CHAPTER 3
Cervical Degenerative Disease
Definition
The term cervical degenerative disease encompasses a wide range of pathologic changes affecting all the components of the cervical spine that may lead to axial or radicular pain.
The mechanisms underlying cervical degenerative disease are complex and multifactorial. Genetics, aging, and attrition and trauma may all play an important role. It is believed that disc degeneration results in altered, abnormal load distribution, which in turn leads to a cascade of structural changes that affect the various components of the spinal column. These structural changes may change spinal posture and stability and may compromise neural function. The pathomechanisms underlying axial and radicular pain are still not completely clear. Increased vascularization after discal herniation and the presence of inflammatory mediators such as nitric oxide, prostaglandin E2, interleukin-6, matrix metalloproteinase, and others play an important role in the pathogenesis of pain [1].
In the seventh and eighth decades of life, most if not all individuals display diffuse degenerative changes throughout the cervical spine. Only a fraction of these individuals, however, have clinical signs and symptoms. Not uncommonly, individuals who are symptomatic early on become asymptomatic as the degenerative process evolves.
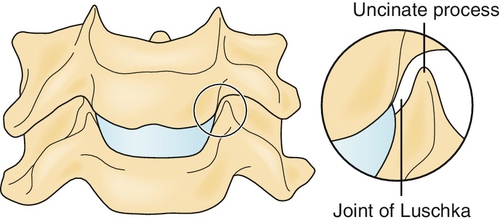
The lowest five cervical vertebrae are connected by five structural elements: the intervertebral disc, the facet joints, and the neurocentral joints (joints of Luschka) [2]. The neurocentral joints are unique to the cervical spine and do not appear anywhere else in the spinal column. These joints, located in the posterolateral aspect of the vertebral bodies, consist of bone projections that articulate with the vertebral body above them (Fig. 3.1). They provide some stability to the very mobile cervical spine and protect the exiting nerve roots from pure lateral disc herniations. Once the disc degenerates, however, these joints may hypertrophy, narrow the intervertebral foramina, and modify their shape, thus compromising the radicular nerves or the dorsal root ganglia. A similar degenerative process may involve the facet joints that are posteriorly located, and they in turn may compress the exiting neural elements from the back. Indeed, the most common cause of cervical radiculopathy is foraminal narrowing due to facet or neurocentral joint hypertrophy [3]. The lower cervical spine, especially C4-C5, C5-C6, and to a lesser extent C6-C7, is the source of pain in most symptomatic individuals. Unlike in the lumbar spine, nucleus pulposus herniation is less frequent and is the cause of radicular pain in only 20% to 25% of cases [3,4]. As the spinal cord occupies a substantial proportion of the cervical spinal canal, posteriorly directed herniations can result in significant cord compression as well as radicular symptoms.
Symptoms
The most common symptom, one that drives most of the patients to the physician’s office, is pain. In the general population, the point prevalence for neck pain ranges between 9.5% and 22%, whereas lifetime prevalence may be as high as 66%. The annual incidence is higher in men and peaks around 50 to 54 years of age [5,6].
In this respect, two large groups of patients can be recognized: patients whose main complaint is limited to axial pain and patients with radicular pain. Patients with axial pain typically complain of stiffness and pain in the cervical spine. The pain is usually more severe in the upright position and relieved only with bed rest. Cervical motion, especially hyperextension and side bending, increases the pain. In patients with pathologic changes involving the upper cervical joints or degeneration of upper cervical discs, the pain may radiate into the head, typically into the occipital region. In patients with lower cervical disease, the pain radiates into the region of the superior trapezius or the interscapular region. On occasion, patients present with atypical symptoms, such as jaw pain or chest pain–cervical angina.
Identification of the pain generator and its management are far more challenging in patients with axial pain because imaging studies frequently show multilevel pathologic changes, such as multilevel disc degeneration, facet arthropathy, and uncovertebral joint disease. It is often difficult and quite challenging to identify the exact source of pain. As the facets and the uncovertebral joints, peripheral discs, and ligaments all contain nerve endings, each one or a combination of them could be the source of pain [4].
Patients with radicular pain have symptoms commensurate with the involved nerve root. The pain usually follows a myotomal distribution and is frequently described as boring, aching, deep-seated pain. The pain is made worse by tilting the head toward the affected side or by hyperextension and side bending. Infrequently, patients find that the pain may be made more tolerable when the hand of the symptomatic side is placed over the top of the head (shoulder abduction release) [7]. The sensory symptoms (numbness, tingling, and burning sensation) usually follow the dermatomal distribution. When carpal tunnel syndrome accompanies cervical radiculopathy (double crush syndrome), the sensory changes may be in median nerve distribution. Indeed, there is a high concurrent incidence of cervical radiculopathy and carpal tunnel syndrome [8]. Sclerotomal pain, frequently overlooked or interpreted as trigger points, may be present and commonly resides in the medial or lateral scapular borders [9,10]. On occasion, patients complain of arm or hand weakness as they may drop things or find difficulty with routine activities of daily living.
Physical Examination
Because of severe axial pain, the patient may keep the head and neck immobile as cervical movements may increase the symptoms. Frequently, the only comfortable position is when the patient reclines and the neck is unloaded. Axial pain may increase with cervical extension or side bending. The Spurling test, whereby simultaneous axial loading and tilting of the head toward the symptomatic side in the upright position are performed, elicits neck and radicular pain. This test may elicit a specific dermatomal pain pattern and has high specificity and sensitivity of 95% for identifying nerve root compression [11]. Manual neck distraction may alleviate the symptoms. Tender spots are frequently found over the cervical paraspinal muscles, within the superior trapezius muscles, or in muscles supplied by the compromised root. These spots refer to areas within the muscles that, when stimulated, elicit a sensation of local pain [10]. Tender spots may be of diagnostic significance, especially when they are found unilaterally or in conjunction with other symptoms of cervical radiculopathy.
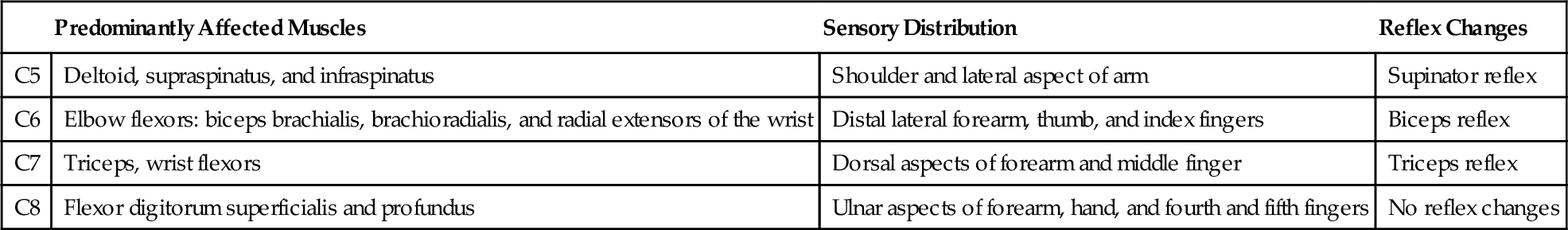
In patients with radicular pain, depending on the root involved, examination may reveal weakness in myotomal distribution, sensory changes in dermatomal distribution, and reflex changes (Table 3.1). Meticulous physical examination helps identify the compromised root: C5 root compromise will affect shoulder abductors; C6, elbow flexors; C7, elbow extensors; and C8, finger flexors. Finding of concomitant sensory and reflex changes is helpful. Dermatomal arrangement is not fixed and may vary in different patients because of aberrant rootlets or anastomoses between peripheral nerves. Frequently, dermatomes represent only a portion of the root’s domain [12]. The dermatomal charts are useful, however, and play a role in the patient’s diagnosis. Radicular pain frequently occurs without weakness, reflex, or apparent sensory changes. The most frequently affected roots are C5, C6, and C7 [3,6]. In the cervical region, unlike in other regions of the spine, the nerve roots exit the spine above their respective vertebrae; the C5 nerve root exits above C5 vertebra and hence may be compromised by herniation of the C4-5 intervertebral disc. The C8 nerve root exits below the C7 vertebral body; all the subsequent nerves below that level follow the same pattern.
Looking for long tract signs is of paramount importance because their presence points toward cord compression and may modify the treatment plan. The diagnostic accuracy of the physical examination is fairly reliable and may correlate well with imaging studies [9,11,13,14].
Functional Limitations
The functional limitations associated with cervical degenerative disease depend on the extent of the degenerative changes and the neurologic involvement. Not infrequently, patients are asymptomatic, and the only functional limitation noted is loss of cervical range of motion. They tend to hold the neck in a forward stooped posture; the neck is held in forward flexion and cannot achieve extension. When these patients stand against a wall, the back of the head may be inches away from it, and they cannot straighten the cervical spine. These patients may function well but have limited range of motion in all planes and cannot look up. When weakness is present, patients may have functional deficits corresponding with their spinal level of involvement (e.g., patients with C8-T1 involvement may drop things and have difficulties with movements requiring fine motor coordination).
Diagnostic Studies
Radiographs (anteroposterior, lateral, oblique, and flexion and extension views) are frequently obtained but may be of limited use. The vertebral components are clearly seen in these studies but not the intervertebral discs, spinal cord, or peripheral nerves. The x-ray films clearly show degenerative changes (narrowing intervertebral discs; spurs and calcified or ossified soft tissues). Frequently, there is no good correlation between the symptoms and the extent of degenerative findings on radiographs [14]. Diffuse multilevel changes are frequently observed but are, for the most part, irrelevant to the patient’s symptoms. Flexion and extension views are important as they can detect degenerative instability that is responsible for the symptoms and that may not be seen in the static views [6]. Radiographs are not helpful in the early stages of infection and tumors.
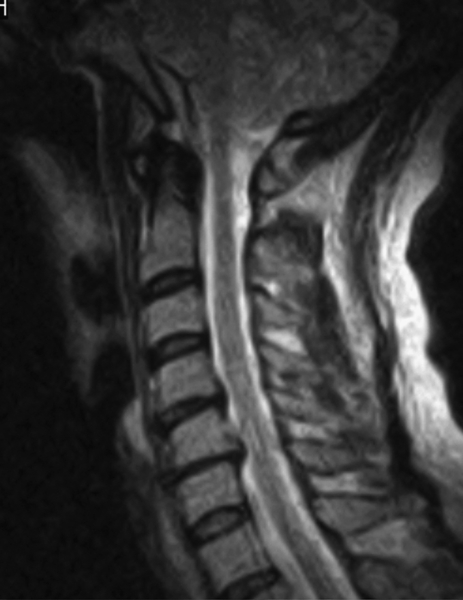
Magnetic resonance imaging is the diagnostic modality of choice because it allows visualization of the whole cervical spine without irradiation and enables the clinician to assess the neural structures (cord, roots) as well as the soft tissues (discs, ligaments). Correlation of the imaging studies with the history and clinical examination is of utmost importance because in many individuals, the magnetic resonance imaging studies reveal significant pathologic changes (herniated discs, neural foraminal stenosis) that are totally irrelevant to the patient’s complaints and symptoms (Fig. 3.2). Computed tomography should be obtained after trauma because it may identify fractures that could be otherwise missed on plain radiography and even magnetic resonance imaging studies. Computed tomographic myelography is frequently obtained before surgery but should not be obtained on a routine basis. Patients with axial pain who do not respond to conservative measures can be referred for discography to identify the pain generator. Discography may be the only way to identify the disc responsible for the symptoms; however, this procedure remains controversial and should be performed only in selected patients. Electrodiagnostic studies play an important role, especially in diabetic patients or whenever peripheral neuropathies are suspected [8,15].
Treatment
Initial
The management of patients with axial pain without radicular symptoms is much more challenging than the management of radicular pain. In the case of axial pain, it is often difficult to identify the pain generator and thus to initiate a direct therapeutic response. Anti-inflammatory drugs along with analgesics should be prescribed as a first line of treatment in the initial stages of the disease. Patients with severe radicular pain may be managed with systemic steroids, such as methylprednisolone (Dosepak), when they do not respond to other anti-inflammatory drugs. Steroids may be beneficial in relieving pain because they reduce inflammation and swelling, thereby facilitating neural nutrient and blood supply, and stabilize neural membranes, thus suppressing ectopic discharges within the affected nerve fibers. They may be administered during the course of a week to 10 days in tapering dose. For severe pain, a starting dose of 70 mg of prednisone decreasing by 10 mg daily may be recommended. Methylprednisolone is quite handy, as the daily dose is prearranged separately within the package. A substantial percentage of patients with spondylotic radicular nontraumatic pain are expected to improve significantly after fluoroscopically guided therapeutic selective nerve root injections (see later) [17,18]. Patients with severe burning pain may respond favorably to gabapentin (Neurontin) or pregabalin (Lyrica).
The patient should be instructed to try the shoulder abduction release maneuver as a therapeutic measure (i.e., put the affected hand over the head) with the hope that this might decrease the tension on the affected nerve root and bring some symptomatic relief [19].
Rehabilitation
Conclusive high-quality studies that clearly define the most efficient rehabilitation approach to patients with neck pain are still lacking [5]. The more commonly applied methods are summarized here.
Activity modifications are of paramount importance. It has been demonstrated in vivo that the neural foraminal dimensions vary with flexion and extension. It has been shown that cervical flexion increases foraminal height, width, and cross-sectional area, whereas extension has the opposite effects [20,21]. Because foraminal narrowing plays a major clinical role in patients with cervical radicular pain, patients should be advised to avoid activities in which cervical extension is involved. The patients should be instructed to drink with a straw, to avoid overhead activities, to face the sink while shampooing the hair, to adjust the monitor height, and the like. Temporary immobilization of the cervical spine may bring about some relief. This can be accomplished with a collar when the patient is mobile but should be used only temporarily. Cervical traction, provided it is administered in the supine position with the head held in slight flexion, may be of value in patients with radicular pain. Traction could be administered manually or, preferably, through a mechanized approach. The mechanized approach allows accurate traction forces to be administered. The distraction forces that are applied to the neck can, to some extent, relieve nerve compression by increasing the foraminal height and the intervertebral distance [22]. Traction application in the supine position is preferable because the weight of the head is eliminated and all the traction forces are effectively directed to the cervical spine. Despite its common use, no conclusive evidence that proves its therapeutic efficacy exists, however [23,24]. Superficial heat should be applied concomitantly with the traction as an adjunct therapy to relax the muscles before and during traction. Isometric neck exercises should be recommended as they may preserve muscle tone and strength without leading to pain. Cervical range of motion exercises are not recommended during the acute pain period.
Manual medicine (massage, mobilization, manipulation), acupuncture, and electrical stimulation are also widely used. Although these approaches are popular, studies demonstrating their efficacy are still lacking [25–32].
Procedures
Translaminar and transforaminal (selective nerve root) steroid administration may provide significant and at times long-term relief in patients with radicular pain. Properly selected, up to 60% of patients who are managed with selective nerve root injection may have good to excellent outcome [3,17]. Because there may be a significant risk with these injections (i.e., vertebral artery injury), they should be fluoroscopically guided and administered only by physicians with proper training.
Surgery
The main indications for surgery are severe or progressive neurologic deficits and persistent pain that does not respond to conservative measures.
The standard surgical treatment of cervical radiculopathy for many decades has been anterior cervical decompression and fusion. This approach prevailed because in most patients with cervical radiculopathy, the symptoms are caused by osteophytes compressing the nerves within the intervertebral foramina, and laminectomy is not effective in these cases.
The anterior approach permits excellent access to anteriorly impinging structures, such as discs and spondylotic spurs. Some surgeons add instrumentation (i.e., plate) to increase the fusion rate and the postoperative stability [13]. Adequate foraminal decompression can result in early pain relief and enhanced muscle strength. Long term, however, no significant differences in pain or function have been found between conservatively and surgically treated patients [25,33]. Dysphagia, which frequently follows the anterior approach, usually subsides several weeks postoperatively.
The negative long-term effects of fusion have only recently been appreciated. Fusion leads to stiffness and lost range of motion, and over the years, it results in next-level degeneration (i.e., accelerated discal degeneration above and below the fused vertebrae). This has led to the development of disc replacement surgery—arthroplasty. Whereas the concept of disc replacement is attractive as disc replacement maintains the intervertebral discal height while preserving spinal motion [34], the advantages of this approach and its long-term effects have not yet been established [35].
Patients with single-level soft disc herniation may be operated on from the back. In these patients, laminotomy with foraminotomy may bring about relief without fusion and its complications while maintaining cervical stability [13].
Potential Disease Complications
Chronic pain and permanent neurologic deficits may develop in some patients. These may compromise the quality of life and interfere with activities of daily living.
Potential Treatment Complications
Steroid administration carries certain risks, and these should be considered before steroid administration. Surgical complications include infection, nerve injury, pain, stiffness, pseudarthrosis, and next-level degeneration.