CASE 28

1. What should be included in the differential diagnosis for the appearance of the heart on the radiograph? (Choose all that apply.)
2. What is the most likely diagnosis?
3. What finding is most specific for a malignant effusion?
B. Nodularity
C. Thickening
D. Enhancement
4. What does pulsus paradoxus indicate?
A. Tamponade
B. Tumor
C. Constriction
D. Hemorrhage
ANSWERS
Reference
Yared K, Baggish AL, Picard MH, et al. Multimodality imaging of pericardial diseases. JACC Cardiovasc Imaging. 2010;3(6):650–660.
Cross-Reference
Cardiac Imaging: The REQUISITES, ed 3, pp 265–267.
Comment
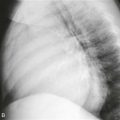
Radiographic Features
A small pericardial effusion is frequently not identified on chest radiography. As the pericardial effusion increases, the cardiac silhouette may acquire a globular (“water bottle”) configuration, which results from obscuration of the normal bulges and indentations of the cardiac contours (Fig. A). Because a pericardial effusion can cause enlargement of the cardiac silhouette, it may be difficult to distinguish pericardial effusion from cardiomegaly on chest radiographs. One differentiating feature is obscuration of the hilar vessels by a large pericardial effusion, which does not occur with cardiomegaly alone. Sometimes a pericardial effusion can cause an opaque band between the pericardial fat and the subpericardial fat on a lateral chest film, known as the “fat pad” sign. Although this sign is specific, its sensitivity for pericardial effusion is limited.
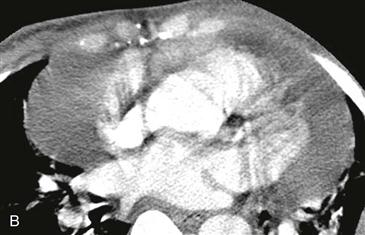
Cross-Sectional Imaging
Echocardiography is more sensitive than chest radiography for the diagnosis of pericardial effusion. When a pericardial effusion is suggested by clinical or radiographic findings, echocardiography can confirm the diagnosis. CT and MRI also can demonstrate pericardial effusion (Fig. B) and are useful for the identification of a hemorrhagic effusion and nodularity of the pericardium, both of which suggest a malignant effusion.