CHAPTER 25 Central Venous Catheterization and Pressure Monitoring
1 Define central venous catheterization
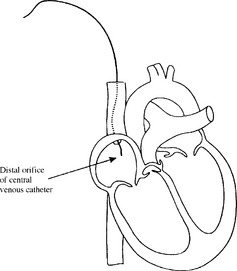
Central venous catheterization involves inserting a catheter into the venous circulation and advancing it so its distal orifice is positioned immediately adjacent to or within the right atrium of the heart (Figure 25-1).
6 Describe the internal jugular vein approach
 Low anterior: Locate the point at which the sternal and clavicular heads of the sternocleidomastoid muscle join. Introduce the needle at this point and direct it at a 30-degree angle to the skin. Advance the needle toward the ipsilateral nipple until venous blood is aspirated.
Low anterior: Locate the point at which the sternal and clavicular heads of the sternocleidomastoid muscle join. Introduce the needle at this point and direct it at a 30-degree angle to the skin. Advance the needle toward the ipsilateral nipple until venous blood is aspirated. High anterior: Palpate the carotid artery at the level of the cricothyroid membrane. Introduce the needle just lateral to the carotid pulsation and advance it toward the ipsilateral nipple at a 30-degree angle until venous blood is aspirated. This approach frequently requires penetration of the sternocleidomastoid muscle by the introducer needle.
High anterior: Palpate the carotid artery at the level of the cricothyroid membrane. Introduce the needle just lateral to the carotid pulsation and advance it toward the ipsilateral nipple at a 30-degree angle until venous blood is aspirated. This approach frequently requires penetration of the sternocleidomastoid muscle by the introducer needle. Posterior: Locate the junction of the posterior border of the sternocleidomastoid muscle and the external jugular vein. Introduce the needle just posterior to this point and advance it along the deep surface of the muscle toward the ipsilateral corner of the sternal notch until venous blood is aspirated.
Posterior: Locate the junction of the posterior border of the sternocleidomastoid muscle and the external jugular vein. Introduce the needle just posterior to this point and advance it along the deep surface of the muscle toward the ipsilateral corner of the sternal notch until venous blood is aspirated.11 In attempting a central venous puncture, dark blood returns. Does this satisfy you that you are indeed within a vein?
13 At what point on the body should central venous pressure be measured?
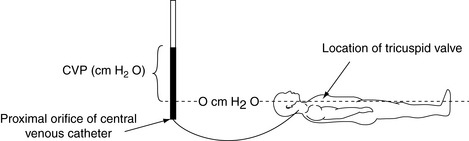
An external landmark for the tricuspid is a point 2 inches behind the sternum, roughly the anterior axillary line, at the fourth intercostal space. Ongoing adjustment is necessary to ensure that the transducer or manometer is consistently at this level whenever the patient’s position or bed height is changed (Figure 25-2).
15 How can you judge the correct positioning of the distal orifice of the catheter?
 Before insertion, measure the distance from the point of insertion to the right atrium (external landmark—immediately to the right of the third costal cartilage), giving a rough estimate of the length of inserted catheter necessary.
Before insertion, measure the distance from the point of insertion to the right atrium (external landmark—immediately to the right of the third costal cartilage), giving a rough estimate of the length of inserted catheter necessary. Advancing the catheter under fluoroscopy is the most accurate method for positioning the catheter tip but is time consuming and cumbersome.
Advancing the catheter under fluoroscopy is the most accurate method for positioning the catheter tip but is time consuming and cumbersome. With a specialized central venous catheter, the tip can be used as an electrocardiogram (ECG) electrode. After insertion the catheter is filled with electrolyte solution (normal saline or 8.4% NaHCO3), and the V lead of the ECG is attached to a proximal connection. The catheter is advanced toward the right atrium. The P-wave axis and voltage on the V lead tracing indicates the catheter tip position. As the catheter tip passes the area of the sinoatrial node, the P wave becomes equal in height to the R wave of the ECG. The catheter tip passing the mid-atrial position is demonstrated by a decreasing or biphasic P wave. Low atrial positioning is indicated by an inverted P wave or absence of the P wave.
With a specialized central venous catheter, the tip can be used as an electrocardiogram (ECG) electrode. After insertion the catheter is filled with electrolyte solution (normal saline or 8.4% NaHCO3), and the V lead of the ECG is attached to a proximal connection. The catheter is advanced toward the right atrium. The P-wave axis and voltage on the V lead tracing indicates the catheter tip position. As the catheter tip passes the area of the sinoatrial node, the P wave becomes equal in height to the R wave of the ECG. The catheter tip passing the mid-atrial position is demonstrated by a decreasing or biphasic P wave. Low atrial positioning is indicated by an inverted P wave or absence of the P wave.16 Describe the normal central venous pressure waveform and relate its pattern to the cardiac cycle
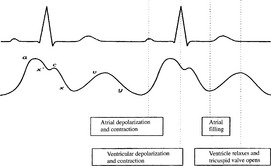
The normal CVP waveform shows a pattern of three upstrokes and two descents that correspond to certain events in the cardiac cycle (Figure 25-3).
 Before total relaxation is completed, the c wave occurs, which is caused by the bulging of the tricuspid valve into the atrium during the early phases of right ventricular contraction.
Before total relaxation is completed, the c wave occurs, which is caused by the bulging of the tricuspid valve into the atrium during the early phases of right ventricular contraction. The x descent follows the c wave and is a continuation of the x′ descent. The x descent is caused by a drop in pressure brought about by a downward movement of the ventricle and tricuspid valve during the later stages of ventricular contraction.
The x descent follows the c wave and is a continuation of the x′ descent. The x descent is caused by a drop in pressure brought about by a downward movement of the ventricle and tricuspid valve during the later stages of ventricular contraction. The v wave represents the increase in atrial pressure that occurs while the atrium fills against a closed tricuspid valve.
The v wave represents the increase in atrial pressure that occurs while the atrium fills against a closed tricuspid valve.19 How does central venous pressure relate to right ventricular preload?
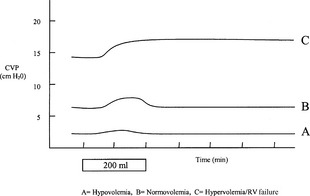
Despite the previous findings, it is widely held that CVP measurement is useful to the clinician as a guide to intravenous fluid replacement, especially at the upper and lower range of CVP. Thus a low (0 to 2 mm Hg) or decreasing CVP may indicate a need for fluid administration, whereas an increasing or elevated CVP (above 12 mm Hg) may indicate overresuscitation or a patient with impaired cardiac performance. The response of CVP to a fluid bolus has also been shown to be useful in assessing fluid status. In Figure 25-4 it can be seen that a 200-ml fluid bolus in the hypovolemic patient will result in a small but transient increase in CVP, whereas the same bolus in the normovolemic patient will result in a larger but still transient increase. However, in the hypervolemic patient with right ventricular failure, the same bolus results in a sustained increase in CVP. The CVP is best used to monitor a trend; an isolated determination is of limited value.
KEY POINTS: Central Venous Catheterization and Pressure Monitoring 
22 Are there noninvasive alternatives to central venous pressure that better indicate volume status?
23 How can an abnormal central venous pressure waveform be used to diagnose abnormal cardiac events?
25 Describe complications associated with placement of the central venous catheter
 Considering the proximity of the carotid artery to the internal jugular vein, it is not surprising that carotid artery puncture is one of the more common complications associated with all internal jugular vein approaches.
Considering the proximity of the carotid artery to the internal jugular vein, it is not surprising that carotid artery puncture is one of the more common complications associated with all internal jugular vein approaches. Pneumothorax may occur and is more commonly associated with a subclavian, low anterior (internal jugular), or junctional approach (junction of the internal jugular vein and subclavian vein).
Pneumothorax may occur and is more commonly associated with a subclavian, low anterior (internal jugular), or junctional approach (junction of the internal jugular vein and subclavian vein). Hemothorax is associated primarily with the subclavian vein approach and occurs secondary to subclavian artery puncture or laceration.
Hemothorax is associated primarily with the subclavian vein approach and occurs secondary to subclavian artery puncture or laceration. The thoracic duct, as it wraps around the left internal jugular vein, can reach as high as 3 or 4 cm above the sternal end of the clavicle. This places the duct in a vulnerable position for puncture or laceration when a left internal jugular venipuncture is attempted.
The thoracic duct, as it wraps around the left internal jugular vein, can reach as high as 3 or 4 cm above the sternal end of the clavicle. This places the duct in a vulnerable position for puncture or laceration when a left internal jugular venipuncture is attempted. Shearing and embolization of a catheter tip may occur when a catheter is withdrawn through a needle. Likewise a Seldinger guidewire can be sheared and embolized if attempts are made to withdraw it through an introducer needle. Therefore, if a catheter or wire cannot be advanced through an introducer needle, remove the parts in unison.
Shearing and embolization of a catheter tip may occur when a catheter is withdrawn through a needle. Likewise a Seldinger guidewire can be sheared and embolized if attempts are made to withdraw it through an introducer needle. Therefore, if a catheter or wire cannot be advanced through an introducer needle, remove the parts in unison.1. Deflandre E., Bonhomme V., Hans P. Delta down compared with delta pulse pressure as an indicator of volaemia during intracranial surgery. Br J Anaesth. 2008;100:245-250.
2. Domino K.B., Bowdle T.A., Posner K.L., et al. Injuries and liability related to central vascular catheters: a closed claims analysis. Anesthesiology. 2004;100:1411-1418.
3. Gelman S. Venous function and central venous pressure. Anesthesiology. 2008;108:735-748.
4. Taylor R.W., Palagiri A.V. Central venous catheterization. Crit Care Med. 2007;35:1390-1396.