CASE 31


History: A 26-year-old woman presents with a 3-year history of crampy abdominal pain and bloody diarrhea.
1. Which of the following should be included in the differential diagnosis of the imaging findings? (Choose all that apply.)
2. Which of the following is characteristically absent in patients with acute ulcerative colitis?
D. Distal colonic distribution
3. Which inflammatory bowel disease (IBD) is most likely to cause fistulas to form?
4. Which IBD has the greatest risk for malignancy?
ANSWERS
CASE 31
Acute Ulcerative Colitis
1. B, C, and D
2. A
3. C
4. B
References
Gore RM, Balthazar EK, Ghahremani GG, Miller FH. CT features of ulcerative colitis and Crohn’s disease. Am J Roentgenol. 1996;167:3–15.
Thoeni RF, Cello JP. CT Imaging of colitis. Radiology. 2006;240:623–638.
Cross-Reference
Gastrointestinal Imaging: THE REQUISITES, 3rd ed, p 291-294.
Comment
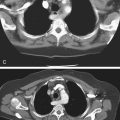
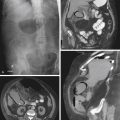
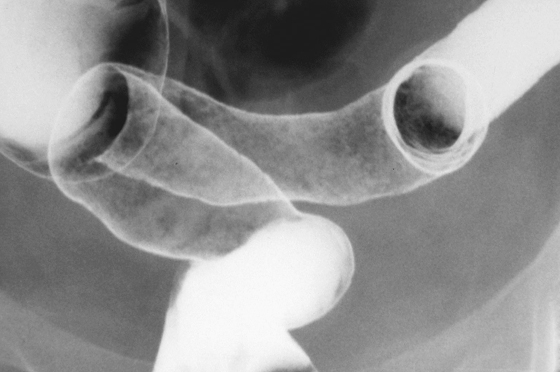
Ulcerative colitis (UC) is a superficial inflammatory disease usually affecting the distal colon. It begins as a granularity, hyperemia, and edema of the mucosa and progresses to multiple widespread evenly distributed tiny ulcerations (see figures). The patient presents with abdominal pain, diarrhea, and blood per rectum. The disease can disappear spontaneously, in which case one ought to reconsider the diagnostic possibilities, or it can go on to simmering chronic disease with occasional flare-ups. The entire colon may be involved in about a third of patients presenting with severe disease.
Differentiating between ulcerative colitis and Crohn’s disease can sometimes be very difficult clinically and histologically. Radiologic examinations can sometimes be more specific. In ulcerative colitis the disease starts distally and progresses proximally. The terminal ileum is never involved with UC, although it can appear patulous (backwash ileitis). The skip lesions and asymmetry seen in Crohn’s disease are not present in UC. The fistula formation commonly seen in Crohn’s disease is not seen with UC. Involvement of other parts of the gut, such as may be seen with Crohn’s disease, is never seen in UC. Extracolonic manifestations can be seen in both diseases. The risk for malignancy is much higher in UC than in Crohn’s disease.