Procedure 30 Synovectomy
Examination/Imaging
Clinical Examination
 Dorsal wrist: Extensor tendon synovitis can clearly be seen and palpated as a soft swelling on the dorsum of the wrist. Isolated dorsal tenosynovitis is painless. When patients with dorsal tenosynovitis complain of pain, one must look for involvement of the radiocarpal or radioulnar joints. Wrist mobility may be limited in this situation. It is also important to assess for the presence of ruptured extensor tendon and differentiate it from subluxation of the extensor tendons over the dorsum of the metacarpophalangeal (MCP) joints.
Dorsal wrist: Extensor tendon synovitis can clearly be seen and palpated as a soft swelling on the dorsum of the wrist. Isolated dorsal tenosynovitis is painless. When patients with dorsal tenosynovitis complain of pain, one must look for involvement of the radiocarpal or radioulnar joints. Wrist mobility may be limited in this situation. It is also important to assess for the presence of ruptured extensor tendon and differentiate it from subluxation of the extensor tendons over the dorsum of the metacarpophalangeal (MCP) joints.
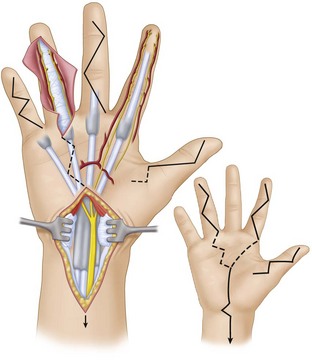
 Palmar aspect of hand: The presence of synovitis over the palmar aspect of the hand is indicated by the presence of (1) swelling (Fig. 30-1), (2) discrepancy between active and passive range of motion (Fig. 30-2), and (3) palpable crepitus along the course of the flexor tendon on active and passive flexion of the digit. This crepitus is best felt by asking the patient to flex the interphalangeal (IP) joints while applying some pressure over the tendon proximal to the A1 pulley of the flexor tendon sheath. The patient may also have triggering of the fingers. Flexor tendon ruptures occur infrequently compared with extensor tendon ruptures. One must also look for carpal tunnel syndrome as a result of proliferative synovitis within the carpal tunnel.
Palmar aspect of hand: The presence of synovitis over the palmar aspect of the hand is indicated by the presence of (1) swelling (Fig. 30-1), (2) discrepancy between active and passive range of motion (Fig. 30-2), and (3) palpable crepitus along the course of the flexor tendon on active and passive flexion of the digit. This crepitus is best felt by asking the patient to flex the interphalangeal (IP) joints while applying some pressure over the tendon proximal to the A1 pulley of the flexor tendon sheath. The patient may also have triggering of the fingers. Flexor tendon ruptures occur infrequently compared with extensor tendon ruptures. One must also look for carpal tunnel syndrome as a result of proliferative synovitis within the carpal tunnel.
Surgical Anatomy
 Synovitis is the hallmark of rheumatoid arthritis (RA), and, in the hand, it involves the synovial lining of the tendon sheath (tenosynovium) and the joint. Flexor tendons are covered by the tenosynovium under the carpal tunnel and in the digital flexor sheath, whereas extensor tendons are covered by tenosynovium only under the extensor retinaculum. Synovitis of the hand involves the extensor tendons more frequently than the flexor tendons.
Synovitis is the hallmark of rheumatoid arthritis (RA), and, in the hand, it involves the synovial lining of the tendon sheath (tenosynovium) and the joint. Flexor tendons are covered by the tenosynovium under the carpal tunnel and in the digital flexor sheath, whereas extensor tendons are covered by tenosynovium only under the extensor retinaculum. Synovitis of the hand involves the extensor tendons more frequently than the flexor tendons.
 Extensor tendon involvement is frequently seen over the dorsum of the wrist and results from synovitis progressing from the distal radioulnar joint and tenosynovitis under the extensor retinaculum. In contrast, the changes in the extensor tendon seen at the interphalangeal joints are caused by the underlying joint synovitis and not tenosynovitis.
Extensor tendon involvement is frequently seen over the dorsum of the wrist and results from synovitis progressing from the distal radioulnar joint and tenosynovitis under the extensor retinaculum. In contrast, the changes in the extensor tendon seen at the interphalangeal joints are caused by the underlying joint synovitis and not tenosynovitis.
 Three main groups of flexor tenosynovitis can be distinguished: isolated carpal tenosynovitis (20%), palmodigital tenosynovitis (50%), and diffuse tenosynovitis (30%). The index, long, and small fingers are most frequently involved. A flexor tendon rupture in the digital flexor sheath is almost always secondary to infiltrative synovitis and usually involves the flexor digitorum superficialis (FDS) at the proximal interphalangeal (PIP) joint. This is probably because the FDS splits into two slips in the distal third of the proximal phalanx. This decreases the thickness of the tendon and increases the surface area in contact with the invading synovium.
Three main groups of flexor tenosynovitis can be distinguished: isolated carpal tenosynovitis (20%), palmodigital tenosynovitis (50%), and diffuse tenosynovitis (30%). The index, long, and small fingers are most frequently involved. A flexor tendon rupture in the digital flexor sheath is almost always secondary to infiltrative synovitis and usually involves the flexor digitorum superficialis (FDS) at the proximal interphalangeal (PIP) joint. This is probably because the FDS splits into two slips in the distal third of the proximal phalanx. This decreases the thickness of the tendon and increases the surface area in contact with the invading synovium.
Tenosynovectomy
1 Digital Flexor Synovectomy
Exposures
 A Bruner type incision is made in the fingers extending onto the distal palm (Fig. 30-3).
A Bruner type incision is made in the fingers extending onto the distal palm (Fig. 30-3).
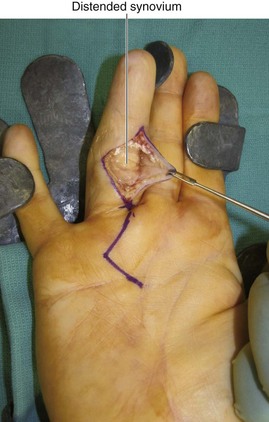
 The skin flaps are raised in a plane superficial to the flexor tendon sheath. This brings into view the sausage-shaped mass of distended synovium (Fig. 30-4).
The skin flaps are raised in a plane superficial to the flexor tendon sheath. This brings into view the sausage-shaped mass of distended synovium (Fig. 30-4).
Procedure
Step 1: Synovectomy
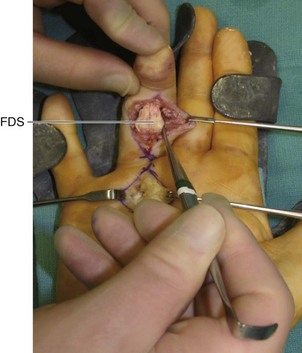
 Flexor tendon synovectomy is performed by pulling the FDS and flexor digitorum profundus (FDP) tendons alternatively through the openings in the tendon sheath. The area of tenosynovitis can then be excised from each tendon using a combination of sharp and blunt dissections (Fig. 30-5).
Flexor tendon synovectomy is performed by pulling the FDS and flexor digitorum profundus (FDP) tendons alternatively through the openings in the tendon sheath. The area of tenosynovitis can then be excised from each tendon using a combination of sharp and blunt dissections (Fig. 30-5).
Step 1 Pitfalls
The slips of the FDS may be infiltrated with tenosynovitis, and the surgeon may be tempted to excise the FDS tendon, which should be avoided because of the progressive nature of the disease. The FDS is the prime flexor of the PIP joint, and excising it may result in a swan neck deformity.
Care is taken not to injure the neurovascular bundles and resect the tendon pulleys accidentally.
Step 2: Checking Passive Range of Motion
 After the tenosynovectomy, the smooth gliding of tendons (FDS and FDP) is confirmed by flexion and extension of the fingers (Fig. 30-6).
After the tenosynovectomy, the smooth gliding of tendons (FDS and FDP) is confirmed by flexion and extension of the fingers (Fig. 30-6).
Step 2 Pearls
If surgery is performed with the patient under local anesthesia or a Bier block, active range of motion can be visualized and any residual diseased areas addressed.
If “catching” is found when testing for tendon excursion after tenosynovectomy, check for flexor tendon nodules in digits and/or palm.
If triggering of finger persists after tenosynovectomy, an A1 pulley release is performed.
Step 2 Pitfalls
The release of the A1 pulley may contribute to the MCP joint ulnar drift deformity, especially for the index and long fingers, because of the oblique line of pull of the long flexors for these digits. Some investigators recommend resection of one slip of the FDS to provide greater space for passage of the FDP instead of A1 pulley release.
Postoperative Care and Expected Outcomes
 A generously padded volar plaster of Paris slab extending to the fingertips is applied while maintaining the fingers in an intrinsic-plus posture and the wrist in moderate extension. The hand is kept elevated, and gentle mobilization is started in 4 to 7 days.
A generously padded volar plaster of Paris slab extending to the fingertips is applied while maintaining the fingers in an intrinsic-plus posture and the wrist in moderate extension. The hand is kept elevated, and gentle mobilization is started in 4 to 7 days.
 Digital flexor tenosynovectomy is a safe and effective method for restoring function to rheumatoid patients with flexor tenosynovitis to prevent further complications such as the flexor tendon rupture.
Digital flexor tenosynovectomy is a safe and effective method for restoring function to rheumatoid patients with flexor tenosynovitis to prevent further complications such as the flexor tendon rupture.
2 Flexor Synovectomy in the Carpal Tunnel and Distal Forearm
Exposures
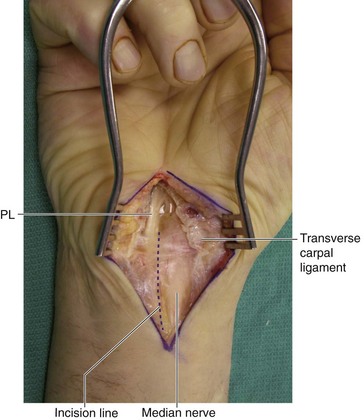
 An extended carpal tunnel incision is made (see Fig. 30-3). This longitudinal incision extends 2 cm distal to the wrist crease and 4 cm proximal to it. The distal limb of the incision is required only if a carpal tunnel release is indicated and is made parallel to the thenar crease. The proximal limb of the incision is made over the palmaris longus (PL). The limbs are connected by a transverse incision over the wrist crease.
An extended carpal tunnel incision is made (see Fig. 30-3). This longitudinal incision extends 2 cm distal to the wrist crease and 4 cm proximal to it. The distal limb of the incision is required only if a carpal tunnel release is indicated and is made parallel to the thenar crease. The proximal limb of the incision is made over the palmaris longus (PL). The limbs are connected by a transverse incision over the wrist crease.
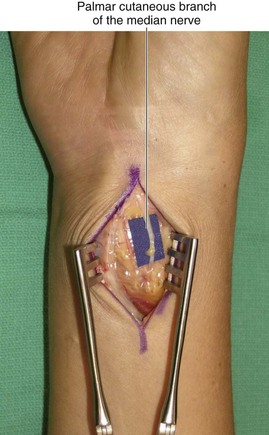
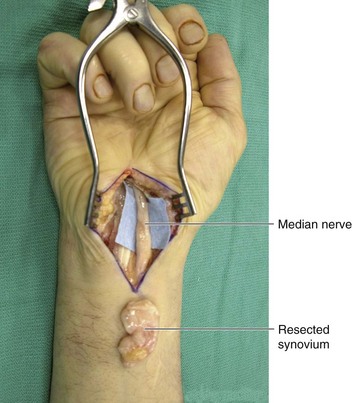
 The forearm fascia is divided ulnar to the PL to expose the median nerve and flexor tendons in the proximal portion of the incision. The subcutaneous fat is bluntly dissected to expose the transverse carpal ligament in the distal portion. The transverse carpal ligament is divided along its entire length (Fig. 30-7).
The forearm fascia is divided ulnar to the PL to expose the median nerve and flexor tendons in the proximal portion of the incision. The subcutaneous fat is bluntly dissected to expose the transverse carpal ligament in the distal portion. The transverse carpal ligament is divided along its entire length (Fig. 30-7).
Procedure
Postoperative Care and Expected Outcomes
 Postoperative immobilization is supported by a volar wrist splint in neutral position followed by immediate active finger motion.
Postoperative immobilization is supported by a volar wrist splint in neutral position followed by immediate active finger motion.
 Flexor tenosynovectomy with decompression of the nerve prevents permanent pain, numbness, thenar muscle loss, and spontaneous rupture, as well as preserving independent tendon gliding function.
Flexor tenosynovectomy with decompression of the nerve prevents permanent pain, numbness, thenar muscle loss, and spontaneous rupture, as well as preserving independent tendon gliding function.
3 Dorsal Wrist Synovectomy
Exposures
 An 8-cm dorsal longitudinal incision centered over the radiocarpal joint is made (Fig. 30-10).
An 8-cm dorsal longitudinal incision centered over the radiocarpal joint is made (Fig. 30-10).
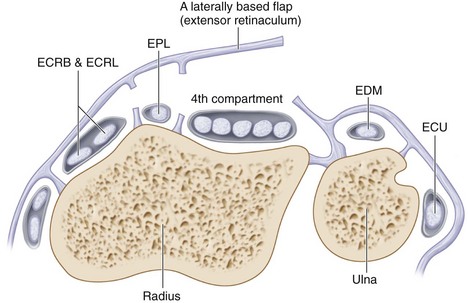
 Sharp dissection is carried down to the extensor retinaculum over the fourth compartment in this case.
Sharp dissection is carried down to the extensor retinaculum over the fourth compartment in this case.
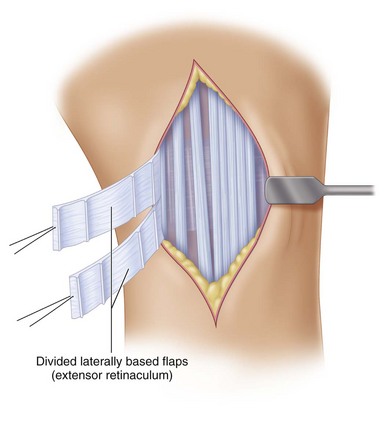
 The extensor retinaculum is incised longitudinally over the fourth compartment (Fig. 30-11). The vertical septae between the extensor compartments are divided, thus raising the retinaculum as a laterally based flap (Fig. 30-12). This exposes the extensor tendons and the hypertrophic synovium.
The extensor retinaculum is incised longitudinally over the fourth compartment (Fig. 30-11). The vertical septae between the extensor compartments are divided, thus raising the retinaculum as a laterally based flap (Fig. 30-12). This exposes the extensor tendons and the hypertrophic synovium.
Pearls
Care is taken to preserve the main longitudinal veins and not to injure branches of the radial sensory nerve.
When the retinaculum flaps are elevated, the first dorsal compartment is not opened unless it is involved significantly.
An alternative exposure involves elevating the extensor retinaculum as a radially based flap by opening it over the fourth or fifth compartment. This flap is divided into two flaps by splitting it transversely (Fig. 30-13). During closure, one flap is passed below the extensor tendons and the other above the tendons (Fig. 30-14). This approach provides a gliding bed for the tendons and creates a barrier between the tendons and the underlying bone and wrist joint.
Procedure
Step 1: Synovectomy
 Hypertrophic synovium is removed from the extensor tendons sharply with a no. 15 blade and occasionally with small scissors (Fig. 30-15).
Hypertrophic synovium is removed from the extensor tendons sharply with a no. 15 blade and occasionally with small scissors (Fig. 30-15).
Step 1 Pearls
As much of the diseased synovium is removed as possible, although it is sometimes necessary to leave material that is densely adherent to the extensor tendon surface to avoid disrupting the tendon substance.
Frayed areas of the tendons are repaired with interrupted 5-0 Ethibond braided sutures.
After a complete tenosynovectomy has been performed, the wrist joint is evaluated. If synovitis is present, the joint is opened, and a wrist synovectomy is performed.
Postoperative Care and Expected Outcomes
 The hand and wrist are immobilized in a bulky conforming dressing and volar plaster splint. The wrist is held in neutral and the MCP joint in extension to prevent extensor lag until active extension is possible. The IP joints are left free.
The hand and wrist are immobilized in a bulky conforming dressing and volar plaster splint. The wrist is held in neutral and the MCP joint in extension to prevent extensor lag until active extension is possible. The IP joints are left free.
 Hand motion is started 24 to 48 hours after surgery. Active extension and flexion exercises are emphasized. The wrist is supported with a volar splint for 2 weeks after the procedure.
Hand motion is started 24 to 48 hours after surgery. Active extension and flexion exercises are emphasized. The wrist is supported with a volar splint for 2 weeks after the procedure.
 Although the appearance of the tendons within the compartments affected by tenosynovitis may be poor (as evidenced by fraying), tendon rupture rarely occurs after dorsal tenosynovectomy is performed.
Although the appearance of the tendons within the compartments affected by tenosynovitis may be poor (as evidenced by fraying), tendon rupture rarely occurs after dorsal tenosynovectomy is performed.
Joints Synovectomy
1 Wrist Synovectomy
Exposures
 The first part is the same as for dorsal wrist synovectomy. After a complete tenosynovectomy has been performed, the wrist joint is evaluated. If synovitis is present, the joint is opened, and a wrist synovectomy is performed.
The first part is the same as for dorsal wrist synovectomy. After a complete tenosynovectomy has been performed, the wrist joint is evaluated. If synovitis is present, the joint is opened, and a wrist synovectomy is performed.
 If one needs to access the radiocarpal joint, the floor of third compartment is incised longitudinally, and if access to the distal radioulnar joint is required, the floor of the fifth compartment is opened.
If one needs to access the radiocarpal joint, the floor of third compartment is incised longitudinally, and if access to the distal radioulnar joint is required, the floor of the fifth compartment is opened.
Procedure
Step 1: Synovectomy
 The synovium in the joints is removed with a small, curved rongeur.
The synovium in the joints is removed with a small, curved rongeur.
 The dorsal aspects of the ulna and radius are examined, and any bony spicules, which might cause attrition ruptures, are removed with a rongeur.
The dorsal aspects of the ulna and radius are examined, and any bony spicules, which might cause attrition ruptures, are removed with a rongeur.
 The distal ulna is resected at the same time if it is dislocated and prominent dorsally (see Procedure 83).
The distal ulna is resected at the same time if it is dislocated and prominent dorsally (see Procedure 83).
2 Metacarpophalangeal Joint Synovectomy
Exposures
 A transverse incision is made over the head of the metacarpals for multiple MCP joint synovectomy and a longitudinal “lazy S”–shaped incision is used when a single joint is being addressed. The skin flaps are retracted to expose the extensor mechanism over the MCP joint.
A transverse incision is made over the head of the metacarpals for multiple MCP joint synovectomy and a longitudinal “lazy S”–shaped incision is used when a single joint is being addressed. The skin flaps are retracted to expose the extensor mechanism over the MCP joint.
 The radial sagittal band is divided 1 to 2 mm lateral to the extensor tendon, and the extensor mechanism is retracted. The dorsal capsules are incised transversely to expose the MCP joint.
The radial sagittal band is divided 1 to 2 mm lateral to the extensor tendon, and the extensor mechanism is retracted. The dorsal capsules are incised transversely to expose the MCP joint.
3 Proximal Interphalangeal Joint Synovectomy
Exposures
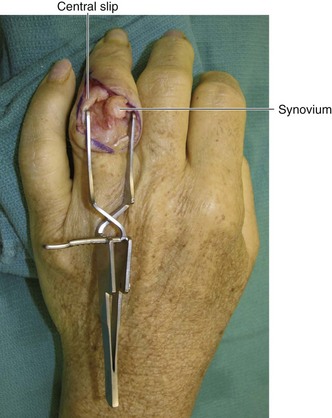
 A curvilinear longitudinal skin incision on the dorsum of the PIP joint is used. If synovial bulging is limited to one side, a lateral incision can be used. Skin flaps are elevated to expose the extensor mechanism.
A curvilinear longitudinal skin incision on the dorsum of the PIP joint is used. If synovial bulging is limited to one side, a lateral incision can be used. Skin flaps are elevated to expose the extensor mechanism.
 The joint can be approached either between the central slip and the lateral band or palmar to the lateral band, depending on the location of the disease. The joint is approached dorsal to the collateral ligament.
The joint can be approached either between the central slip and the lateral band or palmar to the lateral band, depending on the location of the disease. The joint is approached dorsal to the collateral ligament.
Tolat AR, Stanley JK, Evans RA. Flexor tenosynovectomy and tenolysis in longstanding rheumatoid arthritis. J Hand Surg [Br].. 1996;21:538-543.
Wheen DJ, Tonkin MA, Green J, Bronkhorst M. Long-term results following digital flexor tenosynovectomy in rheumatoid arthritis. J Hand Surg [Am].. 1995;20:790-794.