Procedure 25 Flexor Pronator Slide
Indications
 A sustained functional impairment of the spastic upper extremity with a fixed forearm pronation, wrist flexion, and finger flexion deformity.
A sustained functional impairment of the spastic upper extremity with a fixed forearm pronation, wrist flexion, and finger flexion deformity.
 Some retained voluntary motor control of forearm supination, wrist extension, and finger extension must be present.
Some retained voluntary motor control of forearm supination, wrist extension, and finger extension must be present.
 This is more commonly recommended in an established Volkmann forearm contracture.
This is more commonly recommended in an established Volkmann forearm contracture.
Examination/Imaging
Clinical Examination
 Preoperative examination of the upper limb reveals a fixed contracture of the forearm in pronation with contracture of the wrist and fingers. Grasp and release motions of the hand are impaired owing to the fixed wrist position.
Preoperative examination of the upper limb reveals a fixed contracture of the forearm in pronation with contracture of the wrist and fingers. Grasp and release motions of the hand are impaired owing to the fixed wrist position.
 In a forearm Volkmann contracture, there is volar deep soft-tissue adhesions and fibrosis. There is often some retained finger and thumb flexion.
In a forearm Volkmann contracture, there is volar deep soft-tissue adhesions and fibrosis. There is often some retained finger and thumb flexion.
Surgical Anatomy
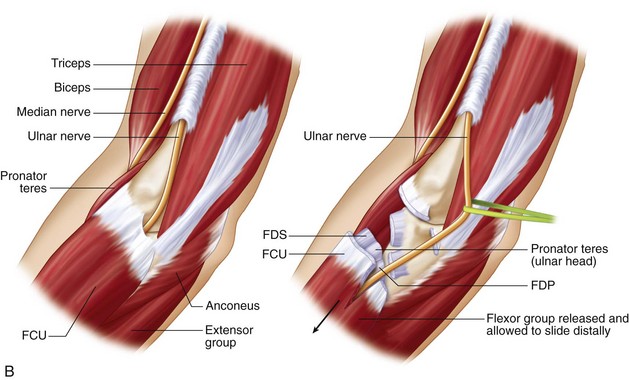
 Pertinent surgical structures include the volar forearm musculature, ulnar nerve, median nerve, brachial artery, and neurovascular structures adjacent to the interosseous membrane.
Pertinent surgical structures include the volar forearm musculature, ulnar nerve, median nerve, brachial artery, and neurovascular structures adjacent to the interosseous membrane.
 Unlike other contracture release procedures, the proximal anatomy is more relevant in this surgical procedure. The location of the median and ulnar nerves in the proximal forearm is vitally important.
Unlike other contracture release procedures, the proximal anatomy is more relevant in this surgical procedure. The location of the median and ulnar nerves in the proximal forearm is vitally important.
Exposures
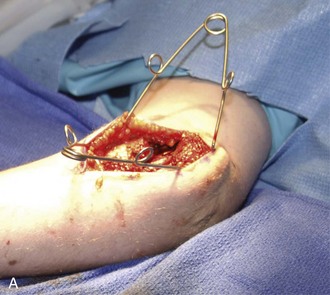
 An anteromedial, longitudinal incision at the elbow situated over the medial epicondyle (Fig. 25-1) is made.
An anteromedial, longitudinal incision at the elbow situated over the medial epicondyle (Fig. 25-1) is made.
 Superficial dissection includes identification and protection of the medial antebrachial cutaneous nerve. Wide subcutaneous flaps are necessary from the cubital tunnel region to the anterior forearm.
Superficial dissection includes identification and protection of the medial antebrachial cutaneous nerve. Wide subcutaneous flaps are necessary from the cubital tunnel region to the anterior forearm.
Pearls
It may be difficult to establish a plane between the flexor-pronator fascia and the subcutaneous tissue. There are multiple perforating vessels to the dermal layer that will require coagulation.
The dissection needs to extend to the median nerve as it enters between the deep and superficial heads of the pronator teres. This is similar to the exposure for a submuscular ulnar nerve transposition.
Procedure
Step 1
 The ulnar nerve is identified proximal to the medial epicondyle, and a decompression is performed through to the deep flexor carpi ulnaris muscle fibers.
The ulnar nerve is identified proximal to the medial epicondyle, and a decompression is performed through to the deep flexor carpi ulnaris muscle fibers.
 The anterior dissection involves a similar decompression of the median nerve as it enters the flexor musculature. The nerve needs to be completely free of adhesions to the flexor-pronator muscles such that the entire muscle group can slide distally after it is released.
The anterior dissection involves a similar decompression of the median nerve as it enters the flexor musculature. The nerve needs to be completely free of adhesions to the flexor-pronator muscles such that the entire muscle group can slide distally after it is released.
 A plane should be established between the posterior and anterior exposures. This plane is just anterior to the elbow capsule and the anterior band of the medial collateral ligament.
A plane should be established between the posterior and anterior exposures. This plane is just anterior to the elbow capsule and the anterior band of the medial collateral ligament.
 The entire flexor-pronator mass is then dissected from the medial epicondyle origin. It is elevated from the anterior elbow capsule and proximal portion of the intraosseous membrane (Fig. 25-2).
The entire flexor-pronator mass is then dissected from the medial epicondyle origin. It is elevated from the anterior elbow capsule and proximal portion of the intraosseous membrane (Fig. 25-2).
 The lateral border of the flexor digitorum superficialis, palmaris longus, and flexor carpi radialis is elevated from the intraosseous membrane. The median nerve has terminal motor branches in this region and requires careful dissection. The deep portion of the entire muscle group is then elevated.
The lateral border of the flexor digitorum superficialis, palmaris longus, and flexor carpi radialis is elevated from the intraosseous membrane. The median nerve has terminal motor branches in this region and requires careful dissection. The deep portion of the entire muscle group is then elevated.
 Dissection extends to the deep portion of the muscle origin.
Dissection extends to the deep portion of the muscle origin.
Step 1 Pearls
Identify the ulnar nerve proximally and release the cubital tunnel in a distal direction.
The deep dissection will permit identification of the medial collateral ligament. In cases of an elbow contracture, it may be difficult to separate the structure.
The flexor-pronator muscle group needs to be sufficiently mobilized from the elbow capsule and ligament such that the ulnar nerve can be transposed.
Step 2
 At the conclusion of the release, the entire flexor-pronator muscle origin will migrate distally (Fig. 25-3A and B).
At the conclusion of the release, the entire flexor-pronator muscle origin will migrate distally (Fig. 25-3A and B).
 This slide effectively translates the muscle origin distally to lengthen the muscles and allow greater supination, wrist extension, and finger extension (Fig. 25-4).
This slide effectively translates the muscle origin distally to lengthen the muscles and allow greater supination, wrist extension, and finger extension (Fig. 25-4).
 A submuscular transposition of the ulnar nerve is usually necessary. The ulnar nerve is placed adjacent to the median nerve in the anterior forearm.
A submuscular transposition of the ulnar nerve is usually necessary. The ulnar nerve is placed adjacent to the median nerve in the anterior forearm.
Postoperative Care and Expected Outcomes
 The forearm and hand are immobilized with long-arm dorsal and volar splints that hold the fingers and wrist in near full extension, with concomitant elbow extension and forearm supination.
The forearm and hand are immobilized with long-arm dorsal and volar splints that hold the fingers and wrist in near full extension, with concomitant elbow extension and forearm supination.
 After the swelling subsides, the splint can be changed into a cast.
After the swelling subsides, the splint can be changed into a cast.
 The immobilization is continued for 1 month and then advanced to a full-time splint that is forearm based to keep the wrist and fingers in extension. The splint is removed for hygiene purposes and for daily exercises.
The immobilization is continued for 1 month and then advanced to a full-time splint that is forearm based to keep the wrist and fingers in extension. The splint is removed for hygiene purposes and for daily exercises.
 There is gradual transition of the splint to a night-time splint over the next several months.
There is gradual transition of the splint to a night-time splint over the next several months.
 Unrestricted activities usually resume 3 to 4 months postoperatively, although in more chronic cases, a splint is worn during rest periods for several additional months.
Unrestricted activities usually resume 3 to 4 months postoperatively, although in more chronic cases, a splint is worn during rest periods for several additional months.