CASE 3
John, a 12-month-old boy with severe gram-positive bacterial pneumonia, has been referred to the local pediatric hospital by the family’s general practitioner. In addition to the fact that this is his fourth such infection in 6 months, he has had recurrent diarrhea (Giardia lamblia) and his tonsils/adenoids are barely detectable. As well, John is below the norm for height and weight. He has received the recommended DTaP (diphtheria, tetanus toxoids, and acellular pertussis) pediatric immunizations (see Fig. 45-1). John has three healthy sisters aged 3, 5, and 7 years. The family lost a boy at 10 months of age to bacterial pneumonia 8 years ago. Blood test results show low total serum immunoglobulin levels, few B cells, but normal numbers and functioning of T cells. All tests for macrophage/neutrophil function and number are normal. Medical and family histories, as well as blood test results, were included in the file that the family physician sent to the hospital. How would you proceed?
QUESTIONS FOR GROUP DISCUSSION
RECOMMENDED APPROACH
Implications/Analysis of Family History
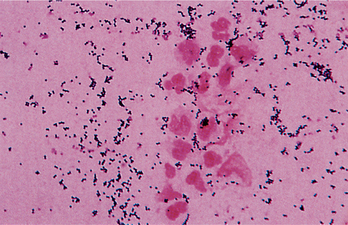
John has three sisters, but they have not presented with severe and recurrent gram-positive bacterial infections (Fig. 3-1). On the other hand, the family has lost a boy to bacterial pneumonia, suggesting that this is an X-linked recessive immunodeficiency disorder. That is, the gene that is missing or mutated is present on the X chromosome. Because females have two X chromosomes, a gene mutation on one chromosome will not manifest as an immunodeficiency disorder when there is a normal copy of that gene on the other chromosome. Nonetheless, the female remains a carrier and can pass the defective gene to her offspring. Females who inherit two defective genes will also present with the disorder. In contrast, males have only one X chromosome and if a gene on that chromosome is mutated, the child will develop the associated disorder. Although identification of males with a similar disorder helps in the diagnosis, the absence of other affected male infants does not rule out a diagnosis of an X-linked disorder.
Implications/Analysis of Clinical History
John’s problems with infections did not begin until he was several months of age, suggesting that prior to this he was protected against infection by maternally transmitted IgG antibodies. Because IgG antibodies have a half-life of about 3 weeks, the maternal IgG anti-bodies that have crossed the placenta will protect the infant for the first few months of life.
Implications/Analysis of Laboratory Investigation
Quantitative assessment of serum immunoglobulin using either nephelometry (see Case 5) or enzyme-linked immunosorbent assay (ELISA) (see Case 7) indicated that serum immunoglobulin levels were below normal (normal pediatric level: see Appendix). B cell numbers, assessed by flow cytometry using fluorescently labeled anti-CD19 antibodies, were also below normal. CD19 is a B cell marker that is initially expressed during the pro–B cell stage and continues to be expressed at all stages of B cell development, including the mature B cell. A CD19+ B cell count of less than 100 mg/dL is suggestive of a primary immunodeficiency: X-linked agammaglobulinemia (XLA).
Although bacterial infections can also result from defects in the complement system, the low B cell numbers, low serum IgG, undetectable titers to immunization antigens, and defect in B cell function suggest that this is not a complement dysfunction. However, a complement defect could be ruled out by measuring the overall activation of both the classical (CH50) and alternative (AH50) pathways (see Case 11).
DIAGNOSIS
John was diagnosed with X-linked agammaglobulinemia (Bruton’s hypo- or agammaglobulinemia).
THERAPY
Gamma Globulin Therapy
Conventional treatment involves the life-long replacement of the defective components (i.e., serum immunoglobulin replacement). Passive immunization with monthly intravenous injections of pooled gamma globulins (˜500 mg/kg administered over ˜4 hours) that contain IgG against a broad spectrum of bacteria, viruses, and parasites is recommended. Because many of these patients are IgA deficient the immune globulin selected must not contain any IgA, to avoid possible anaphylaxis (see Case 5).