Procedure 35 Silicone Metacarpophalangeal Joint Arthroplasty
![]() See Video 27: Silicone Metacarpophalangeal Joint Replacement Arthoplasty for Rheumatoid Arthritis
See Video 27: Silicone Metacarpophalangeal Joint Replacement Arthoplasty for Rheumatoid Arthritis
Examination/Imaging
Clinical Examination
 The patient’s MCP joints should be evaluated for range of motion and stability. If the MCP joints are not dislocated but the fingers are drifted ulnarly, intrinsic transfer may be performed to correct the finger misalignment for the small, ring, and long fingers; the radial sagittal band of the index finger is tightened to centralize its extensor tendon because no ulnar intrinsic tendon is available for transfer.
The patient’s MCP joints should be evaluated for range of motion and stability. If the MCP joints are not dislocated but the fingers are drifted ulnarly, intrinsic transfer may be performed to correct the finger misalignment for the small, ring, and long fingers; the radial sagittal band of the index finger is tightened to centralize its extensor tendon because no ulnar intrinsic tendon is available for transfer.
 With chronic subluxation of the MCP joints, ligamentous contracture around the joints cannot be corrected by soft tissue reconstruction alone. MCP joint arthroplasty is the preferred option in most of these cases.
With chronic subluxation of the MCP joints, ligamentous contracture around the joints cannot be corrected by soft tissue reconstruction alone. MCP joint arthroplasty is the preferred option in most of these cases.
 The thumb MCP joint laxity should be assessed, which is best treated with MCP joint fusion at the time of silicone MCP arthroplasty (SMPA).
The thumb MCP joint laxity should be assessed, which is best treated with MCP joint fusion at the time of silicone MCP arthroplasty (SMPA).
 For patients who have collapse of the wrists and radial deviation of the metacarpals, the wrist problem should be addressed first either by fusion or by arthroplasty. Otherwise, the radial deviation of the metacarpals will cause early postoperative ulnar subluxation of the fingers after SMPA. Realigning the metacarpals by means of the wrist procedures will enhance the outcome of SMPA.
For patients who have collapse of the wrists and radial deviation of the metacarpals, the wrist problem should be addressed first either by fusion or by arthroplasty. Otherwise, the radial deviation of the metacarpals will cause early postoperative ulnar subluxation of the fingers after SMPA. Realigning the metacarpals by means of the wrist procedures will enhance the outcome of SMPA.
Surgical Anatomy
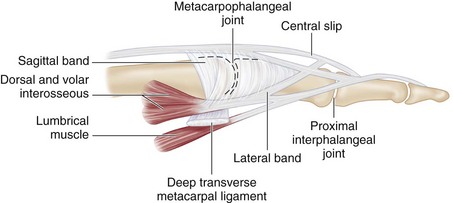
 The MCP joint is a condylar joint that allows flexion and extension but also radial and ulnar deviation.
The MCP joint is a condylar joint that allows flexion and extension but also radial and ulnar deviation.
 The radial and ulnar sagittal bands stabilize the extensor tendon, keeping it over the dorsal midline of the MCP joint. The sagittal bands are attached to the volar plate.
The radial and ulnar sagittal bands stabilize the extensor tendon, keeping it over the dorsal midline of the MCP joint. The sagittal bands are attached to the volar plate.
 The lateral bands pass volar to the MCP joint and dorsal to the proximal interphalangeal (PIP) joint. Contraction of the intrinsic muscles through the lateral bands causes MCP joint flexion and PIP joint extension (Fig. 35-1).
The lateral bands pass volar to the MCP joint and dorsal to the proximal interphalangeal (PIP) joint. Contraction of the intrinsic muscles through the lateral bands causes MCP joint flexion and PIP joint extension (Fig. 35-1).
 The cause of tendon subluxation at the MCP joint in RA is joint synovitis altering the ligamentous support in the joint. The hypertrophic synovial tissue distends the ligamentous support of the joint, resulting in stretching of the radial and ulnar sagittal bands. Forceful gripping in daily activity tasks stresses the radial sagittal band, resulting in weakening of the radial support.
The cause of tendon subluxation at the MCP joint in RA is joint synovitis altering the ligamentous support in the joint. The hypertrophic synovial tissue distends the ligamentous support of the joint, resulting in stretching of the radial and ulnar sagittal bands. Forceful gripping in daily activity tasks stresses the radial sagittal band, resulting in weakening of the radial support.
 Progressive ulnar subluxation of the extensor tendons causes the ulnar drift seen in RA hands.
Progressive ulnar subluxation of the extensor tendons causes the ulnar drift seen in RA hands.
 Chronic ulnar subluxation of the extensor mechanism results in ulnar lateral band contracture, which eventually causes fixed contracture of the ulnar lateral bands.
Chronic ulnar subluxation of the extensor mechanism results in ulnar lateral band contracture, which eventually causes fixed contracture of the ulnar lateral bands.
Exposures
Procedure
Step 1
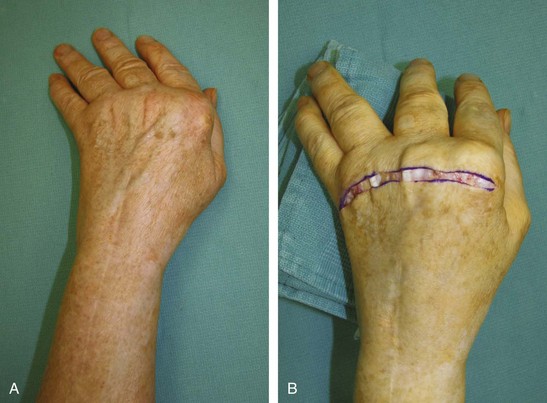
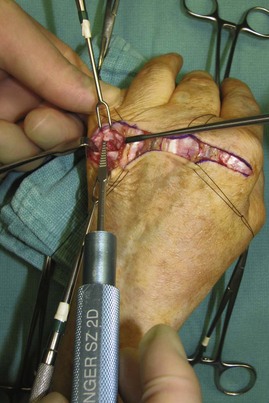
 The radial sagittal bands are incised to expose the MCP joints, and synovial tissues are sharply excised from the joints (see Fig. 35-3, sagittal band incision marked by dotted line).
The radial sagittal bands are incised to expose the MCP joints, and synovial tissues are sharply excised from the joints (see Fig. 35-3, sagittal band incision marked by dotted line).
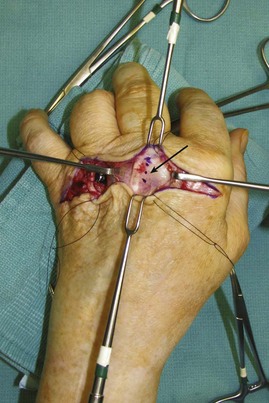
 The collateral ligaments are divided at the metacarpal neck, and heads of the metacarpals are resected at the proximal origin of the collateral ligament using an oscillating saw (Fig. 35-4). After metacarpal head resections, the fingers can be brought into alignment. Resection of the heads should decrease the tightness of the ulnar intrinsic tendons that contribute to ulnar deviation of the fingers. Therefore, ulnar lateral band release is usually not necessary, if sufficient resection of the head of the metacarpal is performed.
The collateral ligaments are divided at the metacarpal neck, and heads of the metacarpals are resected at the proximal origin of the collateral ligament using an oscillating saw (Fig. 35-4). After metacarpal head resections, the fingers can be brought into alignment. Resection of the heads should decrease the tightness of the ulnar intrinsic tendons that contribute to ulnar deviation of the fingers. Therefore, ulnar lateral band release is usually not necessary, if sufficient resection of the head of the metacarpal is performed.
Step 2
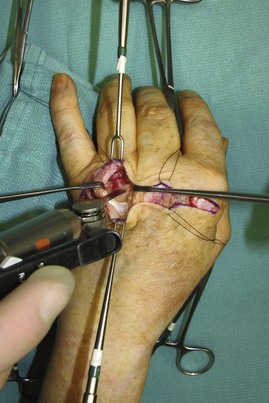
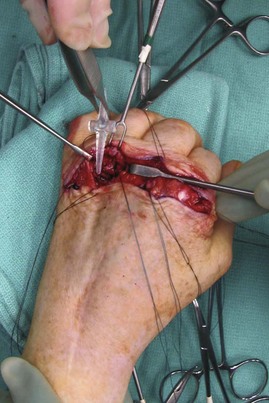
 An awl is used to perforate the medullary cavities of the metacarpals and proximal phalanges (Fig. 35-5). Typically, the medullary cavities of the metacarpals are devoid of bone and are easily broached.
An awl is used to perforate the medullary cavities of the metacarpals and proximal phalanges (Fig. 35-5). Typically, the medullary cavities of the metacarpals are devoid of bone and are easily broached.
Step 3
 Sequential-sized broaches are used to enlarge the medullary cavity. The largest implants that will fit into the medullary cavity are inserted. Unlike the awl, which should be inserted in a twisting motion to enlarge the medullary cavity, the broach is rectangular in shape and should be inserted straight, without twisting, to make a square trough to accommodate the shape of the silicone implant ends (Fig. 35-6).
Sequential-sized broaches are used to enlarge the medullary cavity. The largest implants that will fit into the medullary cavity are inserted. Unlike the awl, which should be inserted in a twisting motion to enlarge the medullary cavity, the broach is rectangular in shape and should be inserted straight, without twisting, to make a square trough to accommodate the shape of the silicone implant ends (Fig. 35-6).
Step 3 Pearls
The medullary canals of the proximal phalanges should be prepared first because these usually determine the implant size to be used. The exception to this is the ring metacarpal, which typically has a narrower canal than the ring finger proximal phalanx and should therefore be prepared first to avoid over-reaming the proximal phalanx.
Step 4
Step 5
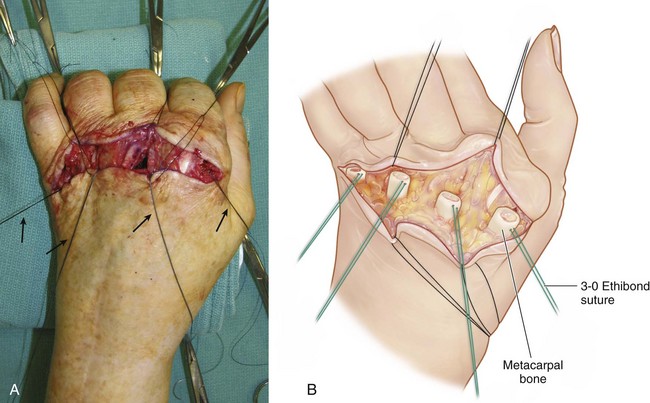
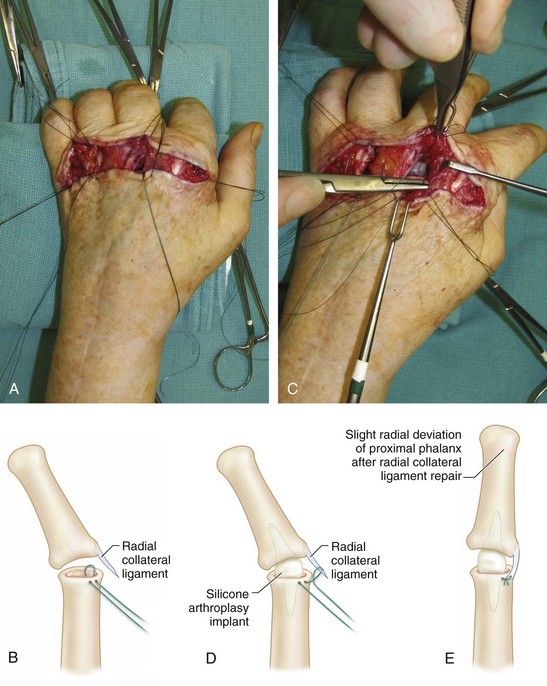
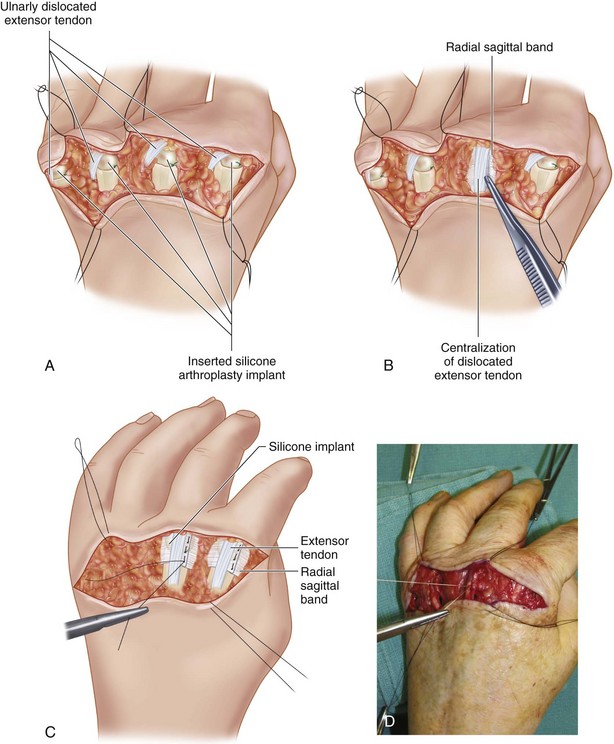
 The implants are inserted (Fig. 35-8), and the radially placed 3-0 braided sutures are used to reattach the radial collateral ligament and bring the fingers into slight radial deviation (Fig. 35-9A to E). The ulnar lateral bands can be released, if they are still tight and cause the fingers to deviate ulnarly. However, as stated previously, ulnar band release is usually not necessary.
The implants are inserted (Fig. 35-8), and the radially placed 3-0 braided sutures are used to reattach the radial collateral ligament and bring the fingers into slight radial deviation (Fig. 35-9A to E). The ulnar lateral bands can be released, if they are still tight and cause the fingers to deviate ulnarly. However, as stated previously, ulnar band release is usually not necessary.
Step 6
Step 7
 The tourniquet is released, and all bleeding points are cauterized. A drain is typically not necessary. The wound is then closed with interrupted absorbable dermal sutures, and the skin is closed with 4-0 horizontal mattress nylon sutures (Fig. 35-11). The hand is immobilized in a volar resting short-arm splint.
The tourniquet is released, and all bleeding points are cauterized. A drain is typically not necessary. The wound is then closed with interrupted absorbable dermal sutures, and the skin is closed with 4-0 horizontal mattress nylon sutures (Fig. 35-11). The hand is immobilized in a volar resting short-arm splint.
Postoperative Care and Expected Outcomes
 One week after surgery, the patient is placed in a dynamic extension splint. The patient will initiate active flexion exercises while in this dynamic splint for 6 weeks. A hand therapist will evaluate the patient’s progress weekly, and the splint is adjusted as necessary to align the fingers.
One week after surgery, the patient is placed in a dynamic extension splint. The patient will initiate active flexion exercises while in this dynamic splint for 6 weeks. A hand therapist will evaluate the patient’s progress weekly, and the splint is adjusted as necessary to align the fingers.
 Studies have shown that static extension splints may work just as well as dynamic extension splints. However, we have no experience with the static protocol. Patients will typically gain about 30 to 40 degrees of active motion at the MCP joint, favoring an extended arc of motion.
Studies have shown that static extension splints may work just as well as dynamic extension splints. However, we have no experience with the static protocol. Patients will typically gain about 30 to 40 degrees of active motion at the MCP joint, favoring an extended arc of motion.
Chung KC, Kotsis SV, Kim HM. A prospective outcomes study of Swanson metacarpophalangeal joint arthroplasty for the rheumatoid hand. J Hand Surg [Am]. 2004;29:646-653.
Chung KC, Kotsis SV, Kim HM, et al. Reasons why rheumatoid arthritis patients seek surgical treatment for hand deformities. J Hand Surg [Am]. 2006;31:289-294.
Chung KC, Kotsis SV, Wilgis EF, et al. Outcomes of silicone arthroplasty for rheumatoid metacarpophalangeal joints stratified by fingers. J Hand Surg [Am]. 2009;34:1647-1652.
Chung KC, Kowalski CP, Kim HM, Kazmers IS. Patient outcomes following Swanson Silastic metacarpophalangeal arthroplasty in the rheumatoid hand: systematic overview. J Rheumatol. 2000;27:1395-1402.