Procedure 27 Flexor Carpi Ulnaris–to–Extensor Carpi Radialis Brevis Transfer
Examination/Imaging
Clinical Examination
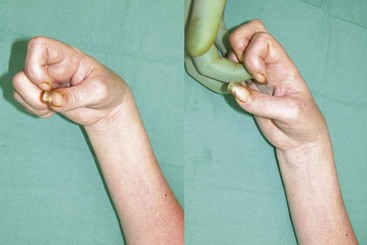
 Cerebral palsy: The flexion deformity in cerebral palsy can be due to spasticity of the wrist flexors, weak wrist extensors, and/or a volar wrist capsular contracture. It is important to differentiate among these causes. An attempt at overcoming muscle spasticity should be done by applying gentle sustained resistance to the spastic force. If the wrist can be extended passively, it rules out capsular contracture. If the wrist cannot be extended passively, but the wrist flexors do not feel spastic, it suggests a wrist capsular contracture. If the spasticity cannot be overcome, a median and ulnar nerve block at the elbow can temporarily eliminate the flexor spasticity and allow an assessment of active and passive wrist extension. An FCU-to–extensor carpi radialis brevis (ECRB) transfer is indicated in patients who have a spastic FCU and good passive wrist extension (no capsular contracture) but lack active wrist extension. Before considering an FCU-to-ECRB transfer, one must ensure that the patient has the following:
Cerebral palsy: The flexion deformity in cerebral palsy can be due to spasticity of the wrist flexors, weak wrist extensors, and/or a volar wrist capsular contracture. It is important to differentiate among these causes. An attempt at overcoming muscle spasticity should be done by applying gentle sustained resistance to the spastic force. If the wrist can be extended passively, it rules out capsular contracture. If the wrist cannot be extended passively, but the wrist flexors do not feel spastic, it suggests a wrist capsular contracture. If the spasticity cannot be overcome, a median and ulnar nerve block at the elbow can temporarily eliminate the flexor spasticity and allow an assessment of active and passive wrist extension. An FCU-to–extensor carpi radialis brevis (ECRB) transfer is indicated in patients who have a spastic FCU and good passive wrist extension (no capsular contracture) but lack active wrist extension. Before considering an FCU-to-ECRB transfer, one must ensure that the patient has the following:
 Neonatal brachial plexus palsy (NBPP): The ulnar deviation deformity in this group of patients can be due to the FCU or the extensor carpi ulnaris (ECU). Either one of these tendons can be used for obtaining wrist extension depending on the predominant cause of the ulnar deviation deformity. In NBPP, the FCU is passed around the radius to the extensor carpi radialis longus (ECRL) to get some radial balance to the hand at the wrist. In cerebral palsy, the transfer is made around the ulna to the ECRB. This chapter describes the procedure in cerebral palsy.
Neonatal brachial plexus palsy (NBPP): The ulnar deviation deformity in this group of patients can be due to the FCU or the extensor carpi ulnaris (ECU). Either one of these tendons can be used for obtaining wrist extension depending on the predominant cause of the ulnar deviation deformity. In NBPP, the FCU is passed around the radius to the extensor carpi radialis longus (ECRL) to get some radial balance to the hand at the wrist. In cerebral palsy, the transfer is made around the ulna to the ECRB. This chapter describes the procedure in cerebral palsy.
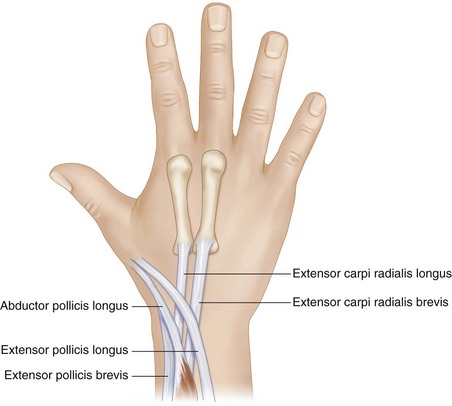
Surgical Anatomy
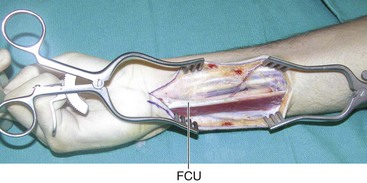
 The purely tendinous portion of the FCU is quite short as the muscle extends distally along the tendon. In addition, the muscle is attached along the ulna over a long distance. The muscle must be detached quite proximally to have adequate excursion of the transferred FCU (Fig. 27-2).
The purely tendinous portion of the FCU is quite short as the muscle extends distally along the tendon. In addition, the muscle is attached along the ulna over a long distance. The muscle must be detached quite proximally to have adequate excursion of the transferred FCU (Fig. 27-2).
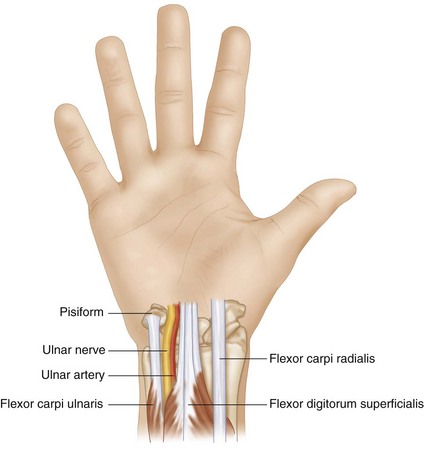
 The ulnar artery and nerve are very closely related to the undersurface of the FCU and must be protected during mobilization of the FCU (Fig. 27-3).
The ulnar artery and nerve are very closely related to the undersurface of the FCU and must be protected during mobilization of the FCU (Fig. 27-3).
Exposures
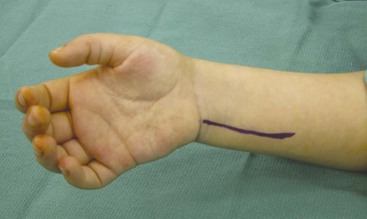
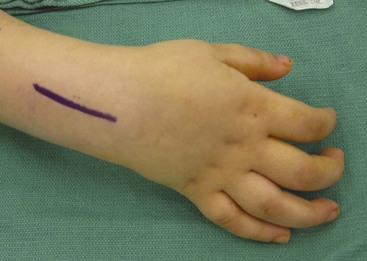
 A 4-cm longitudinal incision over the volar forearm extending proximally from the pisiform is made, in line with the palpable FCU tendon (Fig. 27-4). Skin and subcutaneous tissue are dissected, and the FCU tendon is exposed.
A 4-cm longitudinal incision over the volar forearm extending proximally from the pisiform is made, in line with the palpable FCU tendon (Fig. 27-4). Skin and subcutaneous tissue are dissected, and the FCU tendon is exposed.
 A 6-cm longitudinal incision over the dorsal forearm extending proximally from the base of the long finger metacarpal is made (Fig. 27-5). Skin and subcutaneous tissue are dissected to expose the extensor retinaculum. The second dorsal extensor compartment is opened, and the tendons of the ECRL and ECRB are identified.
A 6-cm longitudinal incision over the dorsal forearm extending proximally from the base of the long finger metacarpal is made (Fig. 27-5). Skin and subcutaneous tissue are dissected to expose the extensor retinaculum. The second dorsal extensor compartment is opened, and the tendons of the ECRL and ECRB are identified.
Procedure
Step 1
Step 2
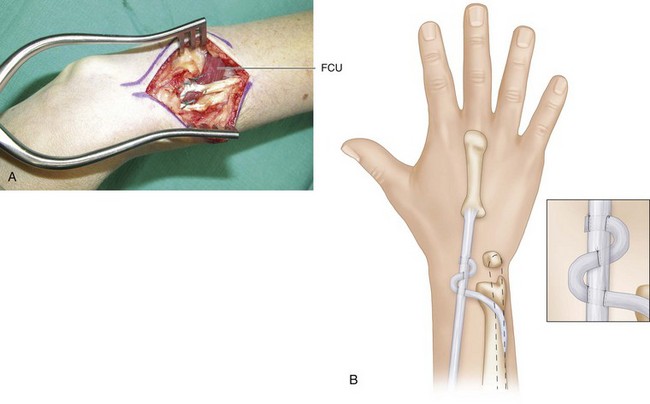
 The FCU tendon is passed around the ulnar aspect of the forearm, over the skin, to the point where it intersects with the ECRB. The route of the FCU tendon is marked.
The FCU tendon is passed around the ulnar aspect of the forearm, over the skin, to the point where it intersects with the ECRB. The route of the FCU tendon is marked.
 A wide subcutaneous tunnel is made along the route from the dorsal incision to the volar incision, and the FCU tendon is delivered in the dorsal wound.
A wide subcutaneous tunnel is made along the route from the dorsal incision to the volar incision, and the FCU tendon is delivered in the dorsal wound.
Step 2 Pearls
It is important to make the subcutaneous tunnel along the shortest, most direct route between these two tendons. Otherwise, the transferred tendon will move over time into the shortest route. This will make the transferred tendon lax and less effective.
The tendon is passed superficial to the extensor tendons of the first and third compartments (adductor pollicis longus [APL], extensor pollicis brevis [EPB], and extensor pollicis longus [EPL]) (Fig. 27-7).
Step 3
 The FCU tendon is weaved into the ECRB tendon using the Pulvertaft weave with 3-0 Ethibond suture (Fig. 27-8A and B).
The FCU tendon is weaved into the ECRB tendon using the Pulvertaft weave with 3-0 Ethibond suture (Fig. 27-8A and B).
 The tension is set with the wrist in neutral or 30 degrees of flexion. One must not overtighten the transfer to achieve wrist extension beyond neutral because the patient typically does not have sufficiently strong finger extensors to extend the fingers and will rely on tenodesis effect with the wrist in flexion to extend the fingers (Fig. 27-9).
The tension is set with the wrist in neutral or 30 degrees of flexion. One must not overtighten the transfer to achieve wrist extension beyond neutral because the patient typically does not have sufficiently strong finger extensors to extend the fingers and will rely on tenodesis effect with the wrist in flexion to extend the fingers (Fig. 27-9).
Postoperative Care and Expected Outcomes
 The patient’s wrist is splinted in neutral position for 4 weeks, followed by range-of-motion exercises. The patient wears a removable splint for an additional 4 weeks. Most patients can extend the wrist actively, but if spasticity is not controlled, they may develop recurrent wrist contracture. These patients are advised to wear a volar wrist extension splint at night.
The patient’s wrist is splinted in neutral position for 4 weeks, followed by range-of-motion exercises. The patient wears a removable splint for an additional 4 weeks. Most patients can extend the wrist actively, but if spasticity is not controlled, they may develop recurrent wrist contracture. These patients are advised to wear a volar wrist extension splint at night.
 This transfer has shown good results with improvements in resting wrist posture and arc of wrist motion. However, it is associated with a loss in wrist flexion, and the range of motion usually remains unchanged.
This transfer has shown good results with improvements in resting wrist posture and arc of wrist motion. However, it is associated with a loss in wrist flexion, and the range of motion usually remains unchanged.
Thometz JG, Tachdjian M. Long-term follow-up of the flexor carpi ulnaris transfer in spastic hemiplegic children. J Pediatr Orthop. 1988;8:407-412.
Tonkin M, Gschwind C. Surgery for cerebral palsy. Part 2: flexion deformity of the wrist and fingers. J Hand Surg [Am]. 1992;17:396-400.
Wolf TM, Clinkscales CM, Hamlin C. Flexor carpi ulnaris tendon transfer in cerebral palsy. J Hand Surg [Am]. 1998;23:340-343.