Procedure 34 Reconstruction of the Central Slip with the Transverse Retinacular Ligament for Boutonnière Deformity
![]() See Video 26: Correction of Boutonnière Deformity
See Video 26: Correction of Boutonnière Deformity
Indications
 Boutonnière deformity is classified into three stages by Nalebuff, as follows:
Boutonnière deformity is classified into three stages by Nalebuff, as follows:
 Indication: Boutonnière deformity of the PIP joint with almost full passive extension (stages 1 and 2) is suitable for this reconstructive surgery.
Indication: Boutonnière deformity of the PIP joint with almost full passive extension (stages 1 and 2) is suitable for this reconstructive surgery.
 Contraindication: If articular destruction is evident or if a severe fixed flexion contracture is present (stage 3), arthrodesis or arthroplasty of the PIP joint is recommended.
Contraindication: If articular destruction is evident or if a severe fixed flexion contracture is present (stage 3), arthrodesis or arthroplasty of the PIP joint is recommended.
Examination/Imaging
Clinical Examination
 Boutonnière deformity is seen in a patient with rheumatoid arthritis (Fig. 34-1).
Boutonnière deformity is seen in a patient with rheumatoid arthritis (Fig. 34-1).
 Passive PIP joint extension should always be evaluated before surgical reconstruction.
Passive PIP joint extension should always be evaluated before surgical reconstruction.
 The mobility of the PIP joint is very important for obtaining good results. Therefore, in the case of the boutonnière deformity with severe flexion contracture of the PIP joint, rehabilitation or joint splinting in extension of the PIP joint should be performed before the operation.
The mobility of the PIP joint is very important for obtaining good results. Therefore, in the case of the boutonnière deformity with severe flexion contracture of the PIP joint, rehabilitation or joint splinting in extension of the PIP joint should be performed before the operation.
Imaging
 Radiographic examination is required to evaluate the status of the metacarpophalangeal (MCP), proximal interphalangeal (PIP), and distal interphalangeal (DIP) joints.
Radiographic examination is required to evaluate the status of the metacarpophalangeal (MCP), proximal interphalangeal (PIP), and distal interphalangeal (DIP) joints.
 If the PIP joint is destroyed, arthrodesis or arthroplasty is recommended.
If the PIP joint is destroyed, arthrodesis or arthroplasty is recommended.
 Magnetic resonance imaging examination may help to identify synovitis of the PIP joint.
Magnetic resonance imaging examination may help to identify synovitis of the PIP joint.
Surgical Anatomy
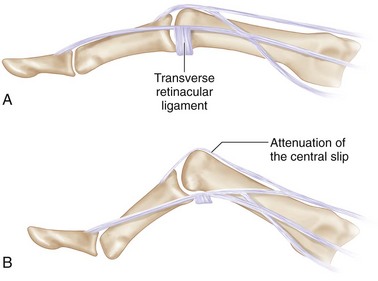
 Disruption of the central slip of the extensor tendon results in palmar migration of the lateral bands with PIP joint flexion. Proximal displacement of the extensor apparatus results in the DIP joint hyperextension deformity (Fig. 34-2A is normal; B shows boutonnière deformity).
Disruption of the central slip of the extensor tendon results in palmar migration of the lateral bands with PIP joint flexion. Proximal displacement of the extensor apparatus results in the DIP joint hyperextension deformity (Fig. 34-2A is normal; B shows boutonnière deformity).
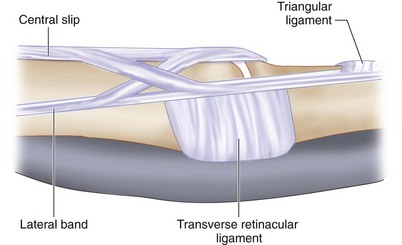
 The transverse retinacular ligament is the key component in this procedure. This ligament holds the lateral bands in the palmar direction during flexion. It inserts into the palmar plate of the PIP joint and flexor tendon sheath (Fig. 34-3).
The transverse retinacular ligament is the key component in this procedure. This ligament holds the lateral bands in the palmar direction during flexion. It inserts into the palmar plate of the PIP joint and flexor tendon sheath (Fig. 34-3).
Exposures
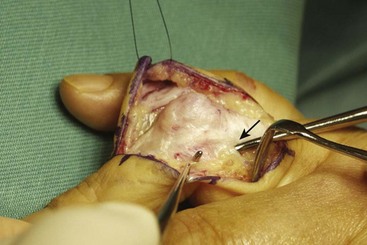
 Extensor apparatus is approached through a dorsal curved incision over the PIP joint. The dissection is carried down to the extensor hood, preserving the dorsal venous system (Fig. 34-4).
Extensor apparatus is approached through a dorsal curved incision over the PIP joint. The dissection is carried down to the extensor hood, preserving the dorsal venous system (Fig. 34-4).
Procedure
Step 1
 Both lateral bands and transverse retinacular ligaments are identified first. The central slip is usually attenuated or ruptured, and the capsule of the PIP joint appears directly under the fat tissue. In Figure 34-5, the black arrow shows the transverse retinacular ligament.
Both lateral bands and transverse retinacular ligaments are identified first. The central slip is usually attenuated or ruptured, and the capsule of the PIP joint appears directly under the fat tissue. In Figure 34-5, the black arrow shows the transverse retinacular ligament.
 The radial and ulnar transverse retinacular ligaments are cleanly separated from their insertions at the palmar plate.
The radial and ulnar transverse retinacular ligaments are cleanly separated from their insertions at the palmar plate.
Step 1 Pearls
If there is a contracture of the PIP joint, the surgeon should cut the accessory collateral ligament and release the volar plate at the proximal portion to obtain full passive extension of the PIP joints.
Removing adhesion of the lateral band and cutting the oblique retinacular ligament may be necessary to obtain flexion of the DIP joint.
Synovectomy of the PIP joint should be performed for patients with active rheumatoid arthritis.
Step 2
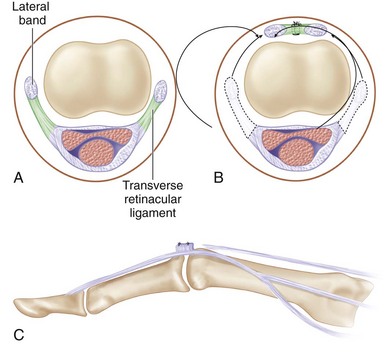
 The transverse retinacular ligaments are turned over onto the dorsal aspect on the PIP joint to lift the lateral band dorsally and are then sutured to one another (Fig. 34-6).
The transverse retinacular ligaments are turned over onto the dorsal aspect on the PIP joint to lift the lateral band dorsally and are then sutured to one another (Fig. 34-6).
 Tension of the suture is determined by noting the nearly full active extension of the PIP joint (Fig. 34-7).
Tension of the suture is determined by noting the nearly full active extension of the PIP joint (Fig. 34-7).
Step 3
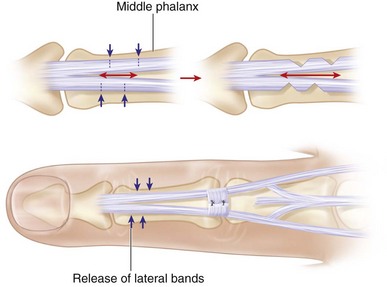
 Check active flexion of the DIP joint because the tension of the lateral band is tighter after suturing of the transverse retinacular ligaments (Fig. 34-9).
Check active flexion of the DIP joint because the tension of the lateral band is tighter after suturing of the transverse retinacular ligaments (Fig. 34-9).
 If DIP joint flexion is limited, releasing the lateral band between the PIP and DIP joints is recommended.
If DIP joint flexion is limited, releasing the lateral band between the PIP and DIP joints is recommended.
 Make small transverse cuts in the lateral band until the DIP joint can be actively flexed at 30 degrees (Fig. 34-10).
Make small transverse cuts in the lateral band until the DIP joint can be actively flexed at 30 degrees (Fig. 34-10).
 After the operation, the PIP joint is immobilized in full extension with a Kirschner wire or volar splint for about 14 days.
After the operation, the PIP joint is immobilized in full extension with a Kirschner wire or volar splint for about 14 days.
Postoperative Care and Expected Outcomes
 Active flexion exercises of the DIP joint are started within 3 days while the PIP joint remains immobilized.
Active flexion exercises of the DIP joint are started within 3 days while the PIP joint remains immobilized.
 About 14 days after surgery, active flexion exercises of the PIP joint are gently started, but active extension exercises of the PIP joint should be avoided at the early stages.
About 14 days after surgery, active flexion exercises of the PIP joint are gently started, but active extension exercises of the PIP joint should be avoided at the early stages.
 The PIP joint is held in full extension in the daytime by a dynamic splint and at night by a static splint for several weeks.
The PIP joint is held in full extension in the daytime by a dynamic splint and at night by a static splint for several weeks.
 After removing the splint, active finger exercises are started gradually.
After removing the splint, active finger exercises are started gradually.
Kato H, Uchiyama S, Yamazaki H, et al. Treatment for boutonnière deformity in rheumatoid arthritis [Japanese]. Kansetsugeka. 2008;27:58-63.
Nalebuff EA, Millender LH. Surgical treatment of the boutonnière deformity in rheumatoid arthritis. Orthop Clinic North Am. 1975;6:753-763.
Ohshio I, Ogino T, Minami A, et al. Reconstruction of the central slip by the transverse retinacular ligament for boutonnière deformity. J Hand Surg [Br]. 1990;15:407-409.
Salvi V. Technique for the buttonhole deformity. Hand. 1969;1:96-97.