Procedure 3 Nail Bed Repair
Indications
Examination/Imaging
Clinical Examination
 Complete sensory examination before anesthesia.
Complete sensory examination before anesthesia.
 Note pattern of nail bed laceration (simple/stellate), involvement of germinal matrix, and dorsal roof matrix. (Fig. 3-3 shows a crush injury of the right thumb with a stellate laceration involving the sterile and germinal matrices.)
Note pattern of nail bed laceration (simple/stellate), involvement of germinal matrix, and dorsal roof matrix. (Fig. 3-3 shows a crush injury of the right thumb with a stellate laceration involving the sterile and germinal matrices.)
 Look out for associated subtotal pulp amputation (Fig. 3-4).
Look out for associated subtotal pulp amputation (Fig. 3-4).
Surgical Anatomy
 The nail is a hard structure composed of desiccated, keratinized, squamous cells attached to the nail bed and is the end product of the nail bed’s generative efforts. The nail is loosely attached to the germinal matrix but is densely adherent to the underlying sterile matrix and the eponychium.
The nail is a hard structure composed of desiccated, keratinized, squamous cells attached to the nail bed and is the end product of the nail bed’s generative efforts. The nail is loosely attached to the germinal matrix but is densely adherent to the underlying sterile matrix and the eponychium.
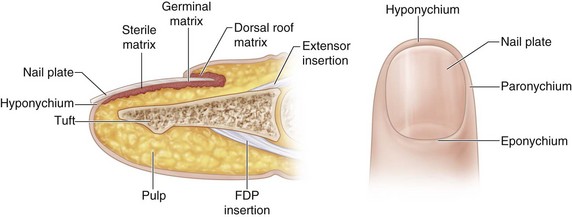
 The nail bed is composed of sterile matrix, germinal matrix, and dorsal roof matrix (Fig. 3-6).
The nail bed is composed of sterile matrix, germinal matrix, and dorsal roof matrix (Fig. 3-6).
 The portion of nail bed beyond the lunula is the sterile matrix. The sterile matrix acts as a road bed for the advancing nail. It adds squamous cells to the nail, making it thicker, stronger, and adherent to the bed. Firm adhesion of the nail to the nail bed is essential to the function of the fingertip.
The portion of nail bed beyond the lunula is the sterile matrix. The sterile matrix acts as a road bed for the advancing nail. It adds squamous cells to the nail, making it thicker, stronger, and adherent to the bed. Firm adhesion of the nail to the nail bed is essential to the function of the fingertip.
 The germinal matrix is the region of the nail bed proximal to the lunula and responsible for production of the nail plate.
The germinal matrix is the region of the nail bed proximal to the lunula and responsible for production of the nail plate.
 The dorsal roof matrix is the dorsal portion of the nail bed and is responsible for the luster of the nail plate.
The dorsal roof matrix is the dorsal portion of the nail bed and is responsible for the luster of the nail plate.
Exposures
 A Freer elevator is inserted between the nail plate and the nail bed distally and used to elevate the nail plate off the nail bed from distal to proximal.
A Freer elevator is inserted between the nail plate and the nail bed distally and used to elevate the nail plate off the nail bed from distal to proximal.
 Nail bed lacerations that extend under the nail fold or involve the germinal matrix require elevation of the dorsal roof matrix to expose the laceration and allow a good repair. This is done by making two oblique incisions at the corner of the nail fold and elevating the dorsal roof matrix as a proximally based flap. Two sutures at either corner maintain the flap in position (Fig. 3-7).
Nail bed lacerations that extend under the nail fold or involve the germinal matrix require elevation of the dorsal roof matrix to expose the laceration and allow a good repair. This is done by making two oblique incisions at the corner of the nail fold and elevating the dorsal roof matrix as a proximally based flap. Two sutures at either corner maintain the flap in position (Fig. 3-7).
Pearls
In children, general anesthesia is required to facilitate a meticulous repair.
If the laceration involves only the distal portion of sterile matrix, the nail plate needs to be elevated only 1 to 2 mm beyond the laceration.
Examine the undersurface of the nail for any nail bed remnants. They can be used as a free graft.
When the dorsal roof matrix flap is sutured back, it is important to ensure that the suture passes through the full thickness of the tissue.
Procedure
Step 1
Step 2
Step 2 Pearls
A slight gap is preferable to a tight nail bed repair.
A nail bed graft needs to be considered if there is loss of nail bed or there is a gap larger than 4 to 5 mm in the sterile matrix. A split-thickness sterile matrix graft can be harvested from the great toe without much donor morbidity. A gap in or loss of the germinal matrix is difficult to reconstruct. A sterile matrix graft will not replace the function of the germinal matrix. A germinal matrix graft from the toes will cause loss of nail growth in the toes, and the result at the finger may not be successful. It may be reasonable to consider an amputation of the digit proximal to the germinal matrix. An option in patients desiring germinal matrix reconstruction is transfer of toe pulp, using the nail complex as a free flap.
In severely comminuted stellate nail bed lacerations, it is better to approximate the multiple nail bed flaps with a few strategic sutures instead of attempting an anatomic repair (Fig. 3-9). Good results have been reported with the use of cyanoacrylate glue (Dermabond) in the suturing of such lacerations (Fig. 3-10).
Step 3
 The nail is replaced into the nail fold. A figure-of-eight suture or a simple suture from the nail to hyponychium can be used to hold the nail in place.
The nail is replaced into the nail fold. A figure-of-eight suture or a simple suture from the nail to hyponychium can be used to hold the nail in place.
 This nail serves as a splint for tuft fractures and undisplaced shaft fractures that cannot be or have not been pinned. The nail also prevents the dressing from adhering to the nail bed repair and makes dressing change less painful. Finally, the nail prevents adhesion (synechia) formation between two adjacent injured epithelial surfaces in cases in which the nail bed laceration involves both the germinal matrix and the dorsal roof matrix.
This nail serves as a splint for tuft fractures and undisplaced shaft fractures that cannot be or have not been pinned. The nail also prevents the dressing from adhering to the nail bed repair and makes dressing change less painful. Finally, the nail prevents adhesion (synechia) formation between two adjacent injured epithelial surfaces in cases in which the nail bed laceration involves both the germinal matrix and the dorsal roof matrix.
Step 3 Pearls
A couple of holes should be made in the nail using an 18-gauge needle. This provides space for blood to drain (after the tourniquet is released).
If the nail is unavailable or crushed, a sterile artificial silicone nail or a suture package cut in the shape of the nail can be placed within the nail fold (Fig. 3-11). One should remember to make holes for drainage in these nail inserts also.
The nail or an artificial splint should be placed into the nail fold for all lacerations involving the germinal matrix.
Procedure
Germinal Matrix Avulsion
Step 1
 A transverse laceration of the germinal matrix at the proximal end of the nail bed (at the junction with the dorsal roof matrix) is referred to as an “avulsion of the germinal matrix.” This distally based flap of germinal matrix prolapses out of the nail fold (Fig. 3-12). It is occasionally associated with a displaced fracture of the base of the distal phalanx and prevents closed reduction of the fracture.
A transverse laceration of the germinal matrix at the proximal end of the nail bed (at the junction with the dorsal roof matrix) is referred to as an “avulsion of the germinal matrix.” This distally based flap of germinal matrix prolapses out of the nail fold (Fig. 3-12). It is occasionally associated with a displaced fracture of the base of the distal phalanx and prevents closed reduction of the fracture.
 The nail bed flap needs to be reduced back into the nail fold and the reduction maintained with a splint in the nail fold.
The nail bed flap needs to be reduced back into the nail fold and the reduction maintained with a splint in the nail fold.
Step 2
 A more secure method of maintaining reduction is to elevate the dorsal roof matrix as a flap, as previously described.
A more secure method of maintaining reduction is to elevate the dorsal roof matrix as a flap, as previously described.
 A 5-0 nonabsorbable suture is passed from the dorsum (at the level of the proximal end of the nail bed), a horizontal bite of the nail bed is taken, and the suture is bought back out onto the dorsum. It is then held by a mosquito forceps.
A 5-0 nonabsorbable suture is passed from the dorsum (at the level of the proximal end of the nail bed), a horizontal bite of the nail bed is taken, and the suture is bought back out onto the dorsum. It is then held by a mosquito forceps.
Management of Associated Distal Phalangeal Fracture
 Fractures should be fixated before nail bed repair.
Fractures should be fixated before nail bed repair.
 It is not necessary to fixate distal tuft fractures or very comminuted fractures. The repair of the nail bed and an external split provide adequate stability for most fractures.
It is not necessary to fixate distal tuft fractures or very comminuted fractures. The repair of the nail bed and an external split provide adequate stability for most fractures.
 Minimal preliminary shortening of the fracture ends can permit easy nail bed repair in cases in which the nail bed repair is expected to be tight.
Minimal preliminary shortening of the fracture ends can permit easy nail bed repair in cases in which the nail bed repair is expected to be tight.
 It is better to pin unstable fractures (e.g., transverse fracture between the terminal extensor and flexor insertions). (Figure 3-14 shows intraoperative and late postoperative radiographs of the patient in Figures 3-3 and 3-5.)
It is better to pin unstable fractures (e.g., transverse fracture between the terminal extensor and flexor insertions). (Figure 3-14 shows intraoperative and late postoperative radiographs of the patient in Figures 3-3 and 3-5.)
 Retrograde pinning of the fracture through the fracture site (approached via the nail bed laceration) allows accurate placement of the K-wire.
Retrograde pinning of the fracture through the fracture site (approached via the nail bed laceration) allows accurate placement of the K-wire.
 A “bamboo split” type of longitudinal fracture can be temporarily stabilized by passing two to three loops of 3-0 or 4-0 absorbable suture (PDS) around the phalanx as a cerclage.
A “bamboo split” type of longitudinal fracture can be temporarily stabilized by passing two to three loops of 3-0 or 4-0 absorbable suture (PDS) around the phalanx as a cerclage.
 Trephination of a closed subungual hematoma associated with a fracture should be approached with care. This converts what was initially a closed fracture into an open fracture. It is preferable to drain the hematoma by an open approach by elevation of the nail, irrigation, and nail bed repair.
Trephination of a closed subungual hematoma associated with a fracture should be approached with care. This converts what was initially a closed fracture into an open fracture. It is preferable to drain the hematoma by an open approach by elevation of the nail, irrigation, and nail bed repair.
Postoperative Care and Expected Outcomes
 A nonadherent dressing covered by sterile gauze over a finger dressing is applied.
A nonadherent dressing covered by sterile gauze over a finger dressing is applied.
 A finger splint that immobilizes the distal interphalangeal joint is provided for patients with a tuft or distal phalanx fracture.
A finger splint that immobilizes the distal interphalangeal joint is provided for patients with a tuft or distal phalanx fracture.
 Patients are told that the nail or artificial nail splint may fall out after 2 to 3 weeks as the new nail starts to grow. Complete nail regeneration takes about 4 to 6 months, and the first-generation nail lacks sheen. The second-generation nail, at 9 to 12 months after the injury, is usually of much better quality.
Patients are told that the nail or artificial nail splint may fall out after 2 to 3 weeks as the new nail starts to grow. Complete nail regeneration takes about 4 to 6 months, and the first-generation nail lacks sheen. The second-generation nail, at 9 to 12 months after the injury, is usually of much better quality.
 The quality of the regenerated nail also depends on the initial injury to the sterile and germinal matrix and the age of the patient.
The quality of the regenerated nail also depends on the initial injury to the sterile and germinal matrix and the age of the patient.
 Figure 3-15 shows the late result of repair of a simple laceration of the sterile matrix after 3 months.
Figure 3-15 shows the late result of repair of a simple laceration of the sterile matrix after 3 months.
 Figure 3-16 shows the late result of repair of a stellate laceration involving the sterile and germinal matrices of the right index finger after 6 months.
Figure 3-16 shows the late result of repair of a stellate laceration involving the sterile and germinal matrices of the right index finger after 6 months.
 Figure 3-17 shows the late results of repair of the germinal matrix avulsion shown in Figure 3-12 after 6 months.
Figure 3-17 shows the late results of repair of the germinal matrix avulsion shown in Figure 3-12 after 6 months.
Roser SE, Gellman H. Comparison of nail bed repair versus nail trephination for subungual hematomas in children. J Hand Surg [Am]. 1999;24:1166-1170.
Strauss EJ, Weil WM, Jordan C, Paksima N. A prospective, randomized, controlled trial of 2-octylcyanoacrylate versus suture repair for nail bed injuries. J Hand Surg [Am]. 2008;33:250-253.