CASE 33
A 22-year-old man is admitted to the intensive care unit (ICU) in severe respiratory distress. This unfortunate fellow was diagnosed with chronic myelogenous leukemia (CML) 6 months ago. His doctors advised both him and his family that a bone marrow transplant offered the only chance of cure. Extensive searching of relatives who were prepared to donate marrow failed to find a good match. However, searching the bone marrow transplant registry revealed one donor matched for all class I and II disparities. Transplant was performed 5 months earlier, after pretreatment with cyclophosphamide. He has had three episodes of graft-versus-host disease (GvHD), all of which resolved with pulses of anti-CD3 antibodies and corticosteroids. His current medications include cyclosporine, methotrexate, and prednisone. He has had hematuria for 10 days and watery diarrhea for 5. While in the ICU his respiratory distress worsens and there is an urgent intubation to allow for adequate oxygenation. All cultures are negative. At this stage you are not sure of what might be going on but are aware of a number of possibilities.
QUESTIONS FOR GROUP DISCUSSION
RECOMMENDED APPROACH
Implications/Analysis of Family History
CML is a clonal disorder of hematopoietic progenitor cells. Consequently, all cell types arising from that progenitor cell will be affected and increased in cell number. This would include granulocytes, monocytes, and platelets. Although the average age at which patients are diagnosed is 53, this disorder also occurs in young adults and children. White males are more likely to get CML than white women or African-American males. Hereditary factors are not known and may not play a role in disease susceptibility because an identical twin does not show greater susceptibility than a sibling when one twin has been diagnosed with CML.
Implications/Analysis of Laboratory Investigations
In general, CML patients have an elevated white blood cell count (see Appendix for reference value) as well as an elevated platelet count (increase of ∼ 40%), in the absence of infection or an inflammatory response.
ETIOLOGY: GRAFT VERSUS HOST DISEASE
Clinical Presentation: GvHD or Infection?
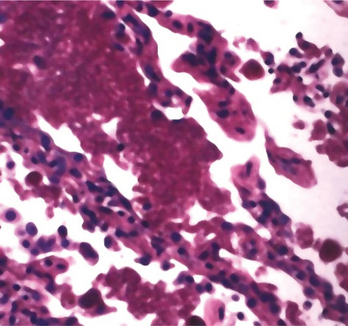
GvHD itself presents often as a multisystem disease with gastrointestinal, lung, genitourinary, and skin involvement. Treatment of GvHD would involve a pulse of increased immunosuppressive drugs. However, an alternative cause of the presenting complaints may itself be an infectious episode, secondary to the immunosuppression to which the patient has been exposed already to allow engraftment (prevent rejection) of the bone marrow graft. This immunosuppression exposes the patient to multiple opportunistic infections (somewhat analogous to HIV infection or patients treated for autoimmune disorders), among which lung pathogens (CMV, Pneumocystis) would rank high on the list (Fig. 33-1). In addition, some of the immunosuppressive drugs used (methotrexate, in particular) can often induce hepatic and/or lung toxicity on their own accord.
Therapy
A reasonable plan might be to treat the most likely pathogens (assuming infection), while at the same time trying to generate data (cultures of serum/urine/blood/cerebrospinal fluid) that would support that hypothesis and attempt to investigate further for signs of GvHD (biopsy of available tissue from affected organs [e.g., liver/bronchoscopy of the lung]) before beginning increased immunosuppressive therapy to treat that option.