CHAPTER 27
Ulnar Neuropathy (Elbow)
Definition
The ulnar nerve is derived predominantly from the nerve roots of C8 and T1 with a small contribution from C7. The C8 and T1 fibers form the lower trunk of the brachial plexus. The ulnar nerve is the continuation of the medial cord of the brachial plexus at the level of the axilla.
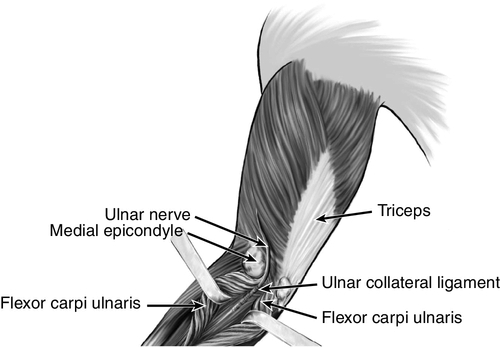
Ulnar neuropathy at the elbow is the second most common entrapment neuropathy. Only carpal tunnel syndrome (median neuropathy at the wrist) is more frequent. The ulnar nerve is susceptible to compression at the elbow for several reasons. First, the nerve has a superficial anatomic location at the elbow. Hitting the “funny bone” (ulnar nerve at the elbow) creates an unpleasant sensation that most people have experienced. If the ulnar nerve is susceptible to subluxation, further injury may result. Second, the nerve is prone to repeated trauma from leaning on the elbow or repetitively flexing and extending the elbow. Poorly healing fractures at the elbow may damage this nerve. Finally, and perhaps most important, the ulnar nerve can become entrapped at the arcade of Struthers, in the cubital tunnel (ulnar collateral ligament and aponeurosis between the two heads of the flexor carpi ulnaris; Fig. 27.1), or within the flexor carpi ulnaris muscle. The nerve lengthens and becomes taut with elbow flexion. In addition, there is decreased space in the cubital tunnel in this position. The volume of the cubital tunnel is maximal in extension and can decrease by 50% with elbow flexion [1]. The nerve may also become compromised after a distal humerus fracture, either as a direct result of the fracture or because of an altered carrying angle of the elbow and decreased elbow extension (tardy ulnar palsy). Repetitive or incorrect throwing can lead to damage of the ulnar nerve at the elbow [2]. Biomechanical risk factors (repetitive holding of a tool in one position), obesity, and other associated upper extremity work-related musculoskeletal disorders (especially medial epicondylitis and other nerve entrapment disorders) have also been associated with the development of ulnar neuropathy at the elbow [3].
Symptoms
If the ulnar nerve is entrapped at the elbow, both the dorsal ulnar cutaneous nerve (which arises just proximal to the wrist) and the palmar cutaneous branch of the ulnar nerve will be affected. Patients will therefore complain of numbness or paresthesias in the dorsal and volar aspects of the fifth and ulnar side of the fourth digits. Hand intrinsic muscle weakness may be apparent. In cases of severe ulnar neuropathy, clawing of the fourth and fifth digits (with attempted hand opening) and atrophy of the intrinsic muscles may be noted by the patient (Fig. 27.2). Symptoms may be exacerbated by elbow flexion. Pain may be noted and may radiate proximally or distally.
Physical Examination
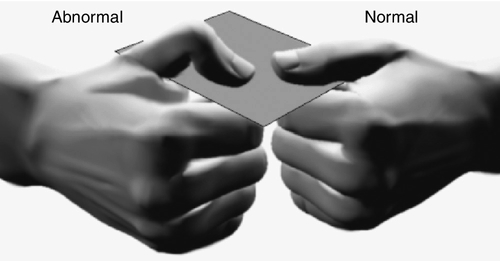
The ulnar nerve may be palpable in the posterior condylar groove (posterior to the medial epicondyle) with elbow flexion and extension. A Tinel sign may be present at the elbow; however, it should be considered significant only if the Tinel sign is absent on the nonaffected side. The ulnar nerve may be felt subluxing with flexion and extension of the elbow. Sensory deficits may be noted in the fifth and ulnar half of the fourth digits. Atrophy of the intrinsic hand muscles and hand weakness may be noted as well (although this is generally seen in more advanced cases). Wartenberg sign (abduction of the fourth and fifth digits) may occur. The patient should be tested for Froment sign. Here, a patient is asked to grasp a piece of paper between the thumb and radial side of the second digit. The examiner tries to pull the paper out of the patient’s hand. If the patient has injury to the adductor pollicis muscle (ulnar innervated), the patient will try to compensate by using the median-innervated flexor pollicis longus muscle (Fig. 27.2).
Functional Limitations
The patient with ulnar neuropathy at the elbow may have poor hand function and complain of dropping things or clumsiness. There may be difficulty with activities of daily living, such as dressing, holding a pen, or using keys.
Diagnostic Studies
Electrodiagnostic studies can help identify, localize, and gauge the severity of an ulnar nerve lesion at the elbow. The findings of abnormal spontaneous potentials (fibrillations and positive sharp waves) in ulnar innervated muscles on needle electromyographic study indicate axonal damage and portend a worse prognosis than with injury to the myelin only. Slowing of the ulnar nerve across the elbow or conduction block (a drop in compound motor action potential amplitude across the elbow) indicates myelin injury. These studies can also identify other areas of nerve compression that may accompany ulnar neuropathy at the elbow. Several studies using ultrasound have shown an increased cross-sectional area of the ulnar nerve in patients with ulnar neuropathy at the elbow [4,5]. Magnetic resonance neurography may play a role in the evaluation of ulnar neuropathy at the elbow [6]. Radiographs of the elbow with cubital tunnel views can be obtained if fractures, spurs, arthritis, and trauma are suspected. In rare cases, magnetic resonance imaging [7] with arthrography may be used to assess for tears in the ulnar collateral ligament or soft tissue disease.
Treatment
Initial
Treatment initially involves relative rest and protecting the elbow. Elbow pads or night splinting in mild flexion may be beneficial. Treatment should be directed at avoidance of aggravating biomechanical factors, such as leaning on the elbows, prolonged or repetitive elbow flexion, and repetitive valgus stress in throwing. Nonsteroidal anti-inflammatory drugs may also be prescribed.
Rehabilitation
Successful rehabilitation of ulnar neuropathy at the elbow includes identification and correction of biomechanical factors. This may include workstation modifications to decrease the amount of elbow flexion, substitution of headphones for telephone handsets, and use of forearm rests. Often, an elbow pad can be beneficial; the pad protects the ulnar nerve and keeps the elbow in relative extension. A rehabilitation program should include strengthening of forearm pronator and flexor muscles. Flexibility exercises should be instituted to maintain range of motion and to prevent soft tissue tightness. Advanced strengthening, including eccentric and dynamic joint stabilization exercises, can be added [8,9].
Procedures
Procedures are not typically performed to treat ulnar neuropathy at the elbow.
Surgery
If conservative management has failed or if significant damage to the ulnar nerve is evident, surgery may be considered [10–12]. The type of surgery depends on the area of ulnar nerve injury and may involve release of the cubital tunnel, ulnar nerve transposition [13], decompression of the ulnar nerve (open or arthroscopic) [14,15], subtotal medial epicondylectomy [16,17], or ulnar collateral ligament repair. Simple decompression and decompression with transposition have been shown to be equally effective in idiopathic ulnar neuropathy at the elbow [18].
Potential Disease Complications
If ulnar neuropathy at the elbow is left untreated, complications may include hand weakness, poor coordination, intrinsic muscle atrophy, sensory loss, and pain. In addition, flexion contractures and valgus deformity may develop at the elbow [8].
Potential Treatment Complications
The results of surgery depend on the extent of ulnar nerve compression, accuracy of identifying the site of compression, type of procedure, thoroughness of compression release, comorbid factors, degree of prior intrinsic muscle loss, and previous sensory loss [8,19–23]. Nonsteroidal anti-inflammatory drugs may cause gastric, hepatic, or renal complications.







