Procedure 32 Crossed Intrinsic Tendon Transfer
![]() See Video 24: Crossed Intrinsic Tendon Transfer for Correction of Ulnar Deviation Deformity
See Video 24: Crossed Intrinsic Tendon Transfer for Correction of Ulnar Deviation Deformity
Indications
 Performed in rheumatoid arthritis patients who have passively correctable ulnar deviation deformity (Fig. 32-1) with associated ulnar subluxation of the extensor tendon at the metacarpophalangeal (MCP) joint (Fig. 32-2) without arthritis or subluxation
Performed in rheumatoid arthritis patients who have passively correctable ulnar deviation deformity (Fig. 32-1) with associated ulnar subluxation of the extensor tendon at the metacarpophalangeal (MCP) joint (Fig. 32-2) without arthritis or subluxation
 Ulnar subluxation of extensor tendon in chronic posttraumatic radial sagittal band injury
Ulnar subluxation of extensor tendon in chronic posttraumatic radial sagittal band injury
Examination/Imaging
Clinical Examination
 Clinical examination is to determine the condition of the MCP joint and the intrinsic tendons.
Clinical examination is to determine the condition of the MCP joint and the intrinsic tendons.
 A crossed intrinsic tendon transfer cannot be done in a patient who has a subluxed or arthritic MCP joint (Fig. 32-3). These patients need implant arthroplasty because a soft tissue procedure will not be able to hold a subluxed MCP joint in position. In addition, the patient is examined for the presence of MCP joint synovitis that can be addressed at the same operation.
A crossed intrinsic tendon transfer cannot be done in a patient who has a subluxed or arthritic MCP joint (Fig. 32-3). These patients need implant arthroplasty because a soft tissue procedure will not be able to hold a subluxed MCP joint in position. In addition, the patient is examined for the presence of MCP joint synovitis that can be addressed at the same operation.
 The intrinsic tendons should be examined for the presence of intrinsic muscle contracture (intrinsic tightness). This is done by the Finochietto-Bunnell test, which is performed by passively holding the patient’s MCP joint in full extension and attempting proximal interphalangeal (PIP) joint flexion. PIP joint flexion will be restricted in patients with intrinsic tightness (Fig. 32-4A and B).
The intrinsic tendons should be examined for the presence of intrinsic muscle contracture (intrinsic tightness). This is done by the Finochietto-Bunnell test, which is performed by passively holding the patient’s MCP joint in full extension and attempting proximal interphalangeal (PIP) joint flexion. PIP joint flexion will be restricted in patients with intrinsic tightness (Fig. 32-4A and B).
Surgical Anatomy
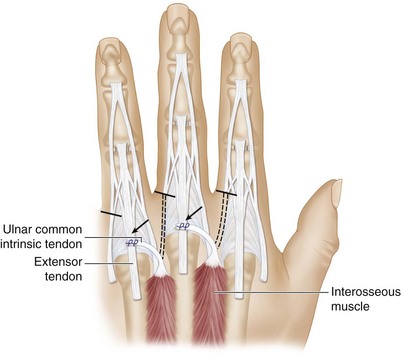
 The common intrinsic tendon is formed by the tendons of the palmar and dorsal interosseous muscles on the ulnar side of the digit and by the interossei (palmar and dorsal) and the lumbrical tendon on the radial side. These tendons pass palmar to the axis of the MCP joint to form the common intrinsic tendon. This tendon then divides into a medial band that inserts along with the central slip into the dorsal base of the middle phalanx and a lateral band that continues to the dorsal base of the distal phalanx (Fig. 32-5A). Contraction of the intrinsic muscles causes MCP joint flexion and interphalangeal (IP) joint extension. The radial and ulnar sagittal bands stabilize the extensor tendon, keeping it over the dorsal midline of the MCP joint (Fig. 32-5B).
The common intrinsic tendon is formed by the tendons of the palmar and dorsal interosseous muscles on the ulnar side of the digit and by the interossei (palmar and dorsal) and the lumbrical tendon on the radial side. These tendons pass palmar to the axis of the MCP joint to form the common intrinsic tendon. This tendon then divides into a medial band that inserts along with the central slip into the dorsal base of the middle phalanx and a lateral band that continues to the dorsal base of the distal phalanx (Fig. 32-5A). Contraction of the intrinsic muscles causes MCP joint flexion and interphalangeal (IP) joint extension. The radial and ulnar sagittal bands stabilize the extensor tendon, keeping it over the dorsal midline of the MCP joint (Fig. 32-5B).
Exposures
 A dorsal “lazy S”–shaped skin incision over the MCP joint is used if only one finger needs to be addressed (Fig. 32-6).
A dorsal “lazy S”–shaped skin incision over the MCP joint is used if only one finger needs to be addressed (Fig. 32-6).
 For correction of multiple fingers, a dorsal transverse incision is made over the MCP joint of the involved fingers (Fig. 32-7).
For correction of multiple fingers, a dorsal transverse incision is made over the MCP joint of the involved fingers (Fig. 32-7).
 The extensor apparatus over the MCP joint is exposed (Fig. 32-8).
The extensor apparatus over the MCP joint is exposed (Fig. 32-8).
Procedure
Step 1: Examination of the Extensor Apparatus and MCP Joint Synovectomy
Step 2: Elevation of Ulnar Common Intrinsic Tendon
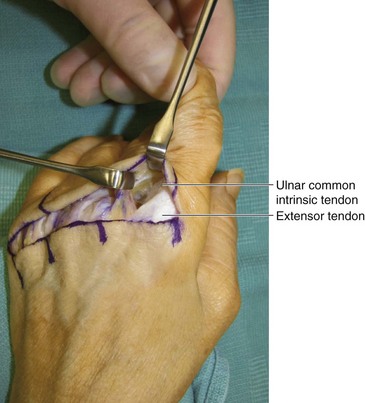
 Dissection is carried out on the ulnar aspect of the proximal phalangeal base in a plane superficial to the extensor apparatus. The interosseous tendons are identified at the base of the MCP joint, and they are followed distally until the formation of the common intrinsic tendon (Fig. 32-10).
Dissection is carried out on the ulnar aspect of the proximal phalangeal base in a plane superficial to the extensor apparatus. The interosseous tendons are identified at the base of the MCP joint, and they are followed distally until the formation of the common intrinsic tendon (Fig. 32-10).
 The common intrinsic tendon is divided transversely at the midproximal phalanx before it divides into medial and lateral bands. It is then divided longitudinally to separate it from the extensor expansion.
The common intrinsic tendon is divided transversely at the midproximal phalanx before it divides into medial and lateral bands. It is then divided longitudinally to separate it from the extensor expansion.
 The common intrinsic tendon is mobilized proximally to the MCP joint (Fig. 32-11).
The common intrinsic tendon is mobilized proximally to the MCP joint (Fig. 32-11).
Step 3: Transfer of the Ulnar Common Intrinsic Tendon
 The mobilized ulnar common intrinsic tendon is passed under the soft tissue between adjacent MCP joints (it contains longitudinal veins and dorsal sensory nerves) to reach the extensor tendon of the digit ulnar to it (Fig. 32-12).
The mobilized ulnar common intrinsic tendon is passed under the soft tissue between adjacent MCP joints (it contains longitudinal veins and dorsal sensory nerves) to reach the extensor tendon of the digit ulnar to it (Fig. 32-12).
 The index finger ulnar common intrinsic tendon is used to correct the long finger; the long finger tendon is used for the ring finger; and the ring finger tendon is used for the small finger. Ulnar deviation of the index finger is corrected by double-breasted repair of the radial sagittal band.
The index finger ulnar common intrinsic tendon is used to correct the long finger; the long finger tendon is used for the ring finger; and the ring finger tendon is used for the small finger. Ulnar deviation of the index finger is corrected by double-breasted repair of the radial sagittal band.
Step 4: Centralization of Extensor Tendon
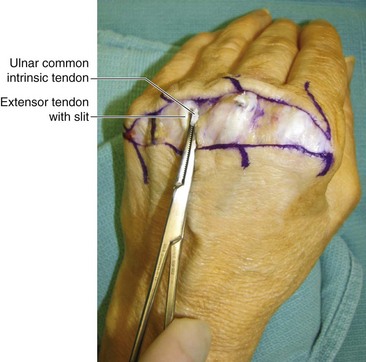
 A 3- to 4-mm longitudinal slit is made in the midportion of the extensor tendon overlying the MCP joint. The ulnar common intrinsic tendon is passed through this slit and sutured to itself using one or two horizontal mattress 3-0 Ethibond sutures. Tension is adjusted by keeping the MCP joint in extension and correcting the ulnar deviation deformity. This centralizes the extensor tendon (Figs. 32-13 and 32-14).
A 3- to 4-mm longitudinal slit is made in the midportion of the extensor tendon overlying the MCP joint. The ulnar common intrinsic tendon is passed through this slit and sutured to itself using one or two horizontal mattress 3-0 Ethibond sutures. Tension is adjusted by keeping the MCP joint in extension and correcting the ulnar deviation deformity. This centralizes the extensor tendon (Figs. 32-13 and 32-14).
 A double-breasted repair of the radial sagittal band is done using one or two 3-0 Ethibond mattress sutures (Fig. 32-15).
A double-breasted repair of the radial sagittal band is done using one or two 3-0 Ethibond mattress sutures (Fig. 32-15).
Postoperative Care and Expected Outcomes
 The hand is immobilized with a volar hand splint that keeps the MCP joint extended and corrects the ulnar deviation deformity. The wound is inspected 10 days later, and the sutures are removed. The patient is then given a thermoplastic splint to maintain the MCP joint in extension for another 4 weeks. This is followed by a gradual mobilization protocol and protective splinting for another 4 weeks.
The hand is immobilized with a volar hand splint that keeps the MCP joint extended and corrects the ulnar deviation deformity. The wound is inspected 10 days later, and the sutures are removed. The patient is then given a thermoplastic splint to maintain the MCP joint in extension for another 4 weeks. This is followed by a gradual mobilization protocol and protective splinting for another 4 weeks.
 A crossed intrinsic transfer provides reliable long-term correction of the ulnar drift deformity in patients without MCP joint subluxation. However, it may be associated with a decrease in active range of motion at the MCP joint.
A crossed intrinsic transfer provides reliable long-term correction of the ulnar drift deformity in patients without MCP joint subluxation. However, it may be associated with a decrease in active range of motion at the MCP joint.
Clark DI, Delaney R, Stilwell JH, et al. The value of crossed intrinsic transfer after metacarpophalangeal silastic arthroplasty: a comparative study. J Hand Surg [Br]. 2001;26:565-567.
Oster LH, Blair WF, Steyers CM, Flatt AE. Crossed intrinsic transfer. J Hand Surg [Am]. 1989;14:963-971.
Pereira JA, Belcher HJ. A comparison of metacarpophalangeal joint Silastic arthroplasty with or without crossed intrinsic transfer. J Hand Surg [Br]. 2001;26:229-234.