CHAPTER 32
Hand and Wrist Ganglia
Definition
Hand and wrist ganglia account for 50% to 70% of all hand masses. The ganglion is a benign, mucin-filled cyst found in relation to a joint, ligament, or tendon. It is typically filled from the joint through a tortuous duct or “stalk” that functions as a valve directing the flow of fluid. The mucin itself contains high concentrations of hyaluronic acid as well as glucosamine, albumin, and globulin [1]. When it is used to describe ganglia, the term synovial cyst is actually a misnomer because ganglion cysts do not contain synovial fluid and are not true cysts lined by epithelium but rather by flat cells. The etiology of ganglia remains a mystery, although many think that ligamentous degeneration or trauma plays an important role [1,2].
By far, the most common location for a ganglion is the dorsal wrist (Fig. 32.1), with the pedicle arising from the scapholunate ligament in virtually all cases. Only 20% of ganglia are found on the volar wrist (Fig. 32.2). This type may originate from either the radioscaphoid or scaphotrapezial joint. Alternatively, ganglia can occur near the joints of the finger. One subtype of hand-wrist ganglia is the “occult” cyst, which is not palpable on physical examination.


Ganglion cysts occur more commonly in women, usually between the ages of 20 and 30 years. However, they can develop in either sex at any age. Ganglia of childhood usually resolve spontaneously during the course of 1 year [3]. The most commonly seen ganglion of the elderly, the mucous cyst, arises from an arthritic distal interphalangeal joint (Fig. 32.3).

Other common types of ganglia in the hand include the retinacular cyst (flexor tendon sheath ganglion; Fig. 32.4), proximal interphalangeal joint ganglion, and first extensor compartment cyst associated with de Quervain tenosynovitis. Less common ganglia include cysts within the extensor tendons or carpal bones (intraosseous) and those associated with a second or third carpometacarpal boss (arthritic spur). Rarely, ganglia within the carpal tunnel or Guyon canal can produce carpal tunnel syndrome or ulnar neuropathy, respectively.
As noted, the cause of ganglion cyst formation is not known, but there may be a link to light, repetitive activity, demonstrated by an increased incidence in typists, musicians, and draftsmen. Interestingly, there is no increased risk in heavy laborers, who bear a greater load on their wrists. Wrist instability has also been discussed as both a possible cause and an effect of the disease. Overall, there is a history of trauma in 10% to 30% of people presenting with the disease [2].
Symptoms
Patients with a wrist ganglion usually present with a painless wrist or hand mass of variable duration. The cyst may fluctuate in size or disappear altogether for a time. Pain and weakness of grip are occasional presenting symptoms; however, an underlying concern about the appearance or seriousness of the problem is usually the reason for seeking medical attention. The pain, when present, is most often described as aching and aggravated by certain motions. With dorsal wrist ganglia, patients often complain of discomfort as the wrist is forcefully extended (e.g., when pushing up from a chair). Interestingly, dorsal wrist pain may be the principal complaint of patients with an occult dorsal wrist ganglion, which is not readily visible. The wrist pain usually subsides as the mass enlarges.
With a retinacular cyst, patients usually complain of slight discomfort when gripping, for example, a racket handle or shopping cart. Patients whose complaints of pain are primarily related to de Quervain tenosynovitis (see Chapter 28) may notice a bump over the radial styloid area. Pain with grip is also a complaint of patients with a carpometacarpal boss. On occasion, the digital extensor tendons may jump over the cyst with radioulnar deviation. Mucous cysts can drain spontaneously and can also produce nail deformity, either of which may be a presenting complaint. Symptoms identical to those of carpal tunnel syndrome will be noted by patients with a carpal tunnel ganglion. A ganglion in the Guyon canal will produce hand weakness (due to loss of intrinsic function) and may produce numbness in the ring and small fingers.
Physical Examination
Ganglia are typically solitary cysts, although they are often found to be multiloculated on surgical exploration. They are usually mobile a few millimeters in all directions on physical examination. The mass may be slightly tender. When the cyst is large, transillumination (placing a penlight directly onto the skin overlying the mass) will help differentiate it from a solid tumor.
The classic location for a dorsal wrist ganglion is ulnar to the extensor pollicis longus, between the third and fourth tendon compartments, or directly over the scapholunate ligament [1]. However, these ganglia may have a long pedicle that courses through various tendon compartments and exits at different locations on the dorsal wrist or even the volar wrist. When the ganglion is small, it may be apparent only with wrist flexion. Wrist extension and grip strength may be slightly diminished. Dorsal wrist pain and tenderness with no obvious mass or instability should suggest an occult ganglion.
Volar ganglia occur most commonly at the wrist flexion crease on the radial side of the flexor carpi radialis tendon but may extend into the palm or proximally, or even dorsally, into the carpal tunnel. They can involve the radial artery, complicating their surgical removal. They may seem to be pulsatile, although careful inspection will demonstrate that the radial artery is draped over the mass.
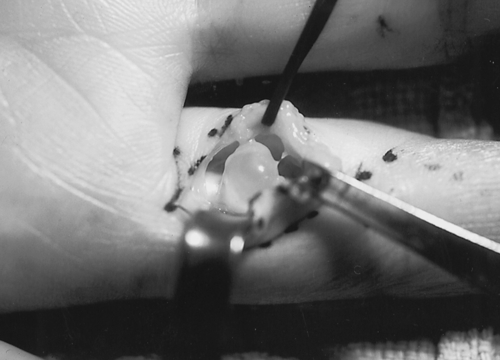
Retinacular cysts are usually not visible but are palpable as pea-sized masses, typically located at the volar aspect of the digit at the palmar digital crease. They are adherent to the flexor tendon sheath and do not move with finger flexion. Alternatively, intratendinous ganglia are distinguished by the fact that they move with finger motion.
Mucous cysts are located over the distal interphalangeal joint, and the overlying skin may be quite thin. They are occasionally mistaken for warts. Spontaneous drainage and even septic distal interphalangeal joint arthritis are not uncommon. Nail plate deformity is an associated finding. Proximal interphalangeal joint ganglia are located on the dorsum of the digit, slightly off midline. Ganglia associated with carpometacarpal bosses produce tender prominences on the dorsum of the hand distal to the typical location for a wrist ganglion.
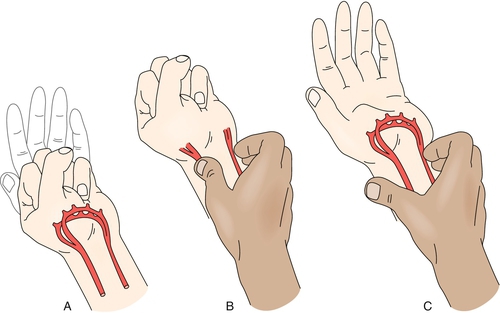
An important sign to look for on physical examination, especially in planning for surgery, is compression of the median or ulnar nerve or of the radial artery. An Allen test should be performed before surgery to evaluate radial and ulnar artery patency, particularly in the case of a volar cyst (Fig. 32.5).
Functional Limitations
Physical limitations due to ganglion cysts are rare. With dorsal wrist ganglia, fatigue and weakness are occasional findings. Patients may have difficulty with weight bearing on the affected extremity with the wrist extended (e.g., when pushing up from a chair).
Diagnostic Studies
The diagnosis of a ganglion cyst is usually straightforward, and ancillary studies are often unnecessary. With wrist ganglia, plain radiographs of the wrist are usually obtained preoperatively to evaluate the carpal relationships and to exclude the possibility of an intraosseous ganglion. With a mucous cyst, radiographs of the affected digit will usually demonstrate a distal interphalangeal joint osteophyte. Ultrasonography or magnetic resonance imaging may be useful in identifying deep cysts in cases of vague dorsal wrist pain. Specifically, magnetic resonance imaging is indicated to rule out Kienböck disease in patients with dorsal wrist pain and no obvious ganglion or wrist instability. In hand soft tissue masses when magnetic resonance imaging is nondiagnostic, the most common underlying diagnoses include giant cell tumor of tendon sheath, angioleiomyoma, fibroma, and peripheral nerve sheath tumor [4]. Cyst aspiration is the single best confirmatory study for ganglion. Aspiration characteristically yields a viscous, clear to yellowish fluid with the appearance and consistency of apple jelly. On occasion, the fluid will be blood tinged.
Treatment
Initial
Reassurance is the single most important initial treatment. Many patients are satisfied to know that they do not have a serious illness. It is important to tell patients that the cyst often fluctuates in size and occasionally disappears on its own. Undoubtedly, observation is the most appropriate treatment of ganglia in children, as long as the diagnosis is certain. In adults, splinting is an appropriate initial treatment of cysts associated with discomfort. A cock-up wrist splint is prescribed for carpometacarpal and dorsal and volar wrist ganglia, whereas a radial gutter splint is prescribed for ganglia associated with de Quervain tenosynovitis. Traditional methods of crushing the cyst with a coin or a Bible, even though occasionally successful, are not recommended. Anecdotally, daily massage of mucous cysts by patients may be successful in resolving them as long as the overlying skin is healthy. Analgesics or nonsteroidal anti-inflammatory drugs may be used on a limited basis for discomfort but do little to treat the disorder.
Rehabilitation
Rehabilitation has a role primarily in the postsurgical setting. The usual course of treatment after dorsal ganglion excision involves 7 to 14 days of immobilization in slight wrist flexion to minimize loss of wrist flexion secondary to scarring. Frequent, active range of motion of the wrist should be started after splint removal, and the patient should be able to return to relatively normal activity approximately 3 weeks after surgery [1]. Most patients are able to carry out their own rehabilitation at home. Formal therapy can be ordered if patients have difficulty returning to normal functioning. Therapy may include modalities for pain control, active-assisted and passive range of motion exercises, and strengthening exercises. Therapists may also evaluate return to work issues, including adaptive equipment that may assist patients in their daily work functions.
Procedures
Aspiration of the cyst serves two purposes: it confirms the diagnosis, and it may be therapeutic. Unfortunately, the recurrence rate after ganglion aspiration is high. One study [5] demonstrated long-term success rates of 27% and 43% for dorsal and volar wrist ganglia, respectively, treated with aspiration, multiple puncture, and 3 weeks of immobilization. Importantly, cysts present for longer than 6 months almost uniformly recurred. The results for aspiration of retinacular cysts were somewhat better, averaging 69% successful.
However, a significant number of patients may elect to proceed with cyst aspiration despite the high likelihood of recurrence. Aspiration of volar wrist ganglia may cause displacement of the cyst and envelop the radial artery. Aspiration of proximal interphalangeal joint ganglia may be successful in eliminating the cyst [6]. Aspiration of mucous cysts is not recommended.
Steroids have not been shown to add any therapeutic benefit to ganglia aspiration.
Surgery
Many patients opt for surgical excision of the cyst, often for primarily cosmetic reasons. Surgery should be advised when the diagnosis is unclear. To minimize the likelihood of recurrence, the surgeon should not only remove the cyst but trace the stalk to its origin within the joint. For wrist ganglia, the surgeon often finds that the visible mass grossly underestimates its actual size and extent. Because these procedures require opening of the wrist joint, they cannot be performed with the use of local anesthesia. With proper technique, recurrence rates should be less than 5%. Volar ganglia are more difficult to access and more often variable in their shape and location, making for more complicated surgery. A prospective cohort study of volar wrist ganglion treatment by observation, aspiration, or surgery concluded that at 5 years, there were no significant differences in the recurrence rates with any of the treatments; 42% of the excised ganglia recurred, whereas 51% of the untreated ganglia had resolved spontaneously [7]. Clearly, it is important that the risks and benefits of surgical treatment of ganglion cysts be carefully discussed with the patient.
Arthroscopic resection of dorsal wrist ganglia has been advocated to be a safe and reliable procedure, with recurrence rates of less than 5% [8]. A small case series of arthroscopic débridement of volar wrist ganglia has demonstrated excellent results as well [9].
The surgical management of mucous cysts must include excision of the cyst stalk as well as the offending osteophyte, which originates from either the dorsal base of the distal phalanx or the head of the middle phalanx. The nail deformity should resolve during several months [10].
Potential Disease Complications
Chronic wrist pain as the result of an untreated wrist ganglion is rare. The cosmetic deformity, however, is obvious. The most important complication associated with a neglected cyst is septic arthritis of the distal interphalangeal joint resulting from spontaneous drainage of a mucous cyst. For that reason, we recommend mucous cyst excision when the overlying skin is thin or spontaneous drainage has occurred.
Potential Treatment Complications
Analgesics and nonsteroidal anti-inflammatory drugs have well-known side effects that most commonly affect the gastric, hepatic, and renal systems. The patient must understand that surgery will replace a bump with a scar. Slight limitation of wrist flexion after dorsal ganglion excision is not uncommon. Another risk is iatrogenic injury to the scapholunate ligament, extensor tendon, and cutaneous nerve. Recurrence is another possibility.
Surgery performed on the volar wrist carries a greater risk of injury to artery and nerve. The structures most at risk are the palmar cutaneous branch of the median nerve and the terminal branches of the lateral antebrachial cutaneous nerve as well as the radial artery, which is often intertwined with the cyst. Perhaps because of the more intricate nature of its surgical removal, the volar cyst is associated with a higher rate of recurrence after surgery.







