CASE 27 Loss of Side Branch During Right Coronary Intervention
Cardiac catheterization
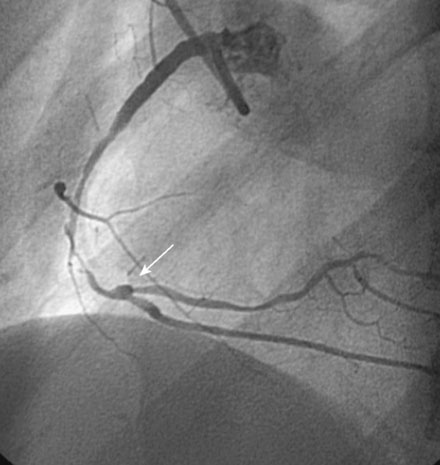
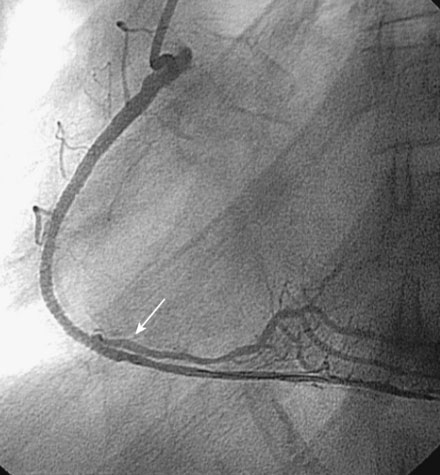
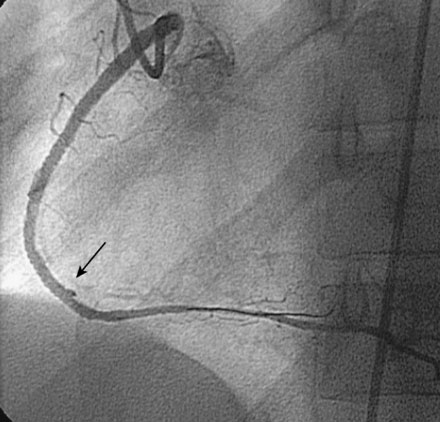
Catheterization was performed during the hospital admission. Left ventricular function appeared normal and there was no significant disease noted in the left coronary artery (Figure 27-1); however, collateral filling of the distal right coronary artery was noted. The right coronary artery arose aberrantly high and anterior in the right coronary sinus. Heavy calcification along with severe atherosclerotic narrowing affected the midportion of the right coronary artery, and atherosclerotic disease also narrowed the ostium of the posterolateral side branch (Figures 27-2, 27-3 and Videos 27-1, 27-2).

FIGURE 27-1 This is a representative left coronary angiogram. There is no significant obstructive disease noted.
Her physician decided to proceed with percutaneous coronary intervention of the right coronary artery. Adequate backup for intervention required a left Amplatz 2.0 guide catheter. Procedural anticoagulation included intravenous bolus of heparin (50 U/kg) and double bolus plus infusion of eptifibatide using standard doses. The operator predilated the stenotic segment with a 2.5 mm diameter by 30 mm long compliant balloon, and chose bare-metal stents because of concern about the patient’s compliance with long-term clopidogrel. Two stents successfully treated the diseased segment with a 2.5 mm diameter by 18 mm long stent placed distally and a 3.0 mm diameter by 28 mm long stent deployed proximally (Figure 27-4 and Video 27-3). At this point, the ostium of the posterolateral branch appeared narrowed but remained patent. Noncompliant balloons (2.5 mm diameter by 20 mm long distally and 3.5 mm diameter by 15 mm long proximally) inflated to high pressure were used to postdilate the stented segment. Angiography after high-pressure balloon inflations demonstrated improved appearance of the stented segment but occlusion of the posterolateral side branch (Figures 27-5, 27-6 and Videos 27-4, 27-5). Although the operator was able to pass a hydrophilic guidewire into the side branch, it was not possible to pass a 2.0 mm diameter by 15 mm long compliant balloon and the side branch remained closed. The patient left the cardiac catheterization laboratory with ongoing mild chest pain, but her rhythm and blood pressure remained stable and she was transferred to a telemetry unit for monitoring.
Discussion
Percutaneous management of lesions involving the bifurcation of a side branch can prove challenging. The chief concern relates to the potential loss of the side branch; this event may cause a periprocedural myocardial infarction and result in significant morbidity if the side branch is large. The risk of side branch closure depends on the location of the atheroma. The highest risk of closure occurs when atheroma surrounds and also involves the ostium of the side branch; in such cases, almost 70% of side branches will close following stenting of the main vessel.1 The risk is lowest when the side branch ostium is free of involvement; closure complicates only about 6% of such cases.1 As shown in the case presented here, most side branches occlude after post-stent dilatation with a high-pressure balloon. However, closure may also occur after pre-stent balloon inflation or after initial stent deployment.
Different treatment strategies to treat bifurcation lesions have been proposed, but it appears that optimal outcomes are obtained using a simple strategy of stenting only the main vessel with provisional stenting of the side branch performed only if an unacceptable result is obtained in the side branch.2 In the author’s experience, the “crush” stent technique is the most reliable method of preserving large side branches, but is associated with a high rate of restenosis and stent thrombosis particularly if a final “kissing” balloon cannot be performed.3
1 Aliabadi D., Tillis F.V., Bowers T.R., Benjuly K.H., Safian R.D., Goldstein J.A., Grines C.L., O’Neill W.W. Incidence and angiographic predictors of side branch occlusion following high-pressure intracoronary stenting. Am J Cardiol. 1997;80:994-997.
2 Steigen T.K., Maeng M., Wiseth R., et al. Nordic PCI Study Group Randomized study on simple versus complex stenting of coronary artery bifurcation lesions: the Nordic Bifurcation Study. Circulation. 2006;114:1955-1961.
3 Hoye A., Iakovou I., Ge L., van Mieghem C.A.G., Ong A.T.L., Cosgrave J., Sangiorgi GM Airoldi F., Montorfano M., Michev I., Chieffo A., Carlino M., Corvaja N., Aoki J., Granillo G.A.R., Valgimigli M., Sianos G., van der Giessen W.J., de Feyter P.J., van Domburg R.T., et al. Long-term outcomes after stenting of bifurcation lesions with the “crush” technique: Predictors of an adverse outcome. J Am Coll Cardiol. 2006;47:1949-1958.