CASE 3 Extensive Coronary Calcification
Case presentation
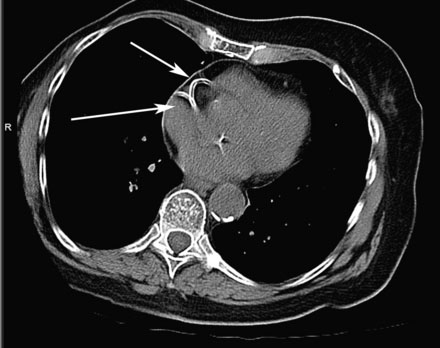
Three years following placement of a bare-metal stent in the right coronary artery, an otherwise active and healthy 85-year-old woman presented with the acute onset of sharp, stabbing anterior precordial chest pain radiating to the back. The pain was unrelieved by sublingual nitroglycerin and she presented to the hospital. Her only medications were aspirin 81 mg daily and atenolol 50 mg daily. Physical examination revealed a heart rate of 67 and a blood pressure of 110/54 mmHg and the remaining exam was unremarkable. In the emergency room, an electrocardiogram revealed nonspecific T wave inversion in lead III and initial cardiac biomarkers were not elevated. Because of the atypical nature of her chest pain and the absence of objective evidence of ischemia, she first underwent a CT angiogram of the chest to determine if her symptoms were due to an acute aortic dissection. This study showed no evidence of dissection but demonstrated extensive coronary and aortic calcification (Figure 3-1). She was admitted to a telemetry unit with a diagnosis of unstable angina, treated with enoxaparin, and underwent cardiac catheterization the next day.
Cardiac catheterization
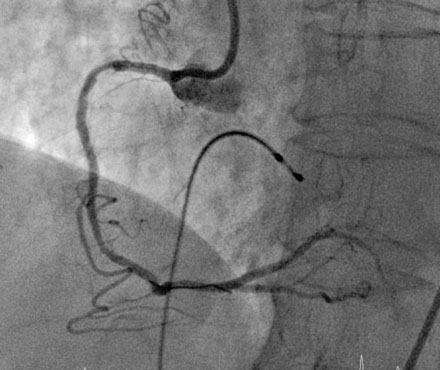
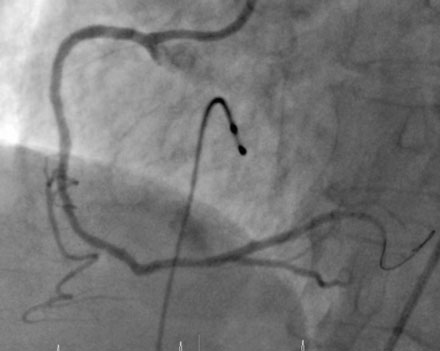
Fluoroscopy confirmed the extensive coronary calcification in both the right and left coronary trees seen by CT scan (Figure 3-2). Despite heavy calcification, there was no significant luminal obstruction present in the left coronary artery on angiography. The right coronary artery, however, contained a complex, high-grade stenosis in the proximal segment, with extensive calcification (Figure 3-3 and Video 3-1).
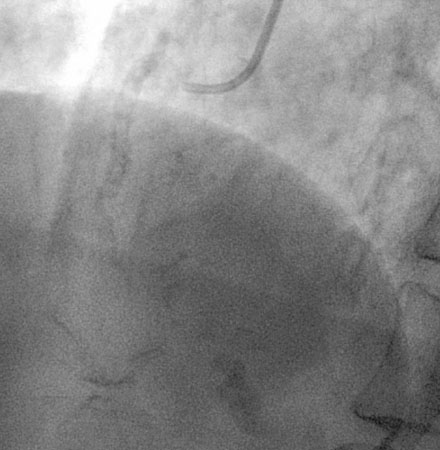
FIGURE 3-2 This is a fluoroscopic image of the right coronary artery showing the heavy calcification present.
Because of the extensive calcification, the operator planned to treat the artery by first performing rotational atherectomy followed by balloon angioplasty and stenting. After placing a temporary transvenous pacemaker, procedural anticoagulation was accomplished with a double bolus followed by an infusion of eptifibatide, along with a bolus of unfractionated heparin, to achieve an activated clotting time of greater than 200 seconds. A 6 French extra backup right coronary guide catheter was selectively engaged and a floppy RotaWire passed into the distal vessel. The operator used a 1.5 mm atherectomy burr, platformed to 160,000 rotations per minute. After three 30-second runs, the burr passed through the proximal lesion without deceleration and a satisfactory angiographic result was observed (Figure 3-4). The burr was removed from the guide catheter and a 2.5 mm diameter by 15 mm long compliant balloon fully expanded at only 6 atmospheres pressure. A 2.5 mm diameter by 15 mm long bare-metal stent was deployed at 15 atmospheres with an excellent angiographic result (Figure 3-5 and Video 3-2); intravascular ultrasound confirmed full stent deployment at the stent site.
Discussion
Procedural success in the presence of heavy coronary calcification may be facilitated by first debulking the lesion with rotational atherectomy (RA). Rotational atherectomy involves the use of a diamond-coated burr rotating at high speed to ablate the inelastic tissue of the plaque while preserving elastic tissue of the vessel wall. Ablation of even a small amount of calcified plaque often changes lesion compliance enough to render it more amenable to intervention. Pre-stenting atheroablation in calcified lesions results in a better acute angiographic result, a larger lumen, and a more favorable clinical outcome compared to either stenting alone or rotational atherectomy alone.1
The decision to first perform rotational atherectomy in a patient such as the one shown here is an important one. While many cases of extensive coronary calcification are successfully treated with balloon angioplasty and stenting, their response is highly unpredictable. A strategy of first attempting balloon angioplasty may be regretted when the operator struggles to dilate the lesion, creates an extensive dissection with a significant residual stenosis, and is then unable to pass a stent. Rotational atherectomy at this point is not possible because of the risk of extending the dissection. Pre-balloon RA might have prevented this scenario. Interestingly, success does not typically require aggressive atherectomy. Use of a single small-diameter burr such as the one used in this case (1.5 mm) is usually adequate to remove enough luminal calcium to facilitate balloon inflation and stent deployment. In fact, a strategy of aggressive rotational atherectomy (burr to artery ratio > 0.7) offers no advantage over modest atherectomy (burr to artery ratio < 0.7).2
1 Hoffmann R., Mintz G.S., Kent K.M., Pichard A.D., Satler L.F., Popma J.J., Hong M.K., Laird J.R., Leon M.B. Comparative early and nine-month results of rotational atherectomy, stents, and the combination of both for calcified lesions in large coronary arteries. Am J Cardiol. 1998;81:552-557.
2 Whitlow P.L., Bass T.A., Kipperman R.M., Sharaf B.L., Ho K.K.L., Cutlip D.E., Zhang Y., Kuntz R.E., Williams D.O., Lasorda D.M., Moses J.W., Cowley M.J., Ecclesotn D.S., Horrigan D.M., Bersin R.M., Ramee S.R., Feldman T. Results of the study to determine rotablator and transluminal angioplasty strategy (STRATAS). Am J Cardiol. 2001;87:699-705.