Section III ACLS Guidelines for Adult Emergency Cardiac Care Algorithms
Pulseless Ventricular Tachycardia (VT)/Ventricular Fibrillation (VF)
Do not interrupt CPR for more than 5–10 seconds for any reason
Pattern becomes CPR-shock-drug
Circulation
Epinephrine (Class Indeterminate)—1 mg (1:10,000 solution) IV every 3–5 minutes.
Vasopressin (Class IIb)—40 units IV bolus (administer only once). (If no response to vasopressin, may resume epinephrine after 10–20 minutes; epinephrine dose 1 mg every 3–5 minutes.)
• Give one shock and immediately resume chest compressions after the shock.
• Re-evaluate cardiac rhythm after 2 minutes (5 cycles) of CPR.
• Amiodarone (Class IIb)—Initial bolus: 300 mg IV/IO bolus diluted in 20–30 mL of NS or D5W. Consider repeat dose (150 mg IV bolus) in 3–5 minutes. If defibrillation successful, follow with 1 mg/min IV infusion for 6 hours (mix 900 mg in 500 mL NS), then decrease infusion rate to 0.5 mg/min IV infusion for 18 hours. Maximum daily dose 2.2 g IV/24 hr.
• Lidocaine (Class Indeterminate)—1.0–1.5 mg/kg IV/IO bolus, consider repeat dose (0.5–0.75 mg/kg) in 5 minutes; maximum IV bolus dose 3 mg/kg. (The 1.5 mg/kg dose is recommended in cardiac arrest.)
• Magnesium (Class IIb if hypomagnesemia present)—1–2 g IV/IO (2–4 mL of a 50% solution) diluted in 10 mL of D5W if torsades de pointes or hypomagnesemia.
Modified from Aehlert B: ACLS quick review study guide, ed 3, St. Louis, 2007, Mosby. Additional information modified from American Heart Association (AHA): Advanced cardiac life support provider manual, 2006, American Heart Association.
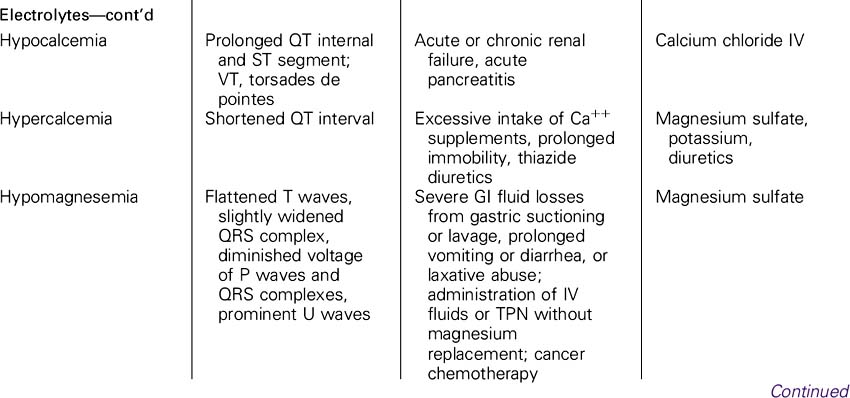
Possible causes of asystole: PATCH-4-MD Pulmonary embolism Acidosis Tension pneumothorax Cardiac tamponade Hypovolemia (most common cause) Hypoxia Heat/cold (hypothermia/ hyperthermia) Hypokalemia/ hyperkalemia (and other electrolytes) Myocardial infarction Drug overdose/accidents (cyclic antidepressants, calcium channel blockers, beta-blockers, digitalis)
Modified from Aehlert B: ACLS quick review study guide, ed 3, St Louis, 2007, Mosby. Additional information modified from American Heart Association (AHA): Advanced cardiac life support provider manual, 2006, American Heart Association.
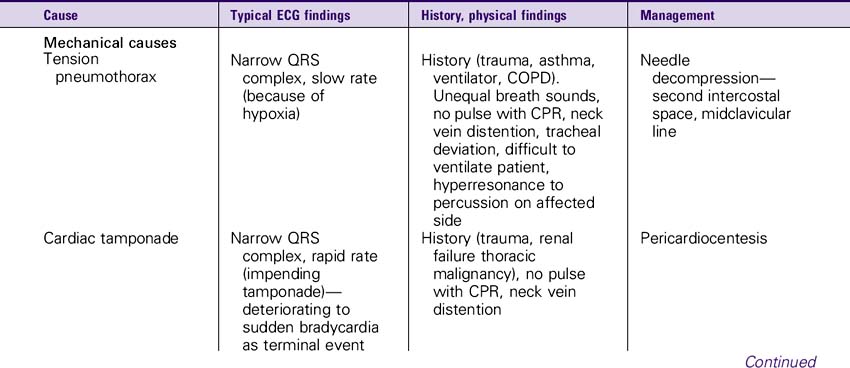
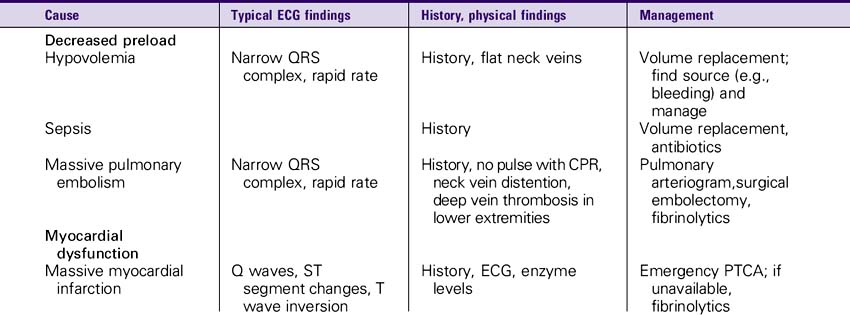
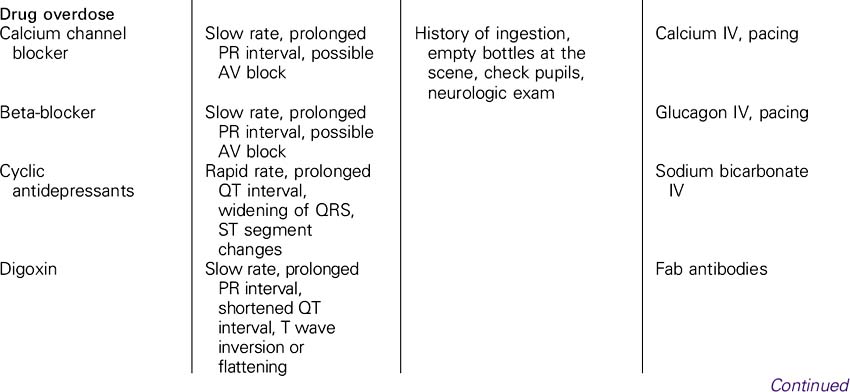
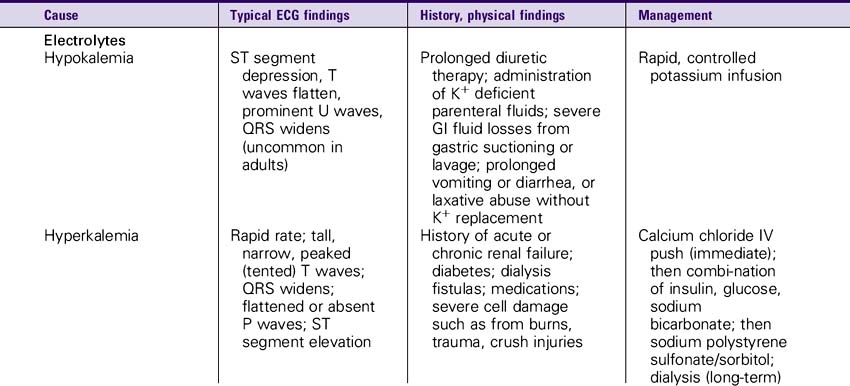
Pulseless Electrical Activity (PEA)
Possible causes of PEA: PATCH-4-MD Pulmonary embolism Acidosis Tension pneumothorax Cardiac tamponade Hypovolemia (most common cause) Hypoxia Heat/cold (hypothermia/ hyperthermia) Hypokalemia/hyperkalemia (and other electrolytes) Myocardial infarction Drug overdose/accidents (cyclic antidepressants, calcium channel blockers, beta-blockers, digitalis)
Differential Diagnosis
• Search for and treat reversible causes (PATCH-4-MD). (Fast narrow QRS—consider hypovolemia, tamponade, pulmonary embolism, tension pneumothorax; slow wide QRS—consider cyclic antidepressant overdose, calcium channel blocker, beta-blocker, or digitalis toxicity.)
Epinephrine—1 mg (1:10,000 solution) IV/IO every 3–5 minutes.
Modified from Aehlert B: ACLS quick review study guide, ed 3, St Louis, 2007, Mosby.Additional information modified from American Heart Association (AHA): Advanced cardiac life support provider manual, 2006, American Heart Association.
Modified from Aehlert B: ACLS quick review study guide, ed 3, St Louis, 2007, Mosby. Additional information modified from American Heart Association (AHA): Advanced cardiac life support provider manual, 2006, American Heart Association.
Advanced life support
Identify the Patient’s Cardiac Rhythm
Is the patient experiencing serious signs and symptoms because of the bradycardia?
• Signs: Low BP, shock, pulmonary congestion, congestive heart failure, angina, acute myocardial infarction (MI), ventricular ectopy
• Symptoms: Chest pain, weakness, fatigue, dizziness, lightheadedness, shortness of breath, exercise intolerance, decreased level of responsiveness
• If no serious signs and symptoms are present, observe.
• If serious signs and symptoms are present, further intervention depends on the cardiac rhythm identified.

Modified from Aehlert B: ACLS quick review study guide, ed 2, St Louis, 2001, Mosby, pp 435–436. Additional information modified from American Heart Association (AHA): Advanced cardiac life support provider manual, 2006, American Heart Association.
Advanced life support
Perform Secondary BLS Survey
• Obtain and review 12-lead ECG.
• Perform a focused history and physical exam.
• Is the patient stable or unstable?
• Is the patient experiencing serious signs and symptoms because of the tachycardia?
Attempt to identify patient’s cardiac rhythm using:
• May repeat 12-mg dose in 1–2 minutes if needed.
• Follow each dose immediately with 20-mL IV flush of NS.
• Use of adenosine is relatively contraindicated in patients with asthma.
• Decrease dose in patients on dipyridamole (Persantine) or carbamazepine (Tegretol); consider increasing dose in patients taking theophylline or caffeine-containing preparations.
Medication Dosing
Amiodarone—150 mg IV/IO over 10 minutes followed by an infusion of 1 mg/min for 6 hours and then a maintenance infusion of 0.5 mg/min. Repeat supplementary infusions of 150 mg as necessary for recurrent or resistant dysrhythmias. Maximum total daily dose 2 g.
Beta-blockers—Esmolol: 0.5 mg/kg over 1 minute, followed by a maintenance infusion at 50 mcg/kg/min for 4 minutes. If inadequate response, administer a second bolus of 0.5 mg/kg over 1 minute and increase maintenance infusion to 100 mcg/kg/min. The bolus dose (0.5 mg/kg) and titration of the maintenance infusion (addition of 50 mcg/kg/min) can be repeated every 4 minutes to a maximum infusion of 300 mcg/kg/min. Metoprolol: 5 mg slow IV push over 5 minutes × 3 as needed to a total dose of 15 mg over 15 minutes.
Calcium channel blockers—Diltiazem: 0.25 mg/kg over 2 minutes (e.g., 15–20 mg). If ineffective, 0.35 mg/kg over 2 minutes (e.g., 20–25 mg) in 15 minutes. Maintenance infusion 5–15 mg/hr, titrated to HR if chemical conversion successful. Calcium chloride (2–4 mg/kg) may be given slow IV push if borderline hypotension exists before administration. Verapamil: 2.5–5.0 mg slow IV push over 2 minutes. May repeat with 5–10 mg in 15–30 minutes. Maximum dose 20 mg.
| Type of countershock | Dysrhythmia | Recommended energy levels |
|---|---|---|
| Defibrillation | Pulseless VF/VT | 360 J or equivalent biphasic energy |
| Sustained polymorphic VT | 360 J or equivalent biphasic energy | |
| VT with a pulse | 100 J, 200 J, 300 J, 360 J or equivalent biphasic energy | |
| Synchronized cardioversion | Paroxysmal supraventricular tachycardia (PSVT) | 50 J, 100 J, 200 J, 300 J, 360 J or equivalent biphasic energy |
| Atrial flutter | 50 J, 100 J, 200 J, 300 J, 360 J or equivalent biphasic energy | |
| Atrial fibrillation | 100 J, 200 J, 300 J, 360 J or equivalent biphasic energy | |
| VT with a pulse | 100 J, 200 J, 300 J, 360 J or equivalent biphasic energy |
Modified from Aehlert B: ACLS quick review study guide, ed 3, St Louis, 2007, Mosby. Additional information modified from American Heart Association (AHA): Advanced cardiac life support provider manual, 2006, American Heart Association.
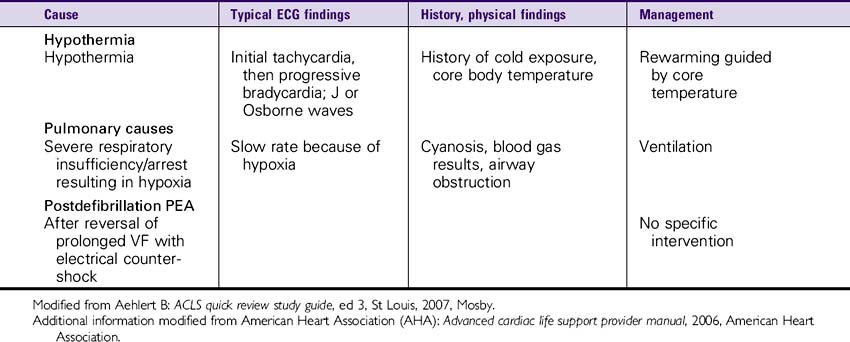
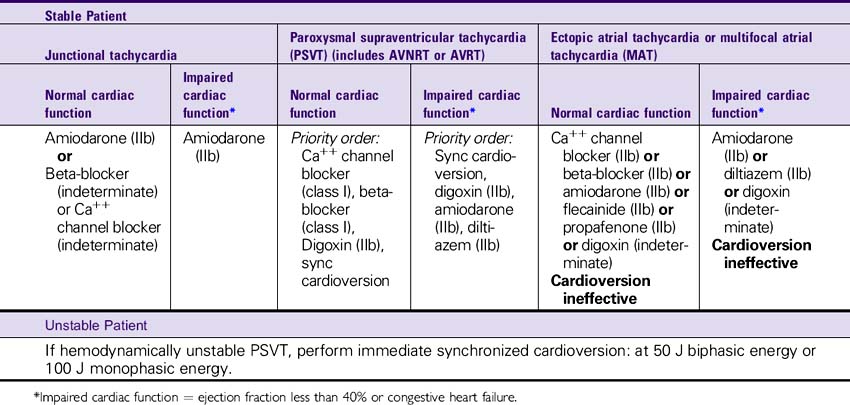
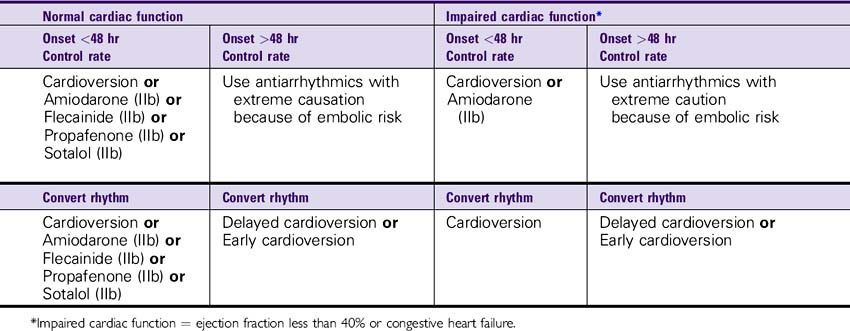
Atrial Fibrillation/Atrial Flutter Algorithm
Modified from Aehlert B: ACLS quick review study guide, ed 3, St Louis, 2007, Mosby. Additional information modified from American Heart Association (AHA): Advanced cardiac life support provider manual, 2006, American Heart Association.
Advanced life support
Perform Secondary BLS Survey
• Administer oxygen, establish IV/IO access, attach cardiac monitor, administer fluids as needed (O2, IV, monitor, fluids).
• Assess vital signs, attach pulse oximeter, and monitor BP.
• Obtain and review 12-lead ECG.
• Perform a focused history and physical exam.
Is the patient stable or unstable?
• Is the patient’s cardiac function normal or impaired?
• Is the patient experiencing serious signs and symptoms because of the tachycardia?
• Attempt to identify patient’s cardiac rhythm using 12-lead ECG, clinical information.
• Is Wolff-Parkinson-White syndrome (WPW) present? If yes, see WPW algorithm.
• Has atrial fibrillation/atrial flutter been present for greater than or less than 48 hours?
Identify the Patient’s Cardiac Rhythm
Delayed cardioversion: Anticoagulation therapy for 3 weeks before cardioversion, for at least 48 hours in conjunction with cardioversion, and for at least 4 weeks after successful cardioversion.
Early cardioversion: IV heparin immediately, transesophageal echocardiography (TEE) to rule out atrial thrombus, cardioversion within 24 hours, anticoagulation × 4 weeks.
| Unstable Patient |
|---|
| If hemodynamically unstable, perform synchronized cardioversion: |

Medication Dosing
Amiodarone—150 mg IV bolus over 10 minutes followed by an infusion of 1 mg/min for 6 hours and then a maintenance infusion of 0.5 mg/min. Repeat supplementary infusions of 150 mg as necessary for recurrent or resistant dysrhythmias. Maximum total daily dose 2 g.
Beta-blockers—Esmolol: 0.5 mg/kg over 1 minute followed by a maintenance infusion at 50 mcg/kg/min for 4 minutes. If inadequate response, administer a second bolus of 0.5 mg/kg over 1 minute and increase maintenance infusion to 100 mcg/kg/min. The bolus dose (0.5 mg/kg) and titration of the maintenance infusion (addition of 50 mcg/kg/min) can be repeated every 4 minutes to a maximum infusion of 300 mcg/kg/min.
Metoprolol: 5 mg slow IV push over 5 minutes × 3 as needed to a total dose of 15 mg over 15 minutes.
Propranolol: 0.1 mg/kg slow IV push divided in 3 equal doses at 2–3 minute intervals. Do not exceed 1 mg/min. Repeat after 2 minutes, if necessary.
Atenolol: 5 mg slow IV (over 5 min). Wait 10 minutes, then give second dose of 5 mg slow IV (over 5 min).
Calcium channel blockers—Diltiazem: 0.25 mg/kg over 2 minutes (e.g., 15–20 mg). If ineffective, 0.35 mg/kg over 2 minutes (e.g., 20–25 mg) in 15 minutes. Maintenance infusions 5–15 mg/hr, titrated to HR if chemical conversion successful. Calcium chloride (2–4 mg/kg) may be given slow IV push if borderline hypotension exists before diltiazem administration. Verapamil: 2.5–5.0 mg slow IV push over 2 minutes. May repeat with 5–10 mg in 15–30 minutes. Maximum dose 20 mg.
Ibutilide—Adults weighing 60 kg or more: 1 mg (10 mL) over 10 minutes. May repeat × 1 in 10 minutes. Adults weighing less than 60 kg: 0.01 mg/kg IV over 10 minutes.
Procainamide—100 mg over 5 minutes (20 mg/min). Maximum total dose 17 mg/kg. Maintenance infusion 1–4 mg/min. Flecainide propafenone: IV form not currently approved for use in the United States.
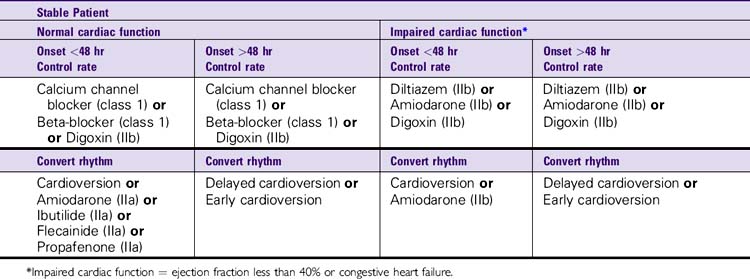
Wolff-Parkinson-White (WPW) Syndrome Algorithm
Modified from Aehlert B: ACLS quick review study guide, ed 3, St Louis, 2007, Mosby. Additional information modified from American Heart Association (AHA): Advanced cardiac life support provider manual, 2006, American Heart Association.
Basic life support
Circulation
• Perform high-quality chest compressions until monitor/AED becomes available.
• Assess vital signs, attach pulse oximeter, and monitor BP.
• Is the patient stable or unstable?
• Is the patient’s cardiac function normal or impaired?
• Is the patient experiencing serious signs and symptoms because of the tachycardia?
• Attempt to identify patient’s cardiac rhythm using 12-lead ECG, clinical information.
• Is Wolff-Parkinson-White syndrome (WPW) present (e.g., young patient; HR greater than 300 beats/min; ECG: short PR interval, wide QRS, delta wave)?
• Has WPW been present for greater than or less than 48 hours?
Identify the Patient’s Cardiac Rhythm
Delayed cardioversion: Anticoagulation therapy for 3 weeks before cardioversion for at least 48 hours in conjunction with cardioversion and for at least 4 weeks after successful cardioversion.
Early cardioversion: IV heparin immediately, transesophageal echocardiography (TEE) to rule out atrial thrombus, cardioversion within 24 hours anticoagulation × 4 weeks.
Medication Dosing
Amiodarone—150 mg IV bolus over 10 minutes followed by an infusion of 1 mg/min for 6 hours and then a maintenance infusion of 0.5 mg/min. Repeat supplementary infusion of 150 mg as necessary for recurrent or resistant dysrhythmias. Maximum total daily dose 2 g.
Procainamide—100 mg over 5 minutes (20 mg/min). Maximum total dose 17 mg/kg. Maintenance infusion 1–4 mg/min.
Flecainide, propafenone—IV form not currently approved for use in the United States.
Sustained Monomorphic Ventricular Tachycardia
Modified from Aehlert B: ACLS quick review study guide, ed 3, St Louis, 2007, Mosby. Additional information modified from American Heart Association (AHA): Advanced cardiac life support provider manual, 2006, American Heart Association.
Advanced life support
Perform Secondary BLS Survey
• Assess vital signs, attach pulse oximeter, and monitor BP.
• Obtain and review 12-lead ECG, portable chest x-ray film.
• Perform a focused history and physical exam.
• Is the patient stable or unstable?
• Is the patient experiencing serious signs and symptoms because of the tachycardia?
• Determine whether the rhythm is monomorphic or polymorphic VT and determine patient’s QT interval.
Identify the Patient’s Cardiac Rhythm
| Stable Patient | |
|---|---|
| May proceed directly to synchronized cardioversion, or use one of the following. | |
| Normal cardiac function | Impaired cardiac function* |
| Unstable VT with a pulse | |
|---|---|
* Impaired cardiac function = ejection fraction less than 40% or congestive heart failure.
Medication Dosing
Amiodarone—150 mg IV bolus over 10 minutes. If chemical conversion successful, follow with IV infusion of 1 mg/min for 6 hours and then a maintenance infusion of 0.5 mg/min. Repeat supplementary infusions of 150 mg as necessary for recurrent or resistant dysrhythmias. Maximum total daily dose 2 g.
Lidocaine—1–1.5 mg/kg initial dose. Repeat dose is half the initial dose every 5–10 minutes. Maximum total dose 3 mg/kg. If chemical conversion successful, maintenance infusion 1–4 mg/min. If impaired cardiac function, dose = 0.5–0.75 mg/kg IV push. May repeat every 5–10 minutes. Maximum total dose 3 mg/kg. If chemical conversion successful, maintenance infusion 1–4 mg/min.
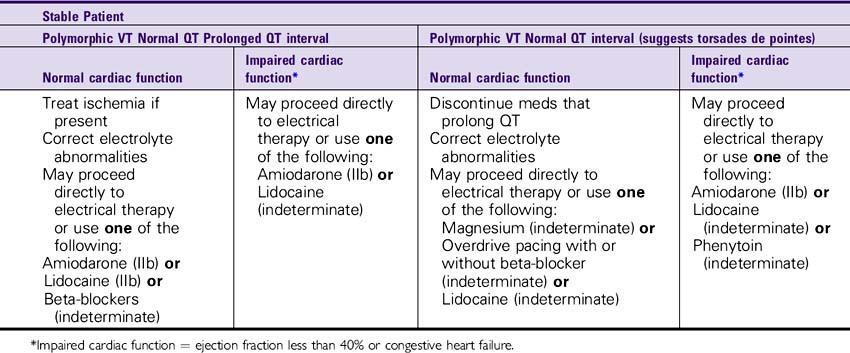
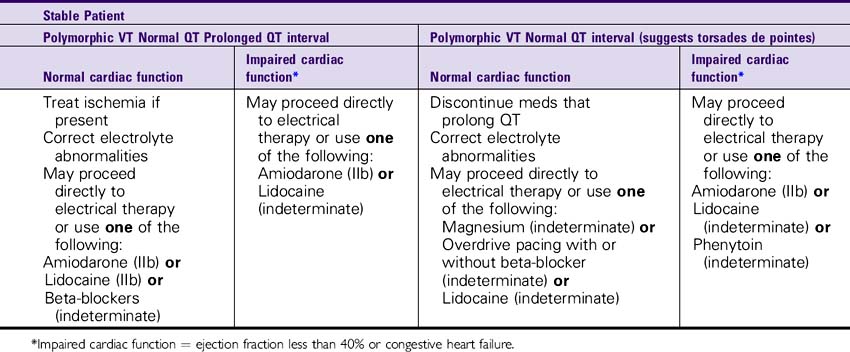
Polymorphic Ventricular Tachycardia
Modified from Aehlert B: ACLS quick review study guide, ed 3, St Louis, 2007, Mosby. Additional information modified from American Heart Association (AHA): Advanced cardiac life support provider manual, 2006, American Heart Association.
Advanced life support
Assess and support airway, breathing and circulation as needed
• Administer oxygen, establish IV/IO access, attach cardiac monitor, administer fluids as needed (O2, IV, monitor, fluids).
• Assess vital signs, attach pulse oximeter, and monitor BP.
• Obtain and review 12-lead ECG.
• Perform a focused history and physical exam.
• Is the patient stable or unstable?
• Is the patient experiencing serious signs and symptoms because of the tachycardia?
• Determine whether the rhythm is monomorphic or polymorphic VT and determine patient’s QT interval.
Identify the Patient’s Cardiac Rhythm
| Unstable Patient |
|---|

Medication Dosing
Amiodarone—150 mg IV bolus over 10 minutes. If chemical conversion successful, follow with IV infusion of 1 mg/min for 6 hours and then a maintenance infusion of 0.5 mg/min. Repeat supplementary infusions of 150 mg as necessary for recurrent or resistant dysrhythmias. Maximum total daily dose 2 g.
Beta-blockers—Esmolol: 0.5 mg/kg over 1 minute followed by a maintenance infusion at 50 mcg/kg/min for 4 minutes. If inadequate response, administer a second bolus of 0.5 mg/kg over 1 minute and increase maintenance infusion to 100 mcg/kg/min. The bolus dose (0.5 mg/kg) and titration of the maintenance infusion (addition of 50 mcg/kg/min) can be repeated every 4 minutes to a maximum infusion of 300 mcg/kg/min. Metoprolol: 5 mg slow IV push over 5 minutes × 3 as needed to a total dose of 15 mg over 15 minutes. Atenolol: 5 mg slow IV (over 5 min). Wait 10 minutes, then give second dose of 5 mg slow IV (over 5 min).
Lidocaine—1–1.5 mg/kg initial dose. Repeat half the initial dose every 5–10 minutes. Maximum total dose 3 mg/kg. If chemical conversion successful, maintenance infusion 1–4 mg/min. If impaired cardiac function, dose = 0.5–0.75 mg/kg IV push. May repeat every 5–10 minutes. Maximum total dose 3 mg/kg. If chemical conversion successful, maintenance infusion 1–4 mg/min.
Magnesium—Loading dose of 1–2 g mixed in 50–100 mL over 5–10 minutes IV. If chemical conversion successful, follow with 0.5–1 g/hr IV infusion.
Phenytoin—250 mg IV at a rate of 25–50 mg/min in NS using a central vein.
Wide QRS Tachycardia of Unknown Origin
Modified from Aehlert B: ACLS quick review study guide, ed 3, St Louis, 2007, Mosby. Additional information modified from American Heart Association (AHA): Advanced cardiac life support provider manual, 2006, American Heart Association.
Advanced life support
Assess and support airway, breathing and circulation as needed
• Administer oxygen, establish IV/IO access, attach cardiac monitor, administer fluids as needed (O2, IV, monitor, fluids).
• Assess vital signs, attach pulse oximeter, and monitor BP.
• Obtain and review 12-lead ECG, portable chest x-ray film.
• Perform a focused history and physical exam.
• Is the patient stable or unstable?
• Is the patient experiencing serious signs and symptoms because of the tachycardia?
• Use 12-lead ECG/clinical information to help clarify rhythm diagnosis.
Initial Assessment and General Treatment of the Patient with an Acute Coronary Syndrome (ACS)
Prehospital
• Obtain a brief, targeted history/physical exam (determine age, gender; signs/symptoms, pain presentation, including location of pain, duration, quality, relation to effort, time of symptom onset; history of coronary artery disease [CAD]; CAD risk factors present?; and history of Viagra use).
If above consistent with possible or definite ACS:
• Use checklist (yes-no); focus on eligibility for reperfusion therapy; evaluate contraindications to aspirin and heparin.
• Establish IV access, ECG monitoring.
• Administer aspirin 162–325 mg (chewed), unless appropriate exclusion criteria exist.
• Obtain 12-lead ECG (machine interpretation or transmission of ECG to physician).
• Draw blood for initial serum cardiac marker levels (to lab on arrival in Emergency Department).
Consider triage to facility capable of angiography and revascularization if any of the following are present:
Emergency Department
• Obtain a brief, targeted history/physical exam (determine age, gender; signs/symptoms, pain presentation, including location of pain, duration, quality, relation to effort, time of symptom onset; history of CAD, CAD risk factors present) and history of Viagra use.
• Assess vital signs, determine oxygen saturation.
If above consistent with possible or definite ACS:
• Brief, targeted history/physical exam
• Evaluate eligibility for reperfusion therapy and contraindications to aspirin and heparin.
• Administer aspirin 162–325 mg (chewed), unless appropriate exclusion criteria exist.
• Administer nitroglycerin as indicated.
• Evaluate 12-lead ECG—Categorize patient into one of three groups: ST-elevation or new or presumably new left bundle branch block (LBBB); ST-depression/transient ST-segment/T wave changes; normal or nondiagnostic ECG.
• Obtain serial ECGs in patients with history suggesting myocardial infarction (MI) and nondiagnostic ECG.
• Obtain baseline serum cardiac marker levels (CK-MB, troponin T or I, myoglobin).
• Obtain lab specimens (CBC, lipid profile, electrolytes, coagulation studies).
• Oxygen 4 L/min by nasal cannula for first 2–3 hours (class IIa).
• Oxygen 4 L/min by cannula, titrate if pulmonary congestion, SaO2 less than 90% (class I).
• Aspirin 162–325 mg (chewed) (if hypersensitivity exists, ticlopidine); may administer via rectal suppository (325 mg) if nausea, vomiting, upper GI disorder present.
• Nitroglycerin sublingual or spray; may repeat twice at 5-minute intervals (ensure IV access, SBP greater than 90 mm Hg, HR greater than 50 beats/min. Use with caution in the case of right ventricular infarction).
• Morphine 2–4 mg IV if pain not relieved with nitroglycerin; may repeat every 5 minutes (ensure SBP greater than 90 mm Hg).
Modified from Aehlert B: ACLS quick review study guide, ed 3, St Louis, 2007, Mosby. Additional information modified from American Heart Association (AHA): Advanced cardiac life support provider manual, 2006. American Heart Association.
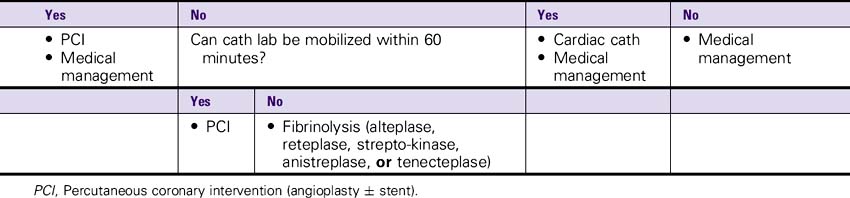
Management of ST-Segment Elevation Myocardial Infarction (MI)
ST-segment elevation 1 mm or more in two or more anatomically contiguous leads or new, or presumably new, left bundle branch block (LBBB)
• Antiplatelet therapy—Aspirin 162–325 mg (chewed)
• Antiischemia therapy—Beta-blockers, nitroglycerin IV (if ongoing ischemia or uncorrected hypertension)
• Antithrombin therapy—Heparin (if using fibrin-specific lytics)
• ACE inhibitors (after 6 hours or when stable)—Especially with large or anterior MI, heart failure without hypotension (SBP greater than 100 mm Hg), previous MI
| Symptom onset >12 hours | |
|---|---|
| Persistent symptoms |
Modified from Aehlert B: ACLS quick review study guide, ed 3, St Louis, 2007, Mosby. Additional information modified from American Heart Association (AHA): Advanced cardiac life support provider manual, 2006, American Heart Association.
Management of Unstable Angina/Non–ST-Segment Elevation Myocardial Infarction (MI)
ECG changes in two or more anatomically contiguous leads
• ST-segment depression greater than 1 mm or T wave inversion greater than 1 mm or
• Transient (less than 30 minutes) ST-segment/T wave changes greater than 1 mm with discomfort
Confirm diagnosis by signs/symptoms, ECG, serum cardiac markers.
All patients with unstable angina/non–ST-segment elevation MI should receive the following (if no contraindications)
• Aspirin—162–325 mg (chewed) if not already administered (and no contraindications) (antiplatelet therapy).
High-risk criteria
• Persistent (“stuttering”) symptoms/recurrent ischemia; left ventricular (LV) dysfunction, congestive heart failure (CHF); widespread ECG changes; prior MI, positive troponin or CK-MB.
Antiischemic therapy (e.g., metoprolol, atenolol, esmolol, propranolol) includes:
• Beta-blockers—If patient not previously on beta-blockers or inadequately treated on current dose of beta-blocker (if no contraindications).
• Nitroglycerin sublingual tablet or spray, followed by IV nitroglycerin—if symptoms persist despite sublingual nitroglycerin therapy and initiation of beta-blocker therapy (and SBP greater than 90 mm Hg).
• Morphine—2–4 mg IV (if discomfort is not relieved or symptoms recur despite antiischemic therapy); may repeat every 5 minutes (ensure SBP greater than 90 Hg).
| Assess clinical status: Is patient clinically stable? | |
|---|---|
| Yes | No |
| Continue in-hospital observation | Cardiac cath |
PCI, Percutaneous coronary intervention; CABG, coronary artery bypass grafting.
Modified from Aehlert B: ACLS quick review study guide, ed 3, St Louis, 2007, Mosby. Additional information modified from American Heart Association (AHA): Advanced cardiac life support provider manual, 2006, American Heart Association.
Management of Patient with a Suspected Acute Coronary Syndrome and Nondiagnostic or Normal ECG
• Evaluate signs/symptoms, serial ECGs, serum cardiac markers.
• Administer aspirin + other therapy as appropriate.
• Assess patient’s clinical risk or death/nonfatal MI.
• Perform a focused history and physical exam.
• Obtain follow-up serum cardiac marker levels, serial ECG monitoring.
• Consider evaluation and treatment in Emergency Department, chest pain unit, or monitored bed.
Modified from Aehlert B: ACLS quick review study guide, ed 3, St Louis, 2007, Mosby. Additional information modified from American Heart Association (AHA): Advanced cardiac life support provider manual, 2006, American Heart Association.
Management of Acute Pulmonary Edema
Advanced life support
Support airway, breathing and circulation as needed
• Administer oxygen, establish IV access, attach cardiac monitor, administer fluids as needed (O2, IV/IO, monitor).
• Assess vital signs, attach pulse oximeter, and monitor BP.
• Obtain and review 12-lead ECG, portable chest x-ray film.
If feasible and BP permits, place patient in sitting position with feet dependent:
If systolic BP greater than 100 mm Hg:
• Sublingual nitroglycerin—1 tablet or spray every 5 minutes (max 3 tablets) until IV nitroglycerin or nitroprusside can take effect.
• Furosemide IV—0.5–1.0 mg/kg (typically 20–40 mg) (can repeat in 30 min if symptoms persist and BP stable).
• Consider morphine IV—2–4 mg.
Consider additional preload/afterload reduction—nitroglycerin or nitroprusside IV, angiotensin converting enzyme (ACE) inhibitors (if SBP greater than 100 mm Hg):
• Nitroglycerin IV—Start at 5 mcg/min and increase gradually until mean systolic pressure falls by 10%-15%, avoid hypotension (SBP less than 90 mm Hg) or
• Readily reversible cause: Institute appropriate intervention (e.g., cardiac dysrhythmias, tamponade).
• Myocardial ischemia/infarction: Institute appropriate intervention—candidate for fibrinolytic therapy? PTCA?
If patient is refractory to previous therapies, hypotensive, or in cardiogenic shock:
• Consider fluid or IV inotropic and/or vasopressor agents (e.g., dobutamine, dopamine, norepinephrine).
• Consider pulmonary and systemic arterial catheterization.
• Obtain ECG to assist in diagnosis, evaluation, and reparability of culprit lesion or condition.
• Consider need for mechanical circulatory assistance (balloon pump).
Modified from Aehlert B: ACLS quick review study guide, ed 3, St Louis, 2007, Mosby. Additional information modified from American Heart Association (AHA): Advanced cardiac life support provider manual, 2006, American Heart Association.
Management of Hypotension/Shock: Suspected Pump Problem
Advanced life support
Marked Hypotension (Systolic BP less than 70 mm Hg)/Cardiogenic Shock
• Norepinephrine infusion—0.5–30 mcg/min until SBP 80 mm Hg.
• Then attempt to change to dopamine—5–15 mcg/kg/min until SBP 90 mm Hg.
• Dobutamine IV—2–20 mcg/kg/min can be given simultaneously in an attempt to reduce magnitude of dopamine infusion.
Consider balloon pump or patient transfer to a cardiac interventional facility.
Modified from Aehlert B: ACLS quick review study guide, ed 3, St Louis, 2007, Mosby. Additional information modified from American Heart Association (AHA): Advanced cardiac life support provider manual, 2006, American Heart Association.
Management of Hypotension/Shock: Suspected Volume Problem
Advanced life support
Hypotension: Suspected Volume (or Vascular Resistance) Problem
Modified from Aehlert B: ACLS quick review study guide, ed 3, St Louis, 2007, Mosby. Additional information modified from American Heart Association (AHA): Advanced cardiac life support provider manual, 2006, American Heart Association.
Management of Hypotension/Shock: Suspected Rate Problem
Modified from Aehlert B: ACLS quick review study guide, ed 3, St Louis, 2007, Mosby. Additional information modified from American Heart Association (AHA): Advanced cardiac life support provider manual, 2006, American Heart Association.