Procedure 31 Tendon Transfers for Extensor and Flexor Tendon Ruptures
![]() See Video 23: Tendon Transfers for the Ruptured Flexor and Extensor Tendons
See Video 23: Tendon Transfers for the Ruptured Flexor and Extensor Tendons
Examination/Imaging
Clinical Examination
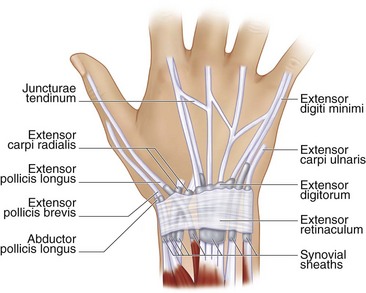
 The most frequently ruptured tendons in rheumatoid arthritis (RA) are the extensor digiti minimi (EDM), followed by the extensor digitorum communis (EDC) tendons to the small, ring, long, and index fingers, in that order; the extensor pollicis longus (EPL); the flexor pollicis longus (FPL); and, rarely, the flexor digitorum superficialis (FDS) and the flexor digitorum profundus (FDP).
The most frequently ruptured tendons in rheumatoid arthritis (RA) are the extensor digiti minimi (EDM), followed by the extensor digitorum communis (EDC) tendons to the small, ring, long, and index fingers, in that order; the extensor pollicis longus (EPL); the flexor pollicis longus (FPL); and, rarely, the flexor digitorum superficialis (FDS) and the flexor digitorum profundus (FDP).
 Patients with isolated small finger extensor tendon (EDM) rupture may still be able to extend the small fingers through the EDC or through the juncturae connecting it to the ring finger (Fig. 31-1). However, these patients will not be able to perform independent extension of the small finger with the other fingers flexed.
Patients with isolated small finger extensor tendon (EDM) rupture may still be able to extend the small fingers through the EDC or through the juncturae connecting it to the ring finger (Fig. 31-1). However, these patients will not be able to perform independent extension of the small finger with the other fingers flexed.
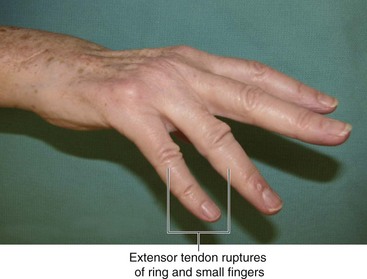
 Patients with rupture of the EDC to one finger may still be able to extend the finger owing to the juncturae connecting it to intact adjoining fingers. However, patients are usually unable to extend the finger when they have ruptured more than one EDC (Fig. 31-2). The inability to extend the finger in RA may also be caused by ulnar subluxation of the extensor tendons over the head of the metacarpal (Fig. 31-3) and rarely is due to posterior interosseous nerve palsy resulting from elbow synovitis. To differentiate between these causes, it is useful to passively extend the finger and ask the patient to hold it there. Patients with tendon rupture or nerve palsy will be unable to maintain the finger in extension, whereas patients with subluxation will be able to do so as the tendon relocates over the metacarpophalangeal (MCP) joint with finger extension. Patients with tendon rupture will also lose the tenodesis effect of finger extension with wrist flexion, whereas the tenodesis effect will be preserved in nerve palsy.
Patients with rupture of the EDC to one finger may still be able to extend the finger owing to the juncturae connecting it to intact adjoining fingers. However, patients are usually unable to extend the finger when they have ruptured more than one EDC (Fig. 31-2). The inability to extend the finger in RA may also be caused by ulnar subluxation of the extensor tendons over the head of the metacarpal (Fig. 31-3) and rarely is due to posterior interosseous nerve palsy resulting from elbow synovitis. To differentiate between these causes, it is useful to passively extend the finger and ask the patient to hold it there. Patients with tendon rupture or nerve palsy will be unable to maintain the finger in extension, whereas patients with subluxation will be able to do so as the tendon relocates over the metacarpophalangeal (MCP) joint with finger extension. Patients with tendon rupture will also lose the tenodesis effect of finger extension with wrist flexion, whereas the tenodesis effect will be preserved in nerve palsy.
 The function of the EPL is tested by asking the patient to lay the palm of the hand flat on the table and then asking the patient to lift the thumb away from the table (retropulsion).
The function of the EPL is tested by asking the patient to lay the palm of the hand flat on the table and then asking the patient to lift the thumb away from the table (retropulsion).
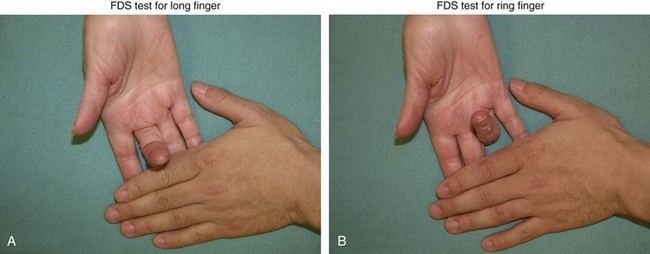
 One must also examine the integrity of the EIP by testing for independent extension of the index finger with the other fingers held in flexion. The function of the FDS and FDP is also checked. The EIP and FDS to the ring and long fingers are often used as motors for tendon transfers in patients with rupture of multiple extensor tendons. Figure 31-4 shows testing for FDS function of the long and ring fingers.
One must also examine the integrity of the EIP by testing for independent extension of the index finger with the other fingers held in flexion. The function of the FDS and FDP is also checked. The EIP and FDS to the ring and long fingers are often used as motors for tendon transfers in patients with rupture of multiple extensor tendons. Figure 31-4 shows testing for FDS function of the long and ring fingers.
Imaging
 It is important to obtain radiographs of the wrist to evaluate the distal radioulnar (DRU), midcarpal, and radiocarpal joints. Pathology involving these joints will also need to be addressed at the time of tendon reconstruction to prevent progressive deformity and rerupture of the reconstructed tendons.
It is important to obtain radiographs of the wrist to evaluate the distal radioulnar (DRU), midcarpal, and radiocarpal joints. Pathology involving these joints will also need to be addressed at the time of tendon reconstruction to prevent progressive deformity and rerupture of the reconstructed tendons.
Surgical Anatomy
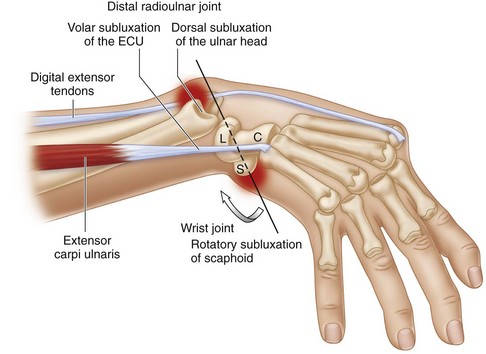
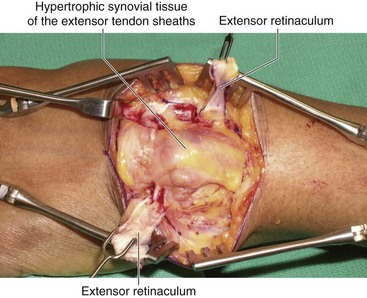
 Tendon rupture in RA occurs as a result of either synovitis or attrition over an eroded bone. The tendon may be directly invaded by the synovial pannus. This occurs in regions where the tendon is covered by tenosynovium (extensor retinaculum, carpal tunnel, and digital flexor sheath). Rupture may also result from ischemia caused by pressure from underlying proliferative synovitis. This occurs in regions where the tendon is in close relation to joints (DRU, radiocarpal, proximal interphalangeal [PIP] joints). Attritional rupture frequently involves the EDM at the ulnar head (Fig. 31-5), EPL at the Lister tubercle, and FPL in the carpal tunnel caused by a flexed scaphoid (see Fig. 31-5). Synovitis between the scaphoid and lunate leads to rupture of the scapholunate ligament and collapse of the scaphoid (scaphoid becomes horizontal with the distal pole protruding into the carpal tunnel).
Tendon rupture in RA occurs as a result of either synovitis or attrition over an eroded bone. The tendon may be directly invaded by the synovial pannus. This occurs in regions where the tendon is covered by tenosynovium (extensor retinaculum, carpal tunnel, and digital flexor sheath). Rupture may also result from ischemia caused by pressure from underlying proliferative synovitis. This occurs in regions where the tendon is in close relation to joints (DRU, radiocarpal, proximal interphalangeal [PIP] joints). Attritional rupture frequently involves the EDM at the ulnar head (Fig. 31-5), EPL at the Lister tubercle, and FPL in the carpal tunnel caused by a flexed scaphoid (see Fig. 31-5). Synovitis between the scaphoid and lunate leads to rupture of the scapholunate ligament and collapse of the scaphoid (scaphoid becomes horizontal with the distal pole protruding into the carpal tunnel).
Treatment Considerations
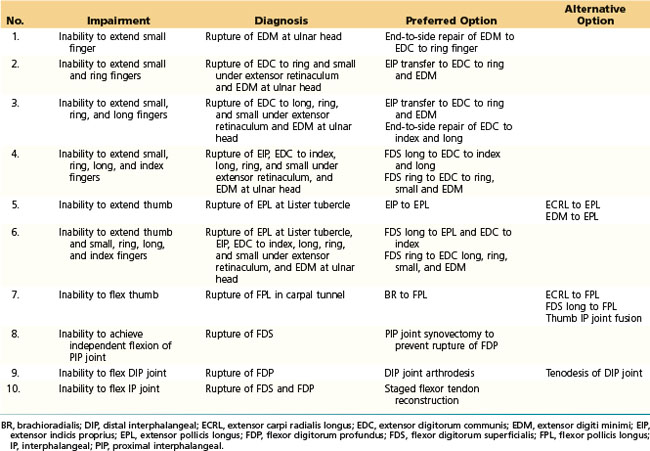
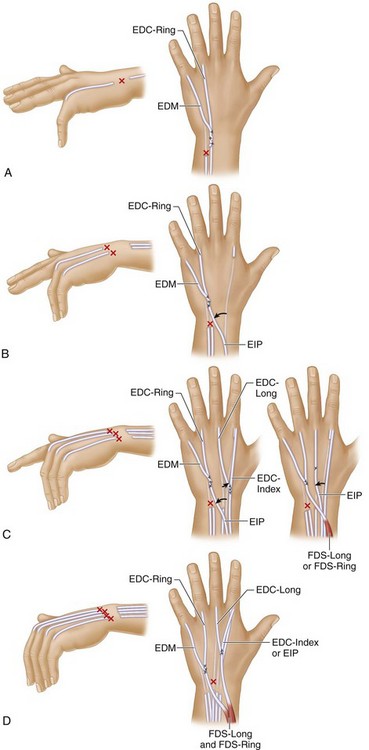
 Direct repair of ruptured tendons is usually not possible because the ruptured ends are of very poor quality. Additionally, these patients frequently present late, and a tendon graft is also not a reliable option owing to proximal myostatic contraction. A tendon transfer is the preferred option for reconstruction. Depending on the number of ruptured tendons, this may involve a simple end-to-side repair to an intact adjacent tendon or may require transfer of a new motor from the extensor or flexor side (Table 31-1; Fig. 31-6).
Direct repair of ruptured tendons is usually not possible because the ruptured ends are of very poor quality. Additionally, these patients frequently present late, and a tendon graft is also not a reliable option owing to proximal myostatic contraction. A tendon transfer is the preferred option for reconstruction. Depending on the number of ruptured tendons, this may involve a simple end-to-side repair to an intact adjacent tendon or may require transfer of a new motor from the extensor or flexor side (Table 31-1; Fig. 31-6).
 It is important to address the cause of the tendon rupture at the time of tendon reconstruction. This may require tendon and joint synovectomy and procedures to address any joint instability and bony erosions. For example, if the patient has small-finger extensor tendon rupture, it is highly likely that the ring finger extensor tendon will rupture subsequently, and this process will progress, resulting in ruptures of all the extensor tendons to the fingers. Therefore, when a patient has an extensor tendon rupture of the small finger, tendon reconstruction and either tenosynovectomy or distal ulna excision, or a combination of both, must be performed to prevent progressive ruptures of the other tendons.
It is important to address the cause of the tendon rupture at the time of tendon reconstruction. This may require tendon and joint synovectomy and procedures to address any joint instability and bony erosions. For example, if the patient has small-finger extensor tendon rupture, it is highly likely that the ring finger extensor tendon will rupture subsequently, and this process will progress, resulting in ruptures of all the extensor tendons to the fingers. Therefore, when a patient has an extensor tendon rupture of the small finger, tendon reconstruction and either tenosynovectomy or distal ulna excision, or a combination of both, must be performed to prevent progressive ruptures of the other tendons.
Exposures
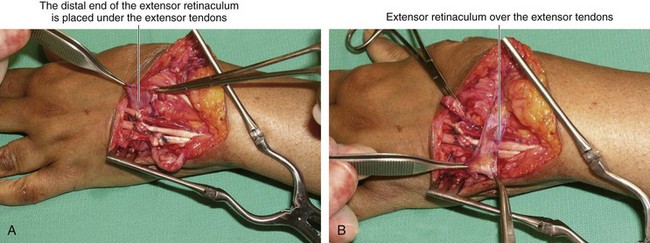
 A 6-cm longitudinal incision is made over the dorsum of the wrist in line with the long finger metacarpal (Fig. 31-7). Skin flaps are raised to expose the extensor retinaculum (Fig. 31-8). The extensor retinaculum is elevated using a stair-step design (Fig. 31-9). The stair-step incision is used to permit easier closure of the extensor retinaculum in a side-to-side fashion, rather than a straight line closure, which may be difficult because of the swelling under the retinaculum that puts pressure over the retinacular closure. Furthermore, if there is radiocarpal bone erosion, half of the retinaculum can be placed under the extensor tendons to shield the wrist from the extensor tendons, and the other half is used to close over the tendons. The septae are divided between the second and third; third and fourth; fourth and fifth; and fifth and sixth extensor compartments. This converts the multiple extensor compartments into a single compartment and reveals the exuberant amount of synovial tissue encasing the extensor tendons (Fig. 31-10).
A 6-cm longitudinal incision is made over the dorsum of the wrist in line with the long finger metacarpal (Fig. 31-7). Skin flaps are raised to expose the extensor retinaculum (Fig. 31-8). The extensor retinaculum is elevated using a stair-step design (Fig. 31-9). The stair-step incision is used to permit easier closure of the extensor retinaculum in a side-to-side fashion, rather than a straight line closure, which may be difficult because of the swelling under the retinaculum that puts pressure over the retinacular closure. Furthermore, if there is radiocarpal bone erosion, half of the retinaculum can be placed under the extensor tendons to shield the wrist from the extensor tendons, and the other half is used to close over the tendons. The septae are divided between the second and third; third and fourth; fourth and fifth; and fifth and sixth extensor compartments. This converts the multiple extensor compartments into a single compartment and reveals the exuberant amount of synovial tissue encasing the extensor tendons (Fig. 31-10).
Procedure
Step 1: Synovectomy
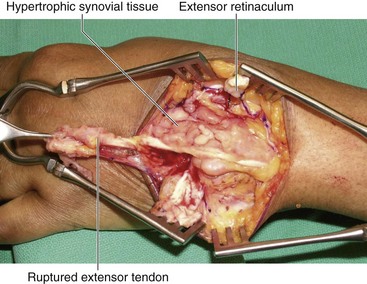
 Fresh, sharp no. 15 blades are used to excise the synovial tissue from the extensor tendons. Tendons with invading synovial tissue within the extensor tendons must be excised completely (Fig. 31-11).
Fresh, sharp no. 15 blades are used to excise the synovial tissue from the extensor tendons. Tendons with invading synovial tissue within the extensor tendons must be excised completely (Fig. 31-11).
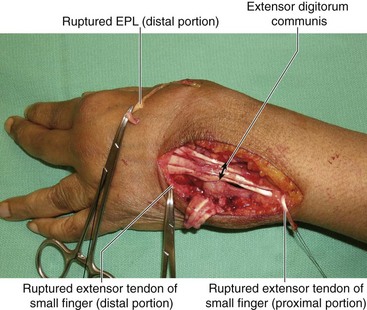
 After removing the synovial tissue, one can appreciate multiple ruptured extensor tendons that will require reconstruction (Fig. 31-12).
After removing the synovial tissue, one can appreciate multiple ruptured extensor tendons that will require reconstruction (Fig. 31-12).
Step 2: Tendon Transfer for the Ruptured Tendons
 The reconstructive plan depends on the number of ruptured extensor tendons (see Table 31-1).
The reconstructive plan depends on the number of ruptured extensor tendons (see Table 31-1).
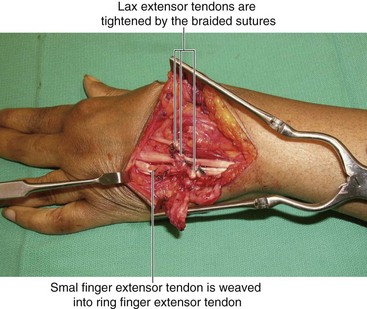
 All the tendon junctures are secured using braided sutures.
All the tendon junctures are secured using braided sutures.
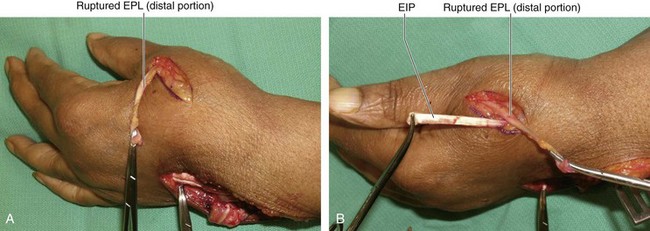
 Figure 31-13 shows a separate incision made at the level of the metacarpal to identify the distal EPL tendon. The EIP tendon was transferred to weave into the EPL tendon to restore EPL tendon function.
Figure 31-13 shows a separate incision made at the level of the metacarpal to identify the distal EPL tendon. The EIP tendon was transferred to weave into the EPL tendon to restore EPL tendon function.
 Figure 31-14 shows the repair of the distal end of the small finger extensor tendon to the intact ring finger extensor tendon in an end-to-side fashion.
Figure 31-14 shows the repair of the distal end of the small finger extensor tendon to the intact ring finger extensor tendon in an end-to-side fashion.
 When more than three extensor tendons are ruptured, the FDS tendons are used for transfer. The FDS of the ring finger is identified and divided through a transverse incision in the distal palm. This tendon is then retrieved in the distal forearm by a separate longitudinal incision and passed in a subcutaneous tunnel on the radial aspect of the forearm to reach the extensor tendons on the dorsum of the wrist. A single FDS tendon can be used to motorize up to three extensor tendons. If more than three extensors are ruptured, one should consider transfer of both the ring and long finger FDS tendons.
When more than three extensor tendons are ruptured, the FDS tendons are used for transfer. The FDS of the ring finger is identified and divided through a transverse incision in the distal palm. This tendon is then retrieved in the distal forearm by a separate longitudinal incision and passed in a subcutaneous tunnel on the radial aspect of the forearm to reach the extensor tendons on the dorsum of the wrist. A single FDS tendon can be used to motorize up to three extensor tendons. If more than three extensors are ruptured, one should consider transfer of both the ring and long finger FDS tendons.
Step 2 Pearls
In patients with both ring and small finger extensor tendon ruptures, an EIP transfer is preferred to an end-to-side repair of the ring and small finger extensor tendons to the long finger extensor tendon because the oblique path of the transferred tendons could result in abduction of the small finger, causing functional problems.
When an FDS tendon is used as a motor, a subcutaneous transfer is preferred to one through the interosseous membrane to reduce the likelihood of adhesions.
It is preferable to transfer the FDS tendons on the radial side of the forearm because the direction of pull will help with correction of the ulnar deviation deformity.
If fusion of the thumb interphalangeal (IP) joint is being considered, it is important to check the strength of the intrinsic muscles and the condition of the MCP joint. A thumb IP joint fusion will be able to give satisfactory pinch strength only if the MCP joint is stable and functional.
Step 3: Imbricate the Lax Dorsal Wrist Capsule
Step 4: Tighten the Lax Extensor Tendons
Postoperative Care and Expected Outcomes
 If the distal ulna is excised, the patient should be placed in a supination splint for 4 weeks to allow healing of the dorsal capsular repair.
If the distal ulna is excised, the patient should be placed in a supination splint for 4 weeks to allow healing of the dorsal capsular repair.
 Fingers are kept in fully extended position for 4 weeks before initiating active range-of-motion exercises.
Fingers are kept in fully extended position for 4 weeks before initiating active range-of-motion exercises.
 With extensor tendon ruptures, the outcome of tendon transfer is good, although an increase in extension lags is observed when more tendons are involved.
With extensor tendon ruptures, the outcome of tendon transfer is good, although an increase in extension lags is observed when more tendons are involved.
 With flexor tendon ruptures, patients with isolated ruptures in the palm or at the wrist had the best functional results. Patients with multiple ruptures within the carpal canal had a worse prognosis.
With flexor tendon ruptures, patients with isolated ruptures in the palm or at the wrist had the best functional results. Patients with multiple ruptures within the carpal canal had a worse prognosis.
Chung US, Kim JH, Seo WS, Lee KH. Tendon transfer or tendon graft for ruptured finger extensor tendons in rheumatoid hands. J Hand Surg [Am]. 2010;35:279-282.
Ertel AN, Millender LH, Nalebuff E, et al. Flexor tendon ruptures in patients with rheumatoid arthritis. J Hand Surg [Am]. 1988;13:860-866.
Ishikawa H, Hanyu T, Tajima T. Rheumatoid wrists treated with synovectomy of the extensor tendons and the wrist joint combined with a Darrach procedure. J Hand Surg [Am]. 1992;17:1109-1117.
Moore JR, Weiland AJ, Valdata L. Tendon ruptures in the rheumatoid hand: analysis of treatment and functional results in 60 patients. J Hand Surg [Am]. 1987;12:9-14.