CASE 30


1. What should be included in the differential diagnosis? (Choose all that apply.)
B. Ventricular septal defect (VSD)
C. Patent ductus arteriosus (PDA)
D. Partial anomalous pulmonary venous connection (PAPVC)
2. What is the most likely diagnosis?
A. ASD
B. VSD
C. PDA
D. PAPVC
3. What lesion commonly causes enlargement of the left atrium?
A. VSD
B. ASD
C. PAPVC
D. Total anomalous pulmonary venous connection (TAPVC)
4. Which anomaly can manifest with cyanosis and shunt vascularity on chest radiographs?
B. PAPVC
D. TAPVC
ANSWERS
Reference
Higgins CB. Radiography of congenital heart disease. In: Webb WR, Higgins CB, eds. Thoracic Imaging: Pulmonary and Cardiovascular Radiology. ed 2 Philadelphia: Lippincott Williams & Wilkins; 2010.
Cross-Reference
Cardiac Imaging: The REQUISITES, ed 3, pp 340–342.
Comment
Radiography
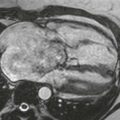
The chest radiographs demonstrate cardiomegaly and shunt vascularity (increased vascularity). The left atrium is enlarged, signifying that the shunt is beyond the atrial level. The aortic knob is normal in size, indicating that the most likely lesion in an acyanotic patient is a VSD. PDA typically causes dilation of the aortic knob. If a VSD is small, the chest radiograph is usually normal. However, if the left-to-right shunt is large, shunt vascularity is identified on chest films, and the central pulmonary arteries, both ventricles, and the left atrium are enlarged.
Cross-Sectional Imaging
Echocardiography usually demonstrates the location and size of the defect. MRI may be performed in certain patients to evaluate associated abnormalities or to define certain lesions such as a supracristal VSD, which may be difficult to image by echocardiography. Velocity-encoded cine phase contrast MRI can be performed to quantify the pulmonary-to-systemic flow ratio, which is an indicator of the severity of the shunt.