CASE 33
History: A 48-year-old man presents with epigastric pain.
1. Which of the following should be included in the differential diagnosis of the dominant imaging finding? (Choose all that apply.)
2. What is the most common benign submucosal tumor of the stomach?
3. How is a malignant tumor (leiomyosarcoma) distinguished from a benign stromal tumor (leiomyoma)?
D. Mitotic activity on pathology
4. What congenital abnormality can mimic a leiomyoma?
A. Gastric fundal diverticulum
ANSWERS
CASE 33
Large Gastrointestinal Stromal Tumor of the Stomach
1. B, C, and D
2. C
3. B
4. D
References
Darnell A, Dalmau E, Pericay C, et al: Gastrointestinal stromal tumors. Abdom Imaging. 2006;31:387–399.
Cross-Reference
Gastrointestinal Imaging: THE REQUISITES, 3rd ed, pp 76-77.
Comment
Smooth muscle or gastrointestinal stromal tumors (GISTs) are among the more commonly encountered tumors of the stomach. They account for almost half of all benign stomach tumors. Only a small percentage (less than 10%) are malignant. Benign GISTs occur equally among men and women, whereas malignant GISTs are more common in men. There tends to be a slight increase in the number of tumors with increasing age.
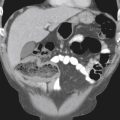
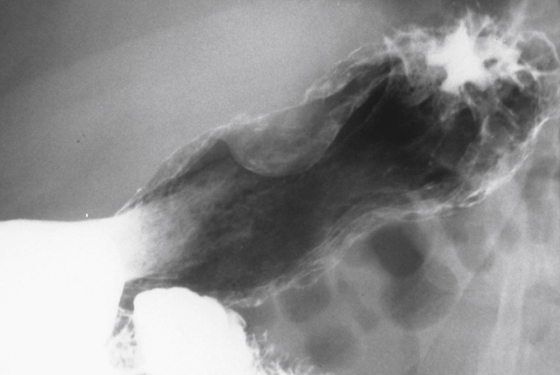
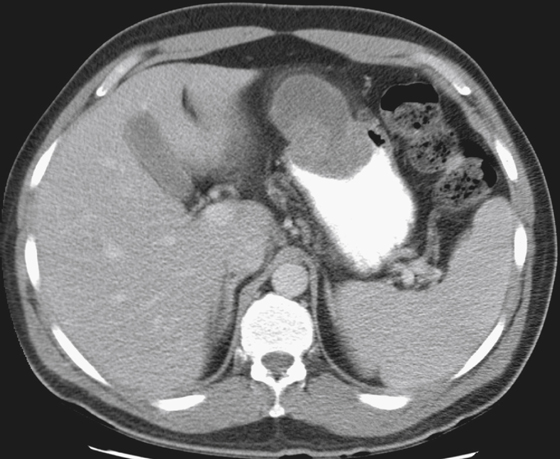
It is difficult to radiologically distinguish between benign and malignant GISTs and other submucosal tumors (see figures). The benign GIST can be found anywhere in the stomach, whereas its sarcomatous counterpart is usually more proximal. The pattern of growth is variable. The majority of both types of lesions grow endogastrically, or into the lumen. However, a small but significant percentage grow exophytically, or into the perigastric abdominal cavity, creating only a mild extrinsic mass impression on the stomach. This growth is fairly unusual but should be considered whenever a large intra-abdominal mass with growth into the abdominal cavity is encountered in the vicinity of the stomach. The tumors that grow into the lumen can ulcerate and can be large or even, rarely, multiple. Because these tumors are vascular, ulceration over the stretched and thinned mucosa can occur, and patients can present with a GI bleed.
Distinguishing benign from malignant smooth muscle tumors is difficult even for the pathologist. The classic criterion has been the number of mitotic figures visible per high-power field (more than 10 for malignant GIST). However, the nature of the histologic activity of the tumor is variable in different parts, and sampling can have a significant impact on the mitotic activity and pleomorphism viewed by the pathologist. Some believe that size of the tumor is just as important. Tumors less than 5 cm in diameter are more likely to be malignant.
Finally, the absolute criterion is evidence of metastatic disease. If the lesion is indeterminate based on pathologic findings, CT often becomes an absolute necessity to determine the exact nature of the tumor (see figures).