CASE 25 Retroperitoneal Bleed
Cardiac catheterization
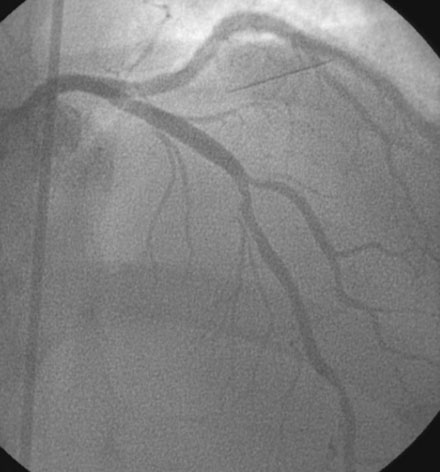
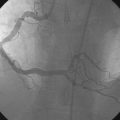
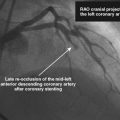
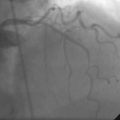
Angiography confirmed proximal occlusion of the left anterior descending artery (Figure 25-1). The operator successfully restored normal flow in this vessel with balloon angioplasty (2.5 mm diameter by 20 mm long balloon) followed by insertion of a 3.5 mm diameter by 15 mm long bare-metal stent (Figure 25-2). Adjunctive pharmacology included an additional bolus of unfractionated heparin and a bolus and infusion of eptifibatide. The left circumflex and right coronary arteries were angiographically normal. At the end of the procedure, 600 mg of clopidogrel was administered orally. The activated clotting time measured 260 seconds. An angiogram of the right femoral artery performed through the arterial sheath is shown in Figure 25-3 and Video 25-1. The operator successfully achieved access site hemostasis using a closure device (Starclose, Abbott Medical). The patient left the cardiac catheterization laboratory feeling well, with a blood pressure of 110/70 mmHg.
Postprocedural course
Upon arrival to the coronary care unit, he remained free of chest pain but became nauseated and reported right lower abdominal and scrotal pain. His heart rate fell to 51 beats per minute and his blood pressure dropped to 81/56 mmHg. He appeared pale and diaphoretic but denied chest pain. An electrocardiogram confirmed resolution of ST-segment elevation. Examination of the access site did not reveal any abnormalities; however, there was significant tenderness noted in the right lower quadrant, and scrotal swelling was observed. The operator again reviewed the femoral artery angiogram shown in Figure 25-3 and became concerned about the possibility of a retroperitoneal bleed. The infusion of eptifibatide was stopped and manual pressure was applied to the access site for 30 minutes. A bolus of 500 cc of normal saline and 1 mg of atropine restored the blood pressure and heart rate to normal. The hematocrit slowly fell from an immediate postcatheterization value of 36.0% to 27.1%, and increased to 34% after a two unit transfusion of packed red cells. Blood pressure, heart rate, and hematocrit remained stable and right lower abdominal discomfort improved. The right lower abdominal discomfort and scrotal swelling gradually resolved over the subsequent 3 days. He remained symptom-free and was discharged 4 days after admission.
Discussion
Few complications of percutaneous coronary intervention are as insidious as a retroperitoneal bleed. Retroperitoneal bleeds complicate about 0.5% to 0.7% of coronary interventions performed via the femoral artery.1–3 Although they are relatively rare, they are associated with a high incidence of serious adverse outcomes, including death in 10% to 12% of cases.2,3 Clearly, the most common cause of a retroperitoneal bleed is from inadvertent puncture of the artery above the inguinal ligament when obtaining femoral artery access. Rarely, a retroperitoneal bleed may be caused by spontaneous hemorrhage from anticoagulation, puncture of a vein, or from perforation of the iliac artery or aorta when advancing guide catheters or sheaths through tortuous vessels. Risk factors for development of retroperitoneal bleed have been well-studied and include female gender, high arterial puncture, chronic renal insufficiency, low body weight, and the use of glycoprotein IIb/IIIa inhibitors.1–3
In addition to the high mortality rate, retroperitoneal bleeding is associated with significant morbidity. Many adverse events are related to prolonged hypotension including renal failure, hepatic or acute lung injury, and multisystem failure. Blood transfusion is needed in 60% to 90% of patients.1,2 Stent thrombosis may arise from hypotension, as well as from abrupt reversal of anticoagulation and transfusion of blood products. Vascular surgical repair may be necessary in 5% to 15% of cases, usually for ongoing bleeding despite conservative measures or for the development of compressive neuropathy or uropathy.1–4
Although not entirely preventable, this dreaded complication can be minimized by using fluoroscopy to guide femoral artery access. Puncture should be directed no higher than the middle of the femoral head. Femoral artery angiography performed by injecting contrast through the side arm of the femoral sheath confirms the puncture site in most cases. The lower border of the loop created by the inferior epigastric artery defines the lower border of the retroperitoneal space (Figure 25-3); arterial access above this site may lead to a retroperitoneal bleed following sheath removal. Without a firm base formed by the bony mass of the femoral head, application of manual pressure cannot effectively compress the artery. Bleeding is directed internally and, reassured by the absence of bleeding from the incision site or development of a hematoma, the operator falsely assumes hemostasis has been achieved. The role of vascular closure devices in the development of this complication is controversial. Operators are urged to avoid them in the event of high puncture.
1 Farouque H.M.O., Tremmel J.A., Shabari F.R., Aggarwal M., Fearon W.F., Ng M.K.C., Rezaee M., Yeung A.C., Lee D.P. Risk factors for the development of retroperitoneal hematoma after percutaneous coronary intervention in the era of glycoprotein IIb/IIIa inhibitors and vascular closure devices. J Am Coll Cardiol. 2005;45:363-368.
2 Ellis S.G., Bhatt D., Kapadia S., Lee D., Yen M., Whitlow P.L. Correlates and outcomes of retroperitoneal hemorrhage complicating percutaneous coronary intervention. Catheter Cardiovasc Interv. 2006;67:541-545.
3 Tiroch K.A., Arora N., Matheny M.E., Liu C., Lee T.C., Resnic F.S. Risk predictors of retroperitoneal hemorrhage following percutaneous coronary intervention. Am J Cardiol. 2008;102:1473-1476.
4 Kent K.C., Moscucci M., Mansour K.A., DiMattia S., Gallagher S., Kuntz R., Skillman J.J. Retroperitoneal hematoma after cardiac catheterization: prevalence, risk factors and optimal management. J Vasc Surg. 1994;20:905-913.