CASE 33 Dissection of Both a Left Internal Mammary Graft and the Subclavian Artery
Cardiac catheterization
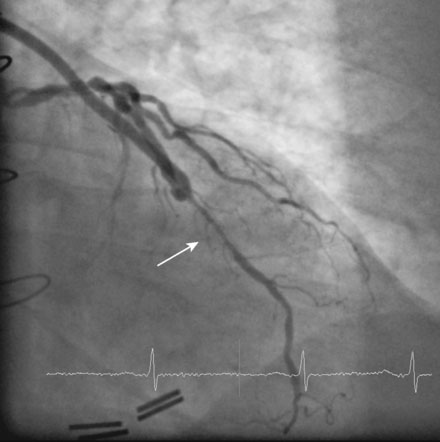
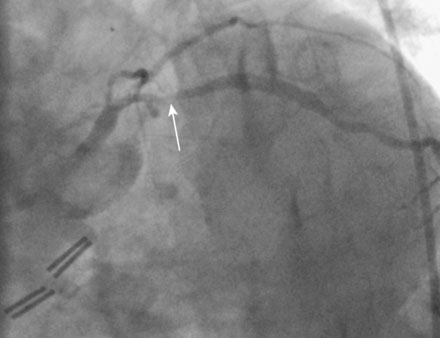
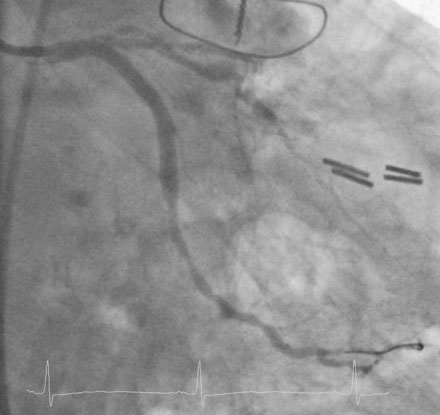
An elective diagnostic coronary angiogram found no significant obstructive disease in the right coronary artery. The left internal mammary artery graft was widely patent but there was severe narrowing within the stent placed 8 years earlier (Figure 33-1 and Video 33-1). In addition, there was obstructive narrowing of the left circumflex artery proximal to an old stent (Figure 33-2) and chronic occlusion of the proximal left anterior descending artery. Based on these findings, the operator planned to treat the circumflex lesion and then the in-stent restenosis in the native left anterior descending artery, to be accessed via the left internal mammary artery graft using bivalirudin as the procedural anticoagulant. The circumflex lesion responded well to balloon dilatation followed by placement of a 3.5 mm diameter by 23 mm long everolimus-eluting stent (Figure 33-3).
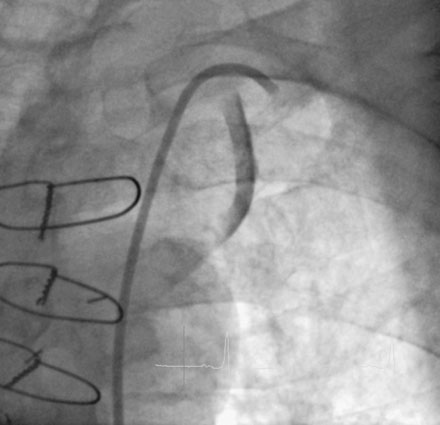
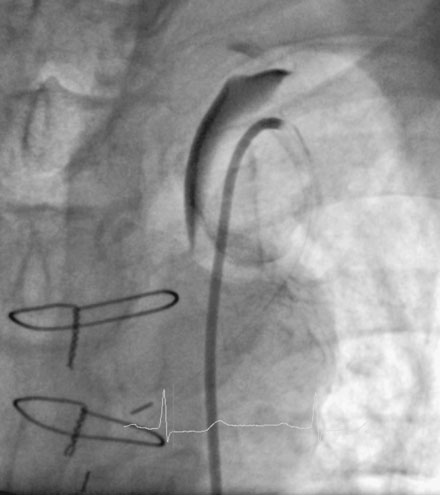
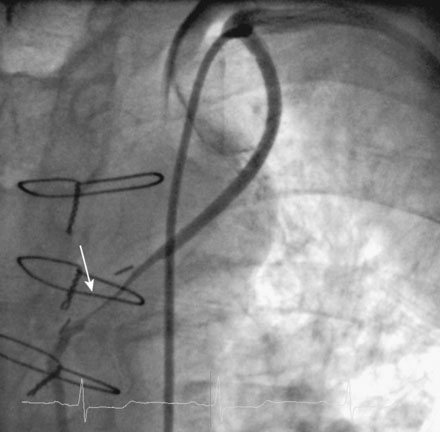
Once satisfied with the circumflex artery, the operator placed a 6 French left internal mammary guide catheter into the left subclavian, but noted contrast staining from the diagnostic angiogram still present in the proximal portion of the left internal mammary artery (Figure 33-4 and Video 33-2). A dissection of the proximal left internal mammary artery graft was suspected, and the guide catheter was cautiously engaged to allow further delineation of the dissection (Video 33-3). At this point, the subclavian artery did not appear to be involved, and the operator advanced a 0.014 inch floppy-tipped guidewire through the mammary artery and into the left anterior descending artery. With additional contrast injections, however, staining of the subclavian artery was noted, confirming that the dissection likely involved the ostium of the internal mammary artery, extending into the subclavian artery (Figure 33-5 and Video 33-4).
Numerous bare-metal stents were deployed within the left internal mammary artery graft, ultimately requiring a total length of 118 mm to cover the entire dissected area (Figure 33-6 and Videos 33-4, 33-5). Once the operator was satisfied with the repair of the left internal mammary artery graft, attention was turned to the subclavian artery. Angiography confirmed a dissection flap, but this remained stable throughout the procedure, did not compromise the origin of the vertebral artery (Figures 33-7, 33-8 and Videos 33-6, 33-7), and did not result in a pressure gradient across the dissected segment. Because the entry site of the intimal flap was opposite the direction of blood flow, it was decided to treat this dissection conservatively and the procedure was halted.
Discussion
The subclavian dissection added further to the operator’s quandary. This complication is very rare.1 Although a stent could have been placed at the site of the subclavian tear,2 the operator was concerned about the dissection’s close proximity to both the vertebral and left internal mammary arteries and feared jeopardizing or “jailing” these important branches. The decision to treat the subclavian dissection conservatively was based on two important observations. First, there was no pressure gradient measurable across the subclavian dissection, indicating that the dissection did not create significant luminal obstruction. Second, the direction of blood flow was opposite the direction of the entry flap, thereby making it unlikely that the dissection would extend. This strategy proved successful, based on the imaging study performed the next day demonstrating no evidence of the subclavian dissection.
1 Frohwein S., Ververis J.J., Marshall J.J. Subclavian artery dissection during diagnostic cardiac catheterization: The role of conservative management. Catheter Cardiovasc Diagn. 1995;34:313-317.
2 Galli M., Goldberg S.L., Zerboni S., Almagor Y. Balloon expandable stent implantation after iatrogenic arterial dissection of the left subclavian artery. Catheter Cardiovasc Diagn. 1995;35:355-357.