosis.
The open release of the transverse carpal ligament represents the standard procedure and can be performed by dividing the transverse carpal ligament through a small open wrist incision. The reliability of and good visualization provided by the open technique continue to make it the preferred operation for many hand surgeons [31]. The endoscopic techniques were introduced in the late 1980s to be minimally invasive and to prevent the palmar scarring. Both methods have equal efficacy and provide excellent outcomes in relieving symptoms of CTS [32], with satisfaction rates up to 90%. Potential benefits of the endoscopic technique, including a more rapid functional recovery, must be weighed against the technique’s increased cost and higher complication rate [32].
Potential Disease Complications
As with any insult to a peripheral nerve, untreated CTS may result in chronic sensory disturbance or motor impairment in the area serviced by the median nerve. It is important that the clinician be wary of this and not allow the nerve disturbance to progress to permanent nerve damage.
Potential Treatment Complications
Although oral analgesics may be important for symptomatic relief early in the stages of CTS, gastric, renal, and hepatic complications of nonsteroidal anti-inflammatory drugs should be monitored. Complications from local corticosteroid injections include infection, bleeding, skin depigmentation, skin and fat atrophy, potential for tendon rupture, and potential for injury to the median nerve at the time of injection.
Surgical complications have been noted to be few in the literature. These include accidental transection of the median nerve, with permanent loss of function distal to the transection. In addition, some have suggested that endoscopic surgery might damage the Berrettini branch of the median nerve, a sensory branch [33]. Whereas complications of surgical intervention are thought to be relatively infrequent, a number have been reported. The most common complication of surgical intervention is the incomplete sectioning of the transverse carpal ligament. Other potential complications include injury to the median nerve, palmar cutaneous branch, recurrent motor branch, and superficial palmar arch; hypertrophied or thickened scar due to inappropriate incision; tendon adhesions because of wound hematoma; recurrence because of repair of the ligament; bowstringing of flexor tendons; malposition of the median nerve; inappropriate separation of the nerve fibers from surrounding scars; pillar pain; and reflex sympathetic dystrophy.







