CHAPTER 35 Valvular Heart Disease
2 Describe common findings of the history and physical examination in patients with valvular heart disease
3 Which tests are useful in the evaluation of valvular heart disease?
Echocardiography is recommended for:
 Asymptomatic patients with diastolic murmurs, continuous murmurs, holosystolic murmurs, grade 3 or louder mid-peaking systolic murmurs, late systolic murmurs, murmurs associated with ejection clicks, or murmurs that radiate to the neck or back.
Asymptomatic patients with diastolic murmurs, continuous murmurs, holosystolic murmurs, grade 3 or louder mid-peaking systolic murmurs, late systolic murmurs, murmurs associated with ejection clicks, or murmurs that radiate to the neck or back.7 How does a normal pressure-volume loop appear?
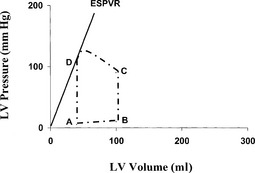
The AB segment is ventricular filling, BC is isovolumic contraction, CD is ejection, and DA is isovolumic relaxation. D point represents the aortic valve closing, A the mitral valve (MV) opening, B the MV closing, and C the aortic valve opening. Stroke volume through the aortic valve is the distance between C and D points. End-systolic volume can be measured at the D point, and end-diastolic volume can be measured at the B point. The end-systolic pressure–volume relationship slope is a measure of contractility. A horizontal-clockwise shift of the slope represents a decrease in contractility (Figure 35-1).
9 How can be the severity of aortic stenosis characterized by echocardiography?
AS severity is graded on the basis of a variety of hemodynamic and natural history data using definitions of valve area, mean pressure gradient, and aortic jet velocity (Table 35-1).
| Mild | Severe | |
|---|---|---|
| Aortic valve area (cm2) | >1.5 | <1 |
| Mean aortic valve pressure gradient (mm Hg) | <25 | >40 |
| Aortic jet velocity (m/s) | <3 | >4 |
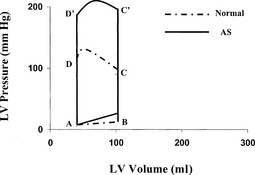
11 How are the compensatory changes in the left ventricle represented by a pressure-volume loop?
Because of the AS, the left ventricle is working with higher intraventricular pressures to generate a normal stroke volume. The higher systolic wall tension initiates myocardial thickening and LV hypertrophy (LVH). The hypertrophied left ventricle has increased contractility to accomplish the pressure work (Figure 35-2). LVH decreases the wall tension during systole, improving the relationship of systolic work to oxygen demand. As the AS increases, LV systolic pressure increases to the level at which LVH cannot normalize the wall tension. At this point the heart starts dilating, resulting in systolic dysfunction and decreasing CO.
14 Discuss the pathophysiology of aortic insufficiency
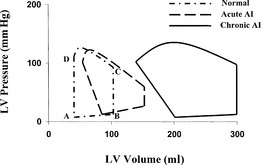
In chronic aortic insufficiency (AI) there is an LV diastolic volume overload because part of the stroke volume regurgitates across the incompetent aortic valve during diastole. Patients have large end-diastolic and stroke volumes. The volume load generates high wall tension in diastole, initiating eccentric hypertrophy (dilated left ventricle with normal or thickened wall). Increasing regurgitant orifice area, slow heart rate (relatively more time spent in diastole) and increased systemic vascular resistance increase the amount of regurgitant flow. Compliance and stroke volume may be markedly increased in chronic AI, whereas contractility gradually diminishes (Figure 35-3). AI can be caused by diseased valve leaflets or enlargement of the aortic root. In the developing world the most common cause of AI is rheumatic heart disease. In developed countries AI is most often caused by aortic root dilation, congenital bicuspid aortic valve, or infective endocarditis. Causes of acute AI are infective endocarditis, aortic dissection (Marfan syndrome), and AI after aortic balloon valvotomy or a failed surgical valve repair.
Ideally patients with chronic AI should have valve replacement surgery before the onset of irreversible myocardial damage. In acute AI the left ventricle is subjected to rapid, massive volume overload with elevated end-diastolic pressure. Hypotension and pulmonary edema may necessitate emergent valvular replacement (see Figure 35-3).
15 What parameters can be used in echocardiography to characterize the severity of aortic insufficiency?
| Mild | Severe | |
|---|---|---|
| Color Doppler jet width (% of LVOT diameter) | <25 | >65 |
| Color Doppler vena contracta (cm) | <0.3 | >0.6 |
| Regurgitant volume (ml) | <30 | ≥60 |
| Regurgitant fraction (%) | <30 | ≥50 |
| Regurgitant orifice area (cm2) | <0.1 | ≥0.3 |
| Left ventricle size | Normal | Increased |
LVOT, Left ventricular outflow tract.
16 What is the indication for aortic valve replacement in aortic stenosis?
 Asymptomatic patients with chronic severe AI and LV systolic dysfunction (ejection fraction 50% or less) at rest
Asymptomatic patients with chronic severe AI and LV systolic dysfunction (ejection fraction 50% or less) at rest17 What does the pressure-volume loop look like in acute and chronic aortic insufficiency?
In acute AI the end-diastolic and end-systolic volume is increasing. The stroke volume can be increased, normal, or decreased, depending on the severity of AI. The LV volume is increasing during the isovolumic relaxation period. The end-diastolic pressure is high. End-diastolic pressure >25 to 30 mm Hg manifests as pulmonary edema. Contractility is decreased because the myocardium is overstretched. There is no diastolic reserve, thus the heart cannot increase the stroke volume with increasing preload or afterload (see Figure 35-3).
In chronic AI the end-diastolic, end-systolic and stroke volumes are enlarged. Cardiac output is normal, although the contractility is decreased. Despite the enlarged LV end-diastolic volume, the end-diastolic pressure is normal; thus the heart has diastolic reserve to increase the stroke volume with increasing preload or afterload (see Figure 35-3).
18 What are the hemodynamic goals in the anesthetic management of patients with aortic insufficiency?
19 Discuss the hemodynamic changes in patients with aortic insufficiency after aortic valve replacement
21 What parameters can be used in echocardiography to characterize the severity of mitral stenosis?
| Mild | Severe | |
|---|---|---|
| Mean mitral valve pressure gradient (mm Hg) | <5 | >10 |
| Valve area (cm2) | >1.5 | <1 |
| Pulmonary artery systolic pressure (mm Hg) | <30 | >50 |
22 What is the indication for mitral valve replacement in mitral stenosis?
Based on the ACC/AHA 2006 guidelines, MV surgery is indicated in the following patients:
 MV surgery (repair if possible) is indicated in patients with symptomatic moderate or severe MS (NYHA functional class III–IV) when:
MV surgery (repair if possible) is indicated in patients with symptomatic moderate or severe MS (NYHA functional class III–IV) when:
23 How is the pressure-volume loop changed from normal in mitral stenosis?
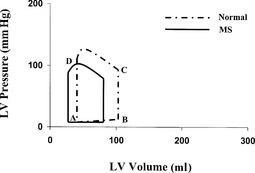
The end-diastolic, end-systolic, and stroke volume are small because of the limited flow into the LV. The LV generates low blood pressure. The contractility is decreased because of chronic underfilling of the left ventricle (Figure 35-4).
25 Discuss the postoperative management of patients with mitral stenosis after mitral valve replacement
27 What parameters can be used in echocardiography to characterize the severity of mitral regurgitation?
| Mild | Severe | |
|---|---|---|
| Color Doppler jet area (cm2) | <4 | >8.0 |
| Color Doppler jet area (% of left atrium) | <20 | >40 |
| Color Doppler vena contracta (cm) | <0.3 | >0.7 |
| Regurgitant volume (ml) | <30 | ≥60 |
| Regurgitant fraction (%) | <30 | ≥50 |
| Regurgitant orifice area (cm2) | <0.1 | ≥0.3 |
| Left atrial end ventricular size | Normal | Enlarged |
28 What is the indication for mitral valve replacement in mitral regurgitation?
Based on the ACC/AHA 2006 guidelines, MV surgery is indicated in the following patients:
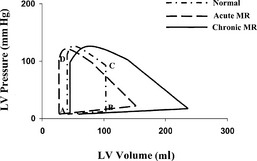
29 How is the pressure-volume loop in mitral regurgitation changed from normal?
In acute MR the end-diastolic volume increases with high end-diastolic pressure. End-systolic volume is normal or decreased, stroke volume is increased, but the ejected volume into the aorta is relatively small, depending on the regurgitant volume (Figure 35-5).
In chronic MR the end-diastolic volume is increased with normal end-diastolic pressure resulting from the chronic myocardial remodeling process. The end-systolic volume is normal. The markedly increased stroke volume preserves the forward CO despite the significant regurgitation. The contractility is decreased (see Figure 35-5).
KEY POINTS: Valvular Heart Disease 
31 Discuss the hemodynamic management after mitral valve repair or replacement in patient with mitral regurgitation
1. Bonow R.O., Carabello B.A., Chatterjee K., et al. ACC/AHA Guidelines for the Management of patients with valvular heart disease. Circulation. 2006;114:450-527.
2. Sukernik M., Martin D.E. Anesthetic management for the treatment of valvular heart diseases. In: Hensley F.A., Martin D.E., Gravlee G.P., editors. A practical approach to cardiac anesthesia. ed 4. Philadelphia: Lippincott Williams & Wilkins; 2008:316-347.