CHAPTER 26 Pulmonary Artery Catheterization
3 What other hemodynamic variables can be measured or calculated from the pulmonary artery catheter? What are their normal values?
4 In what surgical procedures are pulmonary artery catheters most likely to be placed? What medical problems might influence a clinician’s likelihood to insert a pulmonary artery catheter before surgery?
8 How might kinking of the pulmonary artery catheter be avoided?
KEY POINTS: Pulmonary Artery Catheterization 
 The risks of central venous catheterization and PA insertion are many and serious, and the benefits should be identified before these procedures to justify their use.
The risks of central venous catheterization and PA insertion are many and serious, and the benefits should be identified before these procedures to justify their use.11 Describe the features of the right ventricle waveform
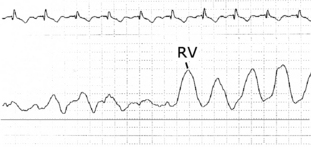
The right ventricle waveform has a rapid upstroke to peak systole, a rapid downstroke, and a small terminal rise at the end of diastole. The peak systolic pressure is found after the QRS complex but before the peak of the T wave. End diastole is found near the end of the QRS complex (Figure 26-1).
12 Describe the pulmonary artery waveform
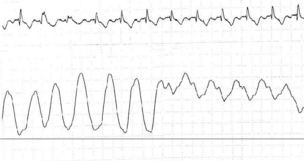
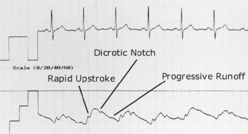
Perhaps the most noticeable change as the catheter tip enters the PA is the upstroke in diastolic pressure (Figure 26-2). Other features include a rapid upstroke, a progressive diastolic runoff, and a dicrotic notch secondary to pulmonic valve closure (Figure 26-3). Peak systole is found after the QRS complex but before the peak of the T wave. End diastole is found near the end of the QRS complex.
13 Review the pulmonary artery occlusion pressure waveform
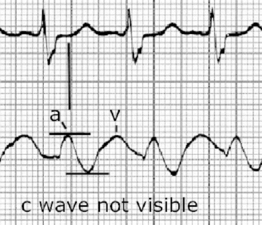
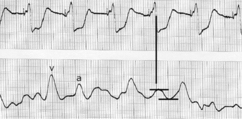
Like the CVP waveform, the PAOP has three positive waves (a, c, and v). Typically the a wave is most prominent, and the c wave is nonvisible. The a wave occurs with left atrial contraction, the c wave with mitral valve closure, and the v wave with left atrial filling. Note that the v wave occurs after the T wave of the electrocardiogram (ECG). The a wave is averaged to determine the PAOP (Figure 26-4).
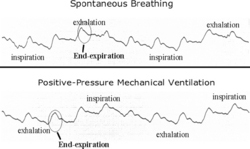
14 Contrast spontaneous breathing and positive-pressure mechanical ventilation and their effect on pulmonary artery occlusion pressure waveforms
The measurement desired is a transmural pressure (i.e., the difference between the chamber undergoing measurement and pleural pressure). As pleural pressures are not measured in clinical practice, the next best thing is to measure the pressure when intrathoracic pressure is least. Intrathoracic pressures are least at end-expiration while breathing spontaneously (Figure 26-5). PEEP and active expiration confound interpretation of the PAOP.
15 Pulmonary artery catheter pressures are surrogate measures for what important physiologic variables? What assumptions are made about the variables obtained through pulmonary artery catheterization?
Numerous assumptions are made to try to estimate the most important information, left ventricular end-diastolic volume (LVEDV). First, we are using pressures to estimate volume. Second, although we can measure pulmonary artery systolic, diastolic, and occlusion pressures, we are using these measures to estimate left atrial pressure (LAP) and left ventricular end-diastolic pressure (LVEDP). PA diastolic pressure in the healthy heart is a reliable estimate of PAOP, LAP, and LVEDP. However, clearly these relationships fall apart in the presence of cardiac and lung disease. LVEDP is dependent not only on volume but also on ventricular compliance, which can be decreased by ischemia, ventricular hypertrophy and dilation, septal shifts, aortic stenosis, pericardial effusions, use of inotropic agents, and hypertension; in these situations LAP poorly estimates LVEDP. In this instance estimating LVEDP by measuring the a wave of the PAOP is best. LAP may be higher than LVEDP in the presence of mitral regurgitation, as evidenced by a large v wave on the PAOP waveform (Figure 26-6). Increased pulmonary vascular resistance, present in chronic obstructive pulmonary disease, pulmonary embolic disease, acute respiratory failure, hypoxia, and hypercarbia, also decreases the correlation between PA diastolic and occlusion pressures.
16 In the presence of a large pulmonary artery occlusion pressure v wave, how should pulmonary artery occlusion pressure be estimated?
The best way to estimate PAOP is to average the a wave (Figure 26-7).
17 How might catheter position within the lung lead to errors in interpreting left atrial pressure catheter data?
The zones of West, as described in Chapter 2, describe the pressure relationship between pulmonary arterial, pulmonary venous, and alveolar pressure in different anatomic areas of the lung. The zones can change as a patient’s position and intravascular volume status changes. Mechanical ventilation and PEEP also change the zones. Usually a PA catheter will float into zone 3 and in fact must do so to accurately reflect left atrial pressure because only in zone 3 is there a constant fluid column between the pulmonary artery and left atrium. However, it should be noted that, once the catheter is inserted, the patient’s volume and ventilatory status may change remarkably, and the catheter tip may no longer be in a suitable position for correct interpretation (the catheter didn’t wander—the patient’s physiology wandered!).
1. Magder S. Invasive intravascular hemodynamic monitoring: technical issues. Crit Care Clin. 2007;23:401-414.
2. Polanco P.M., Pinsky M.R. Practical issues of hemodynamic monitoring at the bedside. Surg Clin North Am. 2006;86:1431-1456.
3. Sandham J.D., Hull R.D., Brant R.F., et al. A randomized, controlled trial of the use of pulmonary artery catheters in high-risk surgical patients. N Engl J Med. 2003;348:5-14.