Thoracentesis (Perform)
Thoracentesis (Perform)
PREREQUISITE NURSING KNOWLEDGE
• Thoracentesis is performed with insertion of a needle or a catheter into the pleural space, which allows for removal of pleural fluid.
• Pleural effusions are defined as the accumulation of fluid in the pleural space that exceeds 10 to 20 mL and results from the overproduction of fluid or disruption in fluid reabsorption.1
• Thoracentesis is not used to verify the presence of pleural effusion. Diagnosis of pleural effusion is made via clinical examination, patient symptoms, and diagnostic techniques. A number of techniques can demonstrate pleural effusion with varying levels of sensitivity. Percussion requires a minimum of 300 to 400 mL for identification of a pleural effusion, whereas a standard chest radiography requires 200 to 300 mL. Lateral decubitus radiographs can be used to recognize smaller fluid amounts and highlight whether present fluid is free flowing. Ultrasound scan, computed tomography (CT) scan, and magnetic resonance imaging (MRI) technology can detect 100 mL of fluid with 100% sensitivity.1 Therefore, initial diagnosis of pleural effusion should use imaging techniques such as chest radiographs, ultrasound scans, CT scans, or MRI combined with patient symptoms and clinical examination findings.
• Diagnostic thoracentesis is indicated for differential diagnosis for patients with pleural effusion of unknown etiology. A diagnostic thoracentesis may be repeated if initial results fail to yield a diagnosis.
• Therapeutic thoracentesis is indicated to relieve the symptoms (e.g., dyspnea, cough, hypoxemia, or chest pain) caused by a pleural effusion.
• Pleural effusions are classified as either transudative or exudative effusions.
• Exudative effusions indicate a local etiology (e.g., pulmonary embolus, infection), whereas transudative effusions usually are associated with systemic etiologies (e.g., heart failure).
• Samples of pleural fluid are analyzed and assist in distinguishing between exudative and transudative etiologies of effusion. Results of laboratory tests on pleural fluid alone do not establish a diagnosis; instead the laboratory results must be correlated with the clinical findings and serum laboratory results.
• Exudative pleural effusions meet one of the following criteria1:
 Pleural fluid lactate dehydrogenase (LDH)-to-serum LDH ratio is greater than 0.6 international units/mL.
Pleural fluid lactate dehydrogenase (LDH)-to-serum LDH ratio is greater than 0.6 international units/mL.
 Pleural fluid LDH is more than two thirds of the upper limit of normal for serum LDH.
Pleural fluid LDH is more than two thirds of the upper limit of normal for serum LDH.
 Pleural fluid protein-to-serum protein ratio is greater than 0.5 g/dL.
Pleural fluid protein-to-serum protein ratio is greater than 0.5 g/dL.
• A transudative pleural effusion is considered when none of the exudative criteria is met and is usually associated with systemic etiologies (e.g., heart failure), whereas exudative effusions indicate a local etiology (e.g., pulmonary embolus, infection, open heart surgery).
• Relative contraindications for thoracentesis include the following:
 Patient anatomy that hinders the practitioner from clearly identifying the appropriate landmarks
Patient anatomy that hinders the practitioner from clearly identifying the appropriate landmarks
 Patients undergoing anticoagulation therapy or with an uncorrectable coagulation disorder
Patients undergoing anticoagulation therapy or with an uncorrectable coagulation disorder
 Patients receiving positive end-expiratory pressure (PEEP) therapy
Patients receiving positive end-expiratory pressure (PEEP) therapy
 Patients with splenomegaly, elevated left hemidiaphragm, or left-sided pleural effusion
Patients with splenomegaly, elevated left hemidiaphragm, or left-sided pleural effusion
 Patients with only one lung as a result of a previous pneumonectomy
Patients with only one lung as a result of a previous pneumonectomy
• Ultrasound scan–guided thoracentesis is thought to reduce complications, especially when used in the last four patient groups listed in the relative contraindications list.3,4
• Complications commonly associated with thoracentesis include:
• Recent studies have shown a reduction in complications with ultrasound scan–guided technique, especially when used in the last four patient groups listed in the relative contraindications list.4–6
• Pneumothorax is the most common postthoracentesis complication with a reported incidence rate between 3% and 30%.11
• Hemorrhagic complications are more likely to occur in elderly patients because of tortuosity of vessels.8
• Hypotension can occur as part of the vasovagal reaction during or hours after the procedure. If it occurs during the procedure, cessation of the procedure and atropine instillation may be necessary. If hypotension occurs after the procedure, it is likely the result of fluid shifting from pleural effusion reaccumulation. In this situation, the patient is likely to respond to fluid resuscitation.11
• Development of cough generally initiates toward the end of the procedure and should result in procedure cessation.
• Reexpansion pulmonary edema is thought to occur from overdraining of fluid too quickly. Limitation of this complication may be accomplished by minimizing fluid removal to 1000 mL,11 but at least one study found no correlation with drainage of up to 2000 mL as long as the patient was symptom free during the procedure.5
EQUIPMENT
Diagnostic Thoracentesis
• Baseline diagnostic study results (i.e., lateral decubitus chest radiograph, ultrasound imaging, CT scan, or MRI)
• Completed patient informed consent form
• Functional intravenous access
• Adhesive bandage or adhesive strip
• Intervention medications (opioid, sedative, or hypnotic agents, local anesthetic 1% or 2% lidocaine)
• One small needle (25-gauge, ⅝-inch long)
• 5-mL syringe for local anesthetic
• Three large needles (20- to 22-gauge, 1½ to 2 inches long)
• Pillow or blanket to be placed on side table
• Available: Atropine, oxygen, thoracostomy supplies, advanced cardiac life support (ACLS) equipment
Therapeutic Thoracentesis
The following equipment is needed in addition to equipment for diagnostic thoracentesis:
Additional equipment (to have available depending on patient need) includes the following:
• Two complete blood count (CBC) tubes
• One anaerobic and one aerobic media bottle for culture and sensitivity
Commercially prepackaged thoracentesis kits are available in some institutions
PATIENT AND FAMILY EDUCATION
• Explain the procedure and purpose for thoracentesis, including potential complications, such as pneumothorax, pain at insertion site, cough, infection, hypoxemia, and hypovolemia. Include an explanation of the amount of fluid expected to be withdrawn, duration of time the procedure may last, and expectation of and reason for coughing during or after thoracentesis.  Rationale: This communication identifies patient and family knowledge deficits concerning patient condition, procedure, expected benefits, and potential risks and allows time for questions to clarify information and voice concerns. Explanations decrease patient anxiety and enhance cooperation.
Rationale: This communication identifies patient and family knowledge deficits concerning patient condition, procedure, expected benefits, and potential risks and allows time for questions to clarify information and voice concerns. Explanations decrease patient anxiety and enhance cooperation.
• Explain the patient’s role in thoracentesis.  Rationale: This explanation increases patient compliance, facilitates needle and catheter insertion, and enhances fluid removal.
Rationale: This explanation increases patient compliance, facilitates needle and catheter insertion, and enhances fluid removal.
PATIENT ASSESSMENT AND PREPARATION
Patient Assessment
• Obtain a history of symptoms, occupational exposure, and medication usage
• Assess for signs and symptoms of pleural effusion:
 Trachea deviated away from the affected side
Trachea deviated away from the affected side
 Affected side dull to flat with percussion
Affected side dull to flat with percussion
 Absent or decreased breath sounds
Absent or decreased breath sounds
 Cough, weight loss, night sweats, anorexia, and malaise may also occur with pleural infection or malignancy disease10
Cough, weight loss, night sweats, anorexia, and malaise may also occur with pleural infection or malignancy disease10
 Rationale: Although physical findings may suggest a pleural effusion, radiography or other imaging studies confirm its presence.
Rationale: Although physical findings may suggest a pleural effusion, radiography or other imaging studies confirm its presence.
• Assess chest radiograph or other imaging findings.  Rationale: If at least half the hemidiaphragm is obliterated on erect anterior-posterior radiograph results, sufficient fluid is in the pleural space for a thoracentesis. Greater than 200 mL of fluid is considered abnormal in erect chest radiograph results. Lateral radiographs show blunting of the costophrenic angle with 50 mL. With a small amount of loculated fluid, however, a lateral decubitus radiograph should be obtained. Lateral decubitus radiographs assist with distinguishing between free moving fluid and pleural thickening. If the pleural effusion is measured to be greater than 10 mm deep on a lateral decubitus radiograph, a diagnostic thoracentesis can be performed. However, if the pleural effusion is measured to be less than 10 mm in diameter or loculated, ultrasound scan is necessary to distinguish between pleural effusion and pleural lesion. Ultrasound scan–guided thoracentesis may be necessary if a pleural effusion has been confirmed.8 In the intensive care setting, supine anterior-posterior radiographs are less sensitive in the identification of pleural effusions. In this setting, hazy opacification of one lung field or minor fissure thickening may be the only clues to the presence of a pleural effusion.10
Rationale: If at least half the hemidiaphragm is obliterated on erect anterior-posterior radiograph results, sufficient fluid is in the pleural space for a thoracentesis. Greater than 200 mL of fluid is considered abnormal in erect chest radiograph results. Lateral radiographs show blunting of the costophrenic angle with 50 mL. With a small amount of loculated fluid, however, a lateral decubitus radiograph should be obtained. Lateral decubitus radiographs assist with distinguishing between free moving fluid and pleural thickening. If the pleural effusion is measured to be greater than 10 mm deep on a lateral decubitus radiograph, a diagnostic thoracentesis can be performed. However, if the pleural effusion is measured to be less than 10 mm in diameter or loculated, ultrasound scan is necessary to distinguish between pleural effusion and pleural lesion. Ultrasound scan–guided thoracentesis may be necessary if a pleural effusion has been confirmed.8 In the intensive care setting, supine anterior-posterior radiographs are less sensitive in the identification of pleural effusions. In this setting, hazy opacification of one lung field or minor fissure thickening may be the only clues to the presence of a pleural effusion.10
 Posterior-anterior and lateral chest radiographs should be performed in all suspected pleural effusions.7
Posterior-anterior and lateral chest radiographs should be performed in all suspected pleural effusions.7
 Consider ultrasound scan guidance if the effusion is small, loculated, or on the side of an elevated hemidiaphram or if the patient is on mechanical ventilation or has a bleeding diathesis.7,8
Consider ultrasound scan guidance if the effusion is small, loculated, or on the side of an elevated hemidiaphram or if the patient is on mechanical ventilation or has a bleeding diathesis.7,8
 CT scans with contrast should be performed for pleural enhancement.7
CT scans with contrast should be performed for pleural enhancement.7
 In difficult drainage situations, CT scan should be used to delineate effusion size and position.7
In difficult drainage situations, CT scan should be used to delineate effusion size and position.7
• Assess medical history of pleuritic chest pain, malignancy disease, heart failure, and medication usage.  Rationale: Medical history may provide valuable clues to the cause of a patient’s pleural effusion or presence of hypercoagulable states as a result of medications. Knowledge of medication usage can indicate the need for anticoagulation reversal before invasive procedure. In addition, an increasing number of medications is noted to contribute to exudative effusions. Common examples include amiodarone, phenytoin, nitrofurantoin, and methotrexate. See www.pneumotox.com for a more comprehensive listing.7,10
Rationale: Medical history may provide valuable clues to the cause of a patient’s pleural effusion or presence of hypercoagulable states as a result of medications. Knowledge of medication usage can indicate the need for anticoagulation reversal before invasive procedure. In addition, an increasing number of medications is noted to contribute to exudative effusions. Common examples include amiodarone, phenytoin, nitrofurantoin, and methotrexate. See www.pneumotox.com for a more comprehensive listing.7,10
• Assess baseline vital signs, including pulse oximetry.  Rationale: Baseline assessment data provide information about patient status and allow for comparison during and after the procedure.
Rationale: Baseline assessment data provide information about patient status and allow for comparison during and after the procedure.
• Assess recent serum laboratory results, including the following:
 Rationale: These studies help determine whether the patient is at increased risk for bleeding. Generally, an INR of 1.3 or less is acceptable for invasive procedures.
Rationale: These studies help determine whether the patient is at increased risk for bleeding. Generally, an INR of 1.3 or less is acceptable for invasive procedures.
Patient Preparation
• Verify correct patient with two identifiers.  Rationale: Prior to performing a procedure, the nurse should ensure the correct identification of the patient for the intended intervention.
Rationale: Prior to performing a procedure, the nurse should ensure the correct identification of the patient for the intended intervention.
• Ensure that the patient understands preprocedural teachings. Answer questions as they arise and reinforce information.  Rationale: This communication evaluates and reinforces understanding of previously taught information.
Rationale: This communication evaluates and reinforces understanding of previously taught information.
• Obtain written informed consent for the procedure.  Rationale: Invasive procedures, unless performed with implied consent in a life-threatening situation, require written consent of the patient or significant other.
Rationale: Invasive procedures, unless performed with implied consent in a life-threatening situation, require written consent of the patient or significant other.
• Consider sedation or chemical paralysis.  Rationale: Sedation or chemical paralysis may be necessary to maximize positioning.
Rationale: Sedation or chemical paralysis may be necessary to maximize positioning.
• Have atropine available.  Rationale: Bradycardia, from a vasovagal reflex, is a common occurrence during thoracentesis.
Rationale: Bradycardia, from a vasovagal reflex, is a common occurrence during thoracentesis.
• Initiate pulse oximetry monitoring.  Rationale: Pulse oximetry provides a noninvasive means for monitoring oxygenation and heart rate at the bedside, which allows for prompt recognition and intervention should problems develop.
Rationale: Pulse oximetry provides a noninvasive means for monitoring oxygenation and heart rate at the bedside, which allows for prompt recognition and intervention should problems develop.
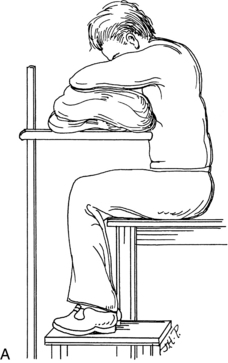
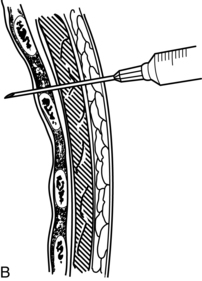
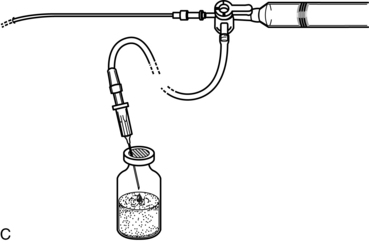
Figure 26-1 Thoracentesis. A, Ideal patient position for thoracentesis. B, Ideal placement of needle insertion. C, Attach catheter to three way stopcock syringe and vacutainer. Barton ED: Thoracentesis. In Rosen, P., Chan, T.C., Vilke, M., Sternbach, G., editors: Atlas of Emergency Procedures (pp. 36-37), St. Louis: Mosby.
References
![]() 1. Barton, E. Thoracentesis. In: Rosen P, Chan T, Vilke G, et al, eds. Atlas of emergency procedures. St Louis: Mosby, 2001.
1. Barton, E. Thoracentesis. In: Rosen P, Chan T, Vilke G, et al, eds. Atlas of emergency procedures. St Louis: Mosby, 2001.
![]() 2. Colt, HG, Brewer, N, Barbur, EB. Evaluation of patient–related and procedure-related factors contributing to -pneumothorax following thoracentesis. Chest. 1999; 116:134–138.
2. Colt, HG, Brewer, N, Barbur, EB. Evaluation of patient–related and procedure-related factors contributing to -pneumothorax following thoracentesis. Chest. 1999; 116:134–138.
![]() 3. Doyle, JJ, et al. Necessity of routine chest roentgenography after thoracentesis. Ann Intern Med. 1996; 124:816–820.
3. Doyle, JJ, et al. Necessity of routine chest roentgenography after thoracentesis. Ann Intern Med. 1996; 124:816–820.
![]() 4. Gervais, DA, et al, US-guided thoracentesis. requirement for post procedure chest radiography in patients who -receive mechanical ventilation versus patients who breathe spontaneously. Radiology 1997; 204:503–506.
4. Gervais, DA, et al, US-guided thoracentesis. requirement for post procedure chest radiography in patients who -receive mechanical ventilation versus patients who breathe spontaneously. Radiology 1997; 204:503–506.
![]() 5. Jones, PW, et al, Ultrasound-guided thoracentesis. is it a safer method. Chest 2003; 123:418–423.
5. Jones, PW, et al, Ultrasound-guided thoracentesis. is it a safer method. Chest 2003; 123:418–423.
![]() 6. Lichtenstein, D, et al. Feasibility and safety of ultrasound-aided thoracentesis in mechanically ventilated patients. Intensive Care Med. 1999; 25:955–958.
6. Lichtenstein, D, et al. Feasibility and safety of ultrasound-aided thoracentesis in mechanically ventilated patients. Intensive Care Med. 1999; 25:955–958.
![]() 7. Maskell, NA, Butland, RJA. BTS guidelines for the investigation of a unilateral pleural effusion in adults. Thorax. 2003; 58:ii8.
7. Maskell, NA, Butland, RJA. BTS guidelines for the investigation of a unilateral pleural effusion in adults. Thorax. 2003; 58:ii8.
![]() 8. Parsons, P, Tu, Y. Thoracentesis and percutaneous pleural biopsy. In: Parsons P, Heffner J, eds. Pulmonary respiratory therapy secrets. Philadelphia: Mosby, 1997.
8. Parsons, P, Tu, Y. Thoracentesis and percutaneous pleural biopsy. In: Parsons P, Heffner J, eds. Pulmonary respiratory therapy secrets. Philadelphia: Mosby, 1997.
![]() 9. Qureshi, N, Momin, ZA, Brandstetter, RD. Thoracentesis in clinical practice. Heart Lung. 1994; 23:376–383.
9. Qureshi, N, Momin, ZA, Brandstetter, RD. Thoracentesis in clinical practice. Heart Lung. 1994; 23:376–383.
10. Rahman, N, Chapman, S, Davies, R, Pleural effusion. a structured approach to care. Br Med Bull. 2005; 72(1):31–47.
![]() 11. Wilson, M, Irwin, R, Thoracentesis. Procedures and techniques in intensive care medicine. Lippincot & Williams & Wilkins, Philadelphia, 2003.
11. Wilson, M, Irwin, R, Thoracentesis. Procedures and techniques in intensive care medicine. Lippincot & Williams & Wilkins, Philadelphia, 2003.
Antunes, G, Neville, E, Duffy, J, et al. BTS guidelines for the management of malignant pleural effusions. Thorax. 2003; 58(Suppl 2):ii29–38.
Davies, CWH, Gleeson, FV, Davies, RJO. BTS guidelines for the management of pleural infection. Thorax. 2003; 58:ii18.
Heffner, JE, Brown, LK, Barbieri, CA. Diagnostic value of tests that discriminate between exudative and transudative -pleural effusions. Chest. 1997; 111:970–980.
Light, RW, et al, Pleural effusion. the diagnostic separation of transudates and exudates. Ann Intern Med 1992; 77:507–513.
Loddenkemper, R. Pleural effusions. In: Albert R, Spiro S, Jett J, eds. Clinical respiratory medicine. Philadelphia: Mosby, 2004.
Mayo, PH, Goltz, HR, Tafreshi, M, et al. Safety of ultrasound-guided thoracentesis in patients receiving mechanical -ventilation. Chest. 2004; 125(3):1059–1062.
Peterson, WG, Zimmerman, R. Limited utility of chest -radiograph after thoracentesis. Chest. 2000; 117:1038–1042.
Quigley, RL. Thoracentesis and chest tube drainage. Crit Care Clin. 1995; 11:111–126.
Thomsen, TW, DelaPena, J, Stenik, GS. Thoracentesis, Videos in clinical medicine 355/e16(15). retrieved from http://-content.nejm.org/cgi/content/video_preview/355/15/e16, 09/14/2008. [accessed].