CHAPTER 3 Peripheral Mechanisms of Acupuncture
INTRODUCTION
Unique Biomedical Mechanisms of Acupuncture Needling
Sound physiologic bases for the scientific explanation of why and how acupuncture works have been already established by distinguished scientists. A prominent researcher in the field of acupuncture analgesia, Professor Bruce Pomeranz of the University of Toronto said, “We know more about acupuncture analgesia than about many chemical drugs in routine use. For example, we know very little about the mechanisms of most anesthetic gases but still use them regularly.”1
Why Patients Respond Differently to the Same Acupuncture Treatment
Using an innovative, well-defined, and reliable evaluation procedure as presented in this book (see Chapter 6), we can categorize patients into four groups of responders: excellent (Group A), good (Group B), average (Group C), and weak (Group D). Professor H.C. Dung2 discovered these important clinical phenomena after examining and treating 15,000 patients.
Integrative Neuromuscular Acupoint System (INMAS): The User-Friendly Protocol
Electrical Acupuncture
Endorphin mechanisms are nonspecific. EA and needling stimulate endorphin mechanisms, whereas chiropractic manipulation, massage, and physical exercises also lead to the secretion of endorphins. The mechanisms of EA are discussed in more detail in Chapter 15. The following discussion focuses on the unique local mechanisms of acupuncture needling.
GENERAL PRINCIPLES OF HEALING PROCESS INDUCED BY ACUPUNCTURE NEEDLING
Our clinical evidence shows that acupuncture is an effective modality in controlling inflammation. Needling and needle-induced lesions are foreign invaders to our body. Needling and its lesions stimulate and increase the number and the activity of immune cells and control the inflammatory process (see Chapter 4), which reduces both acute and chronic inflammation.
NEEDLING AND DE QI SENSATION
The needling process includes the following procedures:
During procedure no. 3, a needle can be manipulated by unidirectional or bidirectional (i.e., clockwise or counterclockwise) rotation or “pistoning” (up and down motion). This manipulation creates winding of connective tissue around the needle, which makes the practitioner feel the needle being grasped by body tissue.3
Once the needle has punctured the deeper tissues, especially the muscles, the patient will feel nonpainful sensations termed de qi (deh chee) in traditional Chinese acupuncture, which means that qi (i.e., the vital energy flow) has obtained or arrived. About 90% of needling will produce some sort of de qi sensation, depending on the nerve fibers encountered by needling and surrounding tissue milieu, such as tissue perfusion and inflammatory mediators.4 Needling the points on limbs may produce a de qi sensation of brief electric shock running up or down along the entire length of the limb. When needling the points on the back, a de qi sensation could be experienced more as localized sensations, like deep aching, soreness, and heaviness.
The phenomenon of de qi sensations can be explained by the types of nerve fibers stimulated by the needling (Table 3-1). Types II, III, and IV muscular afferent fibers not only generate de qi, but they also produce pain sensation if they are injured or pathophysiologically excited; so they represent de qi and pain-transmission nerves. Patients should be warned that some needling sensations such as aching or soreness may last 1 or 2 days.
Table 3-1 De Qi Sensation and Its Related Nerve Fibers in the Muscles
| Types of Afferent Nerve Fibers | Types of Sensation |
|---|---|
| Type II | Numbness |
| Type III | Heaviness, distention, pressure, compression, aching |
| Type IV (unmyelinated) | Soreness, tingling, pain |
The following local chain reactions are started right after needling:
LOCAL SKIN REACTION AND CUTANEOUS MICROCURRENT MECHANISM
When an acupoint transits from latent phase (normal tissue) to passive phase, it becomes tender (Chapter 2). Around a tender acupoint the skin electrical conductance increases and the resistance decreases as discussed in Chapter 2. Inserting a needle into this acupoint will provoke an acute local inflammatory defensive response from all the previously mentioned tissues. The first visible response is the flare response, resulting in the appearance of redness around the needle. This vasodilatation function of the autonomic nervous system (ANS) is mediated by substance P secreted by cutaneous nociceptive sensory nerves. Then the immune reaction is triggered by mast cells, which produce histamine, platelet activating factor (PAF), and leukotrienes. The needle-induced lesion simultaneously activates interaction between the blood coagulation system and the immune complement system.
The body surface wears a layer of electric charges because the human body bathes in the electromagnetic field of the earth. Normally, dry skin has a DC resistance in the order of 200,000 to two million ohms. At acupuncture points this resistance is down to 50,000 ohms.5 Melzack and Katz6 found no difference in conductance between acupuncture points and nearby control points in patients with chronic pain.
This phenomenon can be explained by the dynamic nature of the acupoints. In a healthy person, DC resistance of the acupoints is the same as that of nonacupoints. In a chronically sick person, the acupoints transit from the latent phase (healthy tissue) to the passive phase (tender or sensitized tissue) in a predictable sequence and location (see Chapter 2). The sensitive area of acupoints is getting larger in chronic conditions, which contributes to high electrical conductance and low resistance.
In acute injury, acupoints appear around injured tissue. There is 20 to 90 mV of resting potential across the intact human skin, outside negative and inside positive.7 Most acupoints are measured at 5 mV higher than in nonacupoint areas.5 This higher voltage at acupoint loci can be explained histologically and pathologically. The configuration of most acupoints is rich in nerve fibers and/or vasculolymphatic structures, and once sensitized, inflammation may accumulate more fluids in the tissues of an acupoint. All these conditions may increase conductance and compensate the loss of resistance at acupoint loci according to Ohm’s formula: V = IR.
Insertion of a metal needle makes a short circuit from the skin battery and thus creates a microcurrent, called a current of injury, moving from inside to outside. The tiny lesion created by an acupuncture needle causes negativity at the needling site and produces 10 mA of current of injury, which benefits tissue growth and regeneration.8
These microcurrents induced by the needling are not sufficient to initiate nerve pulses to the spinal cord; thus the microcurrents will not generate effects of “needling tolerance” like “morphine tolerance,” meaning that repetitive needling will not reduce its therapeutic effect. In case of electroacupuncture stimulation of more than 3 hours’ duration, the analgesic effect will gradually decline. Professor J.S. Han of the Beijing Medical University explained that possibly long-lasting electrical stimulation, especially with high frequencies such as 100 Hz, increases the release of cholecystokinin octapeptide (CCK-8), which is an endogenous antiopioid substance.9
NEEDLE MANIPULATION: MECHANICAL SIGNAL TRANSDUCTION THROUGH CONNECTIVE TISSUE
The research team of the University of Vermont College of Medicine demonstrated that manipulation promotes tissue healing by producing biomechanical, vasomotor, and neuromodulatory effects on interstitial connective tissue.3
When a needle is inserted into the body tissue, there is an initial coupling between the metal needle shaft and elastic/collagen fibers. This initial affinity is caused by both surface tension and electrical attraction between the metal needle and connective tissue charges. Once this wrapping has occurred, frictional force takes over. Then rotation of the needle increases the tension of the fibers by winding them around the needle, which pulls and realigns the connective fiber network
In response to this mechanistic deformation, cells generate cascades of cellular and molecular events, including intracellular cytoskeletal reorganization, cell contraction and migration, autocrine release of growth factors, and activation of intracellular signaling pathways and of nuclear binding proteins that promote the transcription of specific genes. These effects lead to the synthesis and local release of growth factors, cytokines, vasoactive substances, degradative enzymes, and structural matrix elements. Release of these substances changes the extracellular milieu surrounding needled tissues and finally promotes local healing. These effects may expand to distant connective tissues to spread the healing process with long-term effects. Thus mechanical signals produced by simple needle manipulations generate cascades of downstream physiologic healing effects.10
LOCAL RELIEF OF CONCURRENT MUSCLE SHORTENING AND CONTRACTURE
Repetitive strain or overuse injuries are common muscle activities that result in local muscle pain. If muscles are used for repetitive movement without adequate recovery time between movements or are held under a load in a relatively fixed position for prolonged periods, discomfort, soreness, or pain will develop following those activities, with peak discomfort during the first day or two. Pain makes muscles tender to palpation, restricted in range of motion, and sometimes slightly swollen. With this type of injury, some disorganization of striation of muscle fibers can occur, and a lack of myofibrillar regeneration could persist for up to 10 days.11 Changes in blood chemistry have been noticed, including increases in plasma interleukin-1, acid-reactive substances, lactic dehydrogenase, serum creatine, phosphokinase, aspartate aminotransferase, and serum glutamic-oxaloacetic transaminase. Most of these enzymes are involved in muscle metabolism.
Joint diseases and dysfunction can cause muscle pain. Because of the segmental reflex, the activity of sensory nerves influences the activity of efferent nerves from motor neurons of the same muscle; however, the sensory nerves of neighboring muscles and joints also affect this muscle. Stimulation of knee joint nociceptors excites afferent motor neurons of both flexor and extensor muscles.12 It is possible that sensory input from a joint will lead to a contraction in neighboring muscles. Then the contracted muscles may put physical stress on the joint and its accessory structures, such as capsules, ligaments, and disks. All these structures will produce pain because they are richly innervated by sensory nerves.
Acupoints have different histologic composition and pathophysiologic phases (Chapters 1 and 2). Some acupoints consist mostly of sensitized nerve fibers; others, in addition to the sensitized nerve receptors, contain muscle contraction knots. Internal factors, such as diseased organs and arthritis, will sensitize acupoints all over the body. Remarkably their locations are highly predictable, partly because of a segmental mechanism or special tissue features associated with sensory nerve fibers. During acute injuries sensitized spots are provocatively formed according to the type of injury and body anatomy involved. For example, the mild ankle sprain (inversion injury) causes only elongation of ligaments on the lateral ankle, whereas a severe ankle injury may tear the ligaments between the fibula and tibia in addition to the lateral ligaments. Knowing anatomy helps in locating the most effective tender points for treatment. (To help locate the effective acupoints, the clinical chapters of this book describe some of the neuromusculoskeletal anatomy in relation to body mechanics.)
The muscle, tendon, or fascia that harbors tender or painful points may resist stretch and become tense, stiff, shortened, and painful. Most acupoints used for pain treatments are of muscular nature as discussed in Chapter 1.
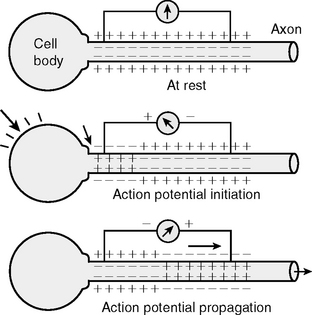
Depolarization can be described as follows. When a cell is not agitated, the outside of the cell membrane is electrically positive, the inside negative. When electric impulses or bioactive molecules stimulate the cell, positive Na+ ions flow into the cell through the membrane so that the outside becomes less positive; this means the electricity flows into the cell. Then positive K+ ions flow out from inside to restore positive polarity of the outside, which means that positive electricity flows out from the inside. Finally Na+ ions are pumped out and K+ ions are pumped in by molecular channels; so the concentration of Na+ ions outside and K+ inside is restored. This represents one cycle, and the process is called depolarization (Figure 3-1). The depolarization consumes metabolic energy.
All five steps of muscle contraction are related to depolarization and consumption of energy:
Now we compare the same steps of pathologic contraction with physiologic contraction. This process was discussed in Chapter 2, but is briefly reviewed here because it is an important mechanism in clinical acupuncture practice. Dr. D.G. Simons explained this process and called it the energy crisis hypothesis.”13 We modify his hypothesis as follows (also see Figure 2-2, p. 22).
Thus the ischemia, hypoxia, low energy supply, and muscle shortening will continue and become a vicious circle (see Figure 2-2, p. 22) until appropriate treatment interrupts the vicious circle of energy crisis. The muscle contracture during such an energy crisis has a higher temperature than normal muscle tissue does. This pathologic contraction is an endogenous, not voluntary, impulse initiated and may persist indefinitely. Clinical experience shows that any method that interrupts the energy crisis will help relax the muscle and reduce muscle pain. Needling, electrical stimulation, physical stretch, proper exercise, and drug injection are effective procedures used to break the energy-consuming vicious circle and to separate actin from myosin to relax the shortened muscle.
NEUROCHEMICAL MECHANISMS OF ACUPUNCTURE ANALGESIA
Recently Professor Zang Hee Cho and his research team at the University of California, Irvine, cooperated with Tian Tan Hospital in Beijing and have obtained new evidence by using functional magnetic resonance imaging (fMRI) techniques (Chapter 4). Our explanation of AA mechanisms is oversimplified for the purpose of this textbook. For example, after pain impulses reach the spinal cord, at least six neural pathways transmit those impulses from the spinal cord to the cerebral cortex, and numerous neurochemicals are released at different sites to modulate pain signals, such as three different endorphins (enkephalin, beta-endorphin, and dynorphin), cholecystokinin (CCK), serotonin, adrenocorticotrophic hormone (ACTH), SOM, substance P, vasoactive intestinal peptide (VIP), neurotensin, CGRP, gamma-aminobutyric acid (GABA), and more. Detailed description of these interactions among the neurochemicals is beyond the scope of this clinical textbook. More detailed discussions are provided in Chapter 4.
The quantitative nature of acupoint physiology discussed in previous chapters is the basis for our evaluation method and treatment protocol. Clinically we first select two types of acupoints (Chapter 5), local and distant, or symptomatic and homeostatic points. Local points are located in painful tissues and are more sensitive or are painful. In chronic cases these sensitized local points may stimulate neurons inside the spinal cord; they synapse with and finally sensitize those spinal neurons.14
Thus, when we stimulate the symptomatic acupoints, we also stimulate the sensitized neurons in the same segment of the spinal cord. This means we stimulate segmental circuits when we select local points. Distant points are located far from those local points, and their tenderness represents a homeostatic imbalance (Chapter 2).
Close attention should be directed to the phenomenon that homeostatic acupoints (HAs) become tender in a predictable sequence all over the body when homeostasis declines.2 Everyone, including healthy persons, has a certain number of tender HAs all over the body. The difference between the healthy and the less healthy bodies is that the healthy ones have fewer tender HAs and the less healthy ones have more tender HAs. Those points, representing homeostatic changes, appear in predictable locations. In chronic cases more tender points are distributed all over the body. In a healthy person with an acute injury, tender points appear locally around the injured area. Clinically segmental (local) treatment may suffice for acute injuries, but both segmental (local or symptomatic) and nonsegmental (distal or homeostatic) points should be used for chronic symptoms to achieve optimal self-healing. Now it is clear that when we place needles into local painful points, AA is produced through segmental mechanism. If we use distal points, AA works through a nonsegmental mechanism. These mechanisms enhance one another.
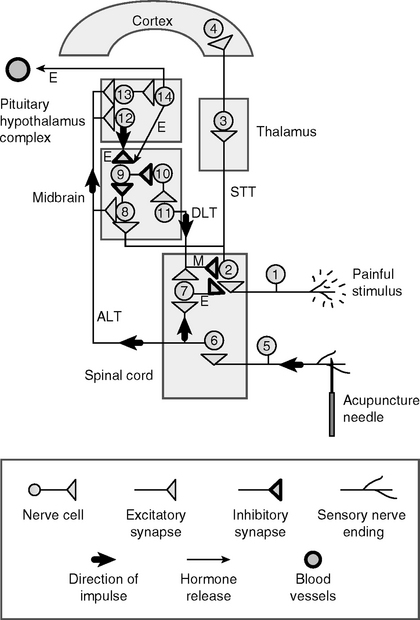
Neural mechanisms in AA can be explained step by step as shown in Figure 3-2. Pain (cell 1) sends messages to the spinal cord, where they are relayed up through pathways (cell 2) to the brain centers, thalamus, and cortex; these messages are perceived as pain (see Chapter 4). When we use acupuncture to treat this pain, we select both local (segmental circuit) and distal (nonsegmental circuit) acupoints. Wherever we insert a needle into a patient’s body, the needling stimulates afferent sensory receptors of small-diameter nerves in the skin and muscles, as discussed previously (cutaneous A-delta and C fibers, muscular type III and IV fibers, sometimes type II fibers).
Finally the needling signals generate neuronal activities in the highest brain level, the neocortical area. Professor Zang-Hee Cho and his research team provided the first scientific evidence for this central processing.15 This cortical processing is responsible for the modulation of pain perception.
BLOOD COAGULATION SYSTEM AND IMMUNE COMPLEMENT SYSTEM
A needle-induced lesion is a minute trauma to the tissue cells and mostly causes invisible tiny internal bleeding. This lesion activates the restorative control mechanisms involving the neuroendocrine-cardiovascular–mediated immune response, and thus promotes tissue healing and homeostatic restoration, resulting in systemic healing of the whole body in addition to local healing of the pathological symptoms.
When the needle is removed, tissue repair processes are stimulated, lesioned cells are digested, and protein synthesis is mobilized. The lesion-induced healing is directed by systemic neurohormonal mechanisms. The pituitary starts to increase the blood volume of ACTH, which triggers synthesis and the secretion of physiologic corticosteroids and other hormones. This process protects the body from stress, including reduction of the inflammatory reaction (see Chapter 4). Descending neural control systems from the brain inhibit and desensitize the nociceptive neurons in the spinal cord and peripheral nerve endings, and balance the ANS, which normalizes blood flow and energy metabolism. Finally the body’s homeostasis is improved or restored and local tissue healing and pain relief are accelerated.
SUMMARY
Patients respond differently to acupuncture treatments because of their physiological differences. About 28% of the clinic population are excellent responders, 64% good and average responders, and 8% weak or nonresponders.2
Differentiation of patients and prediction of prognosis are important parts of the treatment procedure in acupuncture therapy. Understanding the needling mechanisms facilitates development of a practical protocol for all pain symptoms. Our INMAS protocol (see Chapter 5) simplifies the process of point selection. INMAS provides a standardized protocol required by Western medicine and ensures the personalized treatment practiced in TCM. Our 16-point quantitative evaluation method provides a generally predictable prognosis of pain management.
This chapter discusses the peripheral effects of acupuncture stimulation. Chapter 4 presents a discussion of the central effects of acupuncture stimulation. To help understand both peripheral and central mechanisms, a brief outline of both mechanisms is provided here.
The central effects of acupuncture stimulation activate the four front lines of homeostasis: (1) the nervous system, (2) the immune system, (3) the endocrine system, and (4) the cardiovascular system controlled by neural pathways such as the ANS, especially the vagus nerve pathway. These built-in homeostatic survival mechanisms are discussed briefly in Chapter 4.
All the available scientific data definitely support and justify the INMAS (see Chapter 5) and its clinical application. Both laboratory and clinical data match and agree with each other. The following points explain how the fMRI data support clinical procedures.
Acupoints are neurogenic. Stimulation of any sensory and postganglionic nerve endings in the body produces analgesic effects both locally and systemically. Nevertheless, certain acupoints associated with certain nerve structures such as major nerve trunks or other particular anatomic configurations (see Chapters 1 and 2) produce more effective analgesia or therapeutic results. The 24 HAs listed in Chapter 5 (also see the inside cover) are such acupoints. These 24 HAs represent the most important acupoints in the classic meridian system and contain the major features of neuromuscular configurations. In plain language, as Professor Cho said in a Newsweek interview, “We may find that one well-placed needle can do what we now do with 20.”16 In Chapter 4, readers will find that in fMRI experiments, stimulation of both homeostatic acupoint H5 deep peroneal (Liv 3, Taichong) and a “sham” acupoint produce analgesic effects, but H5 reduces more pain signals in the cerebral cortex.
Clinically we should select the acupoints that are able to produce more AA effects. fMRI data (see Chapter 4) and electrophysiologic data (Ma, Y.-T., unpublished) indicate that, at least in AA, stimulation of any acupoint activates similar analgesic effects at supraspinal levels, such as in the midbrain and cortices. This means that any randomly selected acupoint may produce pain relief. However, symptomatic acupoints activate both peripheral and central analgesic mechanisms, whereas distal points such as distal homeostatic acupoints activate mostly central analgesic mechanisms. Thus it is very important to select more effective SAs. To achieve this, a clinician should have a practical knowledge of pathophysiology, anatomy, and body mechanics. We have provided this basic knowledge in the clinical chapters.
Clinical data also suggest that 24 HAs produce AA in more than 92% of all patients (see Chapter 6) with different pain symptoms. Application of these 24 HAs simplifies clinical procedure while providing sufficient AA effects.
Both fMRI and clinical data agree in that stimulation of any sensory nerve endings produces AA effects in the spinal cord and brain. The difference among the stimuli to different acupoints is that some points produce more AA effects than others. In clinical practice, however, practitioners need to consider the segmental nature when selecting some acupoints (see Chapter 5). For example, when treating elbow problems, PAs along C4-T1 are selected because SAs in the elbow and PAs along C4-T1 belong to the same spinal segments. In the same way, paravertebral acupoints along L2-L5 are selected for treating knee pain. These combinations of SAs (such as in the elbow or the knee) with PAs are based simply on the segmental innervation of the spinal nerves.
1 Pomeranz B. Acupuncture analgesia—basic research. In: Stux G, Hammerschlag R, editors. Clinical acupuncture scientific basis. Berlin: Springer, 2001.
2 Dung HC. Physiology in acupuncture. In: Anatomical acupuncture. San Antonio, Texas: Antarctic Press; 1997.
3 Langevin HM, Yandow JA. Relationship of acupuncture points and meridians to connective tissue planes. Anat Rec. 2002;269(6):257-265.
4 Levine JD, Fields HL, Basbaum AI. Peptides and the primary afferent nociceptor. J Neurosci. 1993;13:2273-2286.
5 Becker O, et al. Electrophysiological correlates of acupuncture points and meridians. Psychoenergetic Systems. 1976;1:195-212.
6 Melzack R, Katz J. Auriculotherapy fails to relieve chronic pain. JAMA. 1984;251:1041-1043.
7 Jaffe L, et al. The glabrous epidermis of cavies contains a powerful battery. Am J Physiol. 1982;242:R358-R366.
8 Pomeranz B. Effects of applied DC fields on sensory nerve sprouting and motor nerve regeneration in adult rats. In: Nuccitelli R, editor. Ionic currents in development. New York: Alan R Liss, 1986.
9 Han JS, Tang J, Huang BS. Acupuncture tolerance in rats: antiopiate substrates implicated. Chin Med J. 1979;92:625-627.
10 Langevin HM, Churchill DL, Cipolia M. Mechanical signaling through connective tissue: a mechanism of the therapeutic effect of acupuncture. FASEB J. 2001;15:2275-2282.
11 O’Reilly KP, Warhol MJ, Fielding RA, et al. Eccentric exercise-induced muscle damage impairs muscle glycogen repletion. J Appl Physiol. 1987;63:252-256.
12 He X, Proske U, Shcaible H-G, et al. Acute inflammation of the knee joint in the cat alters responses of flexor motoneurons to leg movements. J Neurophysiol. 1988;59:326-340.
13 Simons DG. Referred phenomena of myofascial trigger points. Vecchiet L, et al, editors. Pain research and clinical management: New trends in referred pain and hyperalgesia, vol 27. Amsterdam: Elsevier, 1993.
14 Dubner R, Ruda MA. Activity dependent neuronal plasticity following tissue injury and inflammation. Trends Neurosci. 1992;15:96-103.
15 Cho Z-H, et al. Functional magnetic resonance imaging of the brain in the investigation of acupuncture. In: Stux G, Hammerschlag R, editors. Clinical acupuncture. Berlin: Springer, 2001.
16 Cowley G: Now, ‘integrative’ care, Newsweek December 2, 2002, p. 50