CHAPTER 27 Arterial Catheterization and Pressure Monitoring
3 What are the indications for intra-arterial blood pressure monitoring?
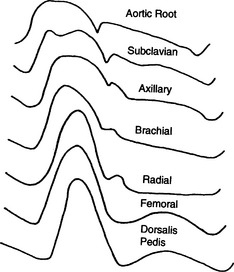
10 How does a central waveform differ from a peripheral waveform?
As the arterial pressure is transmitted from the central aorta to the peripheral arteries, the waveform is distorted (Figure 27-1). Transmission is delayed, high-frequency components such as the dicrotic notch are lost, the systolic peak increases, and the diastolic trough is decreased. The changes in systolic and diastolic pressures result from a decrease in the arterial wall compliance and from resonance (the addition of reflected waves to the arterial waveform as it travels distally in the arterial tree). The systolic blood pressure in the radial artery may be as much as 20 to 50 mm Hg higher than the pressure in the central aorta.
11 What information can be obtained from an arterial waveform?
The arterial waveform provides valuable information about the patient’s hemodynamic status:
 The waveform determines the heart rate during electrocardiographic electrocautery interference and whether the electrical spikes from a pacemaker result in ventricular contractions.
The waveform determines the heart rate during electrocardiographic electrocautery interference and whether the electrical spikes from a pacemaker result in ventricular contractions.KEY POINTS: Arterial Catheterization and Pressure Monitoring 
12 How is the arterial waveform reproduced?
Reproduction of the arterial waveform requires the following equipment:
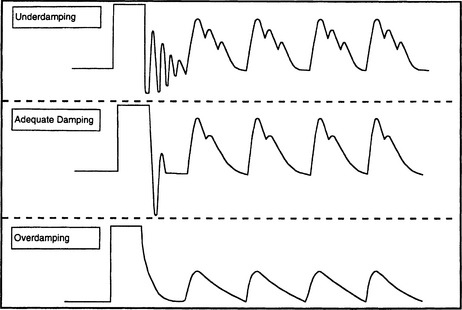
14 What are the characteristics of overdamped and underdamped monitoring systems?
The damping coefficient is estimated by evaluating the time for the system to settle to zero after a high-pressure flush (Figure 27-2). An underdamped system continues to oscillate for three or four cycles; it overestimates the systolic and underestimates the diastolic blood pressure. An overdamped system settles to baseline slowly without oscillating; it underestimates the systolic and overestimates the diastolic blood pressure. However, in both cases the mean blood pressure is relatively accurate.
15 How can the incidence of artifacts in arterial monitoring systems be reduced?
The incidence of artifacts can be reduced by meticulous care of the monitoring system:
 The connecting tubing should be rigid with an internal diameter of 1.5 to 3 mm and a maximal length of 120 cm.
The connecting tubing should be rigid with an internal diameter of 1.5 to 3 mm and a maximal length of 120 cm. The mechanical coupling system should be flushed with saline to maintain the patency of the arterial line and minimize the risk of distal embolization and nosocomial infection.
The mechanical coupling system should be flushed with saline to maintain the patency of the arterial line and minimize the risk of distal embolization and nosocomial infection.1. Barbeito A., Mark J.B. Arterial and central venous pressure monitoring. Anesthesiol Clin. 2006;24:717-735.
2. Murphy G.S., Szokol J.W., Marymont J.H., et al. Retrograde blood flow in the brachial and axillary arteries during routine radial arterial catheter flushing. Anesthesiology. 2006;105:492-497.
3. Tuncali B.E., Kuvaki B., Tuncali B., et al. A comparison of the efficacy of heparinized and nonheparinized solutions for maintenance of perioperative radial arterial catheter patency and subsequent occlusion. Anesth Analg. 2005;100:1117-1121.