CHAPTER 3 GYNAECOLOGY
PREMENSTRUAL SYNDROME
Management
Prescribing
INTERMENSTRUAL (OR POSTCOITAL) BLEEDING
Management
IRREGULAR PERIODS
Irregular periods are almost always a non-pathological variant of normal. They are most common at the extremes of reproductive life. The patient can usually be reassured. Irregular periods are a feature of POS (see p. 49). This symptom may progress to amenorrhoea (see p. 43).
DYSMENORRHOEA
ENDOMETRIOSIS
Endometriosis is a common cause of dysmenorrhoea, dyspareunia, pelvic pain and menorrhagia. Diagnosis is by laparoscopy. Women with infertility and worsening symptoms should be referred. Hormonal treatment aims to suppress ovulation for 6–12 months, during which time the lesions atrophy. Endometriosis usually resolves at the menopause. Pelvic pain may be treated with:
MENORRHAGIA
Management
Prescribing
AMENORRHOEA
Management
PELVIC PAIN
Diagnosis
Try to exclude the following diagnoses on history and examination:
Management of acute pelvic inflammatory disease (PID)
An HVS and endocervical swab (both in bacterial transport media) and an endocervical chlamydia swab (see p. 46) should be taken.
Treatment with antibiotics is usually given without a definite diagnosis, and should cover Neisseria gonorrhoeae and Chlamydia (the two major causes), and mixed aerobic and anaerobic infections. Treat with ofloxacin 400 mg bd and metronidazole 400 mg bd for 14 days.
VAGINAL DISCHARGE
The most common causes of vaginal discharge in general practice are Candida and Gardnerella (bacterial vaginosis – BV). Trichomonas is a less common cause. Chlamydia, gonorrhoea and herpes simplex are rarely associated with vaginal discharge (see also STIs, p. 46).
SEXUALLY TRANSMITTED INFECTIONS
Investigations should be performed to exclude the presence of any other STI. Referral to a GUM clinic is recommended for full investigation and for treatment of the patient and their sexual contacts (see p. 2 for considering possible STI risk).
CHLAMYDIA
See also p. 15 for opportunistic screening.
Chlamydia is a major cause of PID, tubal infertility and ectopic pregnancy. It is the commonest curable STI in the industrialised world. Most women with chlamydia are asymptomatic. An endocervical chlamydia swab should be taken. Standard regimens for treatment of PID will cover chlamydia (see p. 44). Refer to a GUM clinic.
GONORRHOEA
Gonorrhoea is a major cause of PID. Patients should be referred to a GUM clinic. Remember chlamydia.
GENITAL WARTS
Genital warts are diagnosed by clinical appearance. They are caused by human papilloma virus (HPV).
URETHRAL SYNDROME
HIRSUTISM
Management
BREAST CANCER
THE MENOPAUSE/CLIMACTERIC
Diagnosis
Management
Hysterectomy with ovarian conservation is associated with early ovarian failure.
Bleeding usually becomes increasingly infrequent as the menopause approaches. However, any bleeding which occurs 1 year or more after the last period is considered to be postmenopausal (see p. 40) and should be referred for investigation to exclude malignancy.
HORMONE REPLACEMENT THERAPY (HRT)
Contraindications
First appointment
Advice
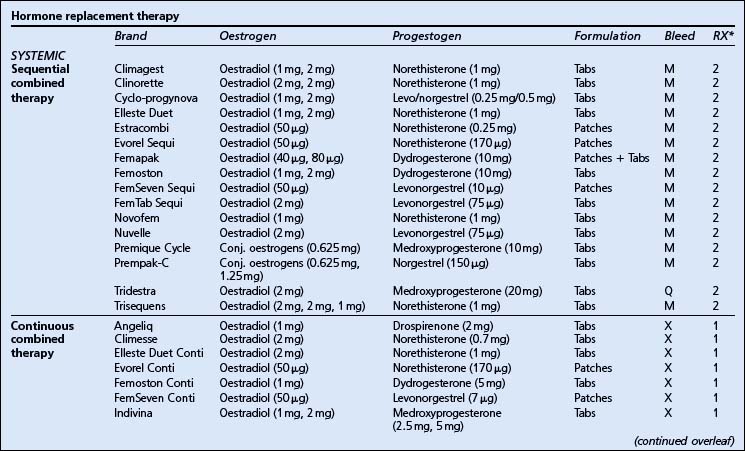
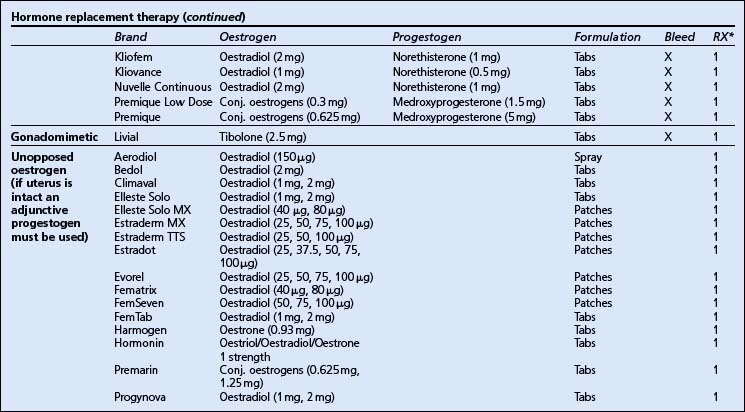
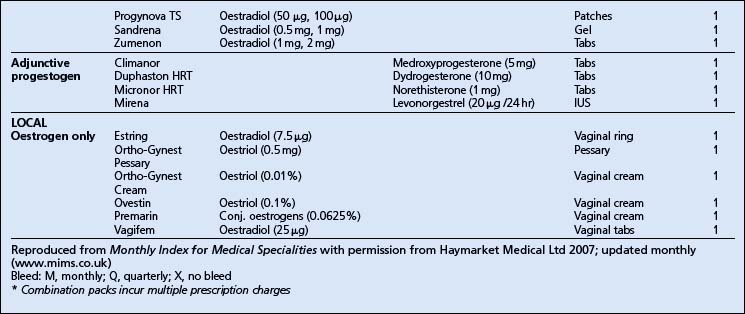
Prescribing.
(The lowest effective maintenance dose should be prescribed.)
CERVICAL CANCER
Cervical cancer kills 1000 women in the UK per year.
Discussion points for primary prevention of cervical cancer
Negative smear reports sometimes reveal incidental findings which require action as follows.
Specific infections
INFERTILITY
The main causes of infertility are:
Diagnosis
History
Investigations.
Before referral, the GP can arrange for semen analysis and confirmation of ovulation.
Confirmation of ovulation.
Ovulation can be confirmed by the following:
TERMINATION OF PREGNANCY REQUEST
The 1967 Abortion Act (revised in 1991) allows the following grounds for termination of pregnancy: