Vitamins and Minerals
Objectives
1. Identify the actions and indications for vitamins and minerals.
2. List at least six products used to treat vitamin or mineral deficiencies.
3. Present a teaching plan for patients who require vitamin or mineral supplements.
Key Terms
ascorbic acid (ăs-KŎR-bĭk, p. 430)
minerals (MĬN-ĕr-ălz, p. 432)
niacin (NĪ-ă-sĭn, p. 427)
riboflavin (RĪ-bō-flā-vĭn, p. 427)
thiamine (THĪ-ă-mĭn, p. 426)
vitamin A (VĪ-tă-mĭn, p. 426)
vitamins (VĪ-tă-minz, p. 425)
Overview
![]() http://evolve.elsevier.com/Edmunds/LPN/
http://evolve.elsevier.com/Edmunds/LPN/
This chapter discusses the uses of vitamins and minerals. An overview of their actions, indications for use, and common adverse effects and drug interactions is presented. Vitamins are taken by people to maintain health and also by those who use medications to correct nutritional deficiencies. There may be drug interactions between vitamins and medications that affect both nutrient and drug absorption. Brief comments of importance for the nurse are included. Summaries of a sample of vitamin and mineral supplements available on the market are included in tables at the end of each major discussion. These over-the-counter (OTC) products change quickly, and the latest information should always be obtained for specific products. See Chapter 15 for additional related information about fluid and electrolyte products.
Vitamins
Overview
Vitamins are chemical compounds found naturally in plant and animal tissues but most are not made in the human body. Some are available in their active form; others come from food as a “precursor” or “provitamin” that then is converted to the active form. Two vitamins, Vitamin K and biotin, are not from food at all but are synthesized by bacteria inside the intestinal tract. They are necessary for life and essential to normal metabolism. They can act as coenzymes to regulate the creation of compounds in the body. Vitamins are classified into two types. Fat soluble vitamins are found primarily in various plant and animal oils or fats and can be stored in the body so daily intake is not essential. These vitamins are transported through the body by the bloodstream and remain dissolved because of unique-carrier proteins. Deficiencies are slow to develop. Water soluble vitamins are readily excreted in the urine and not stored in the body. The vitamins are destroyed by heat and deficiencies are quickly seen in patients. Usually patients get enough vitamins from a well-balanced, nutritious diet, except when certain conditions prevent them from eating food (such as intravenous therapy when a patient is taking nothing by mouth) or when the vitamins are not absorbed or their action is blocked (as in disorders that block fat metabolism) or the metabolism is accelerated (with some types of thyroid disease or pregnancy). Such conditions may require a vitamin supplement until a normal diet can be resumed or the underlying problem corrected.
Although controversy exists over natural versus synthetic vitamin preparations, current research confirms that vitamins are still vitamins, and the least expensive vitamin preparation is most likely as good therapeutically as a more expensive version. There are still many mysteries about the action of various vitamins in the body, but research has consistently demonstrated that taking large amounts of vitamins is unnecessary, may be harmful, and should be avoided.
There is a lot of literature about antioxidant vitamins and nutritional supplements. The major antioxidants are vitamin E (alpha-tocopherol), beta-carotene (a precursor, or forerunner, to vitamin A), vitamin C (ascorbic acid), and the mineral selenium. All of these are found in fruits and vegetables. Many research studies are looking at the mechanism of action of antioxidants. Current research suggests that when low-density lipoprotein (LDL) cholesterol is oxidized, sometimes incomplete oxidation takes place, producing free radicals that lead to atherosclerotic plaques. (An analogy has been made to wood that burns incompletely in a fireplace and “pops,” sending sparks against the screen.) It is thought that antioxidants retard or prevent LDL oxidation because they are oxidized in preference to LDL. This slows or eliminates the progression of atherosclerosis. It is also believed that antioxidants may slow the process that may cause cancer in cells. This has resulted in a large market for antioxidants to reduce the risk of cardiovascular disease and cancer.
Although many major research studies have looked at antioxidants after the fact and have suggested major benefits from increased use for many disease states, there are at present no intervention studies that support the role of antioxidants in cancer prevention. Epidemiologic evidence does indicate that those who eat fruits and vegetables regularly have a lower risk of cancer, although there is no conclusive evidence that this is the result of antioxidants. Therefore supplementation with vitamin antioxidants may be beneficial; however, in certain populations, such as smokers, research has found that it may actually be harmful. Nonetheless, the U.S. Department of Agriculture and the U.S. Department of Health and Human Services released new food guidelines in early 2011 based on what should be on a plate rather than the food pyramid. Today there is more emphasis than ever on eating fruits, vegetables, and whole-grain products, and on taking in fewer calories and getting more exercise to reverse widespread obesity in all age groups.
Vitamin A
Action And Uses
Vitamin A is a fat-soluble, long-chain alcohol that comes in several isometric forms: retinol, retinene, carotene, and retinoic acid. Its best understood action is helping the eye adjust to changes from light to darkness. Less understood actions include: (1) helping to stabilize and maintain the cell membrane structure, especially epithelial cell membranes, thereby helping the body resist infection; (2) affecting the synthesis of protein, which affects growth of skeletal and soft tissue; and (3) playing an essential role in reproduction.
Vitamin A supplementation is used to treat deficiency that may be provoked by sprue, colitis, regional enteritis, biliary tract or pancreatic disease, or partial gastrectomy. It is also used for the treatment of specific eye diseases and night blindness.
Adverse Reactions
If vitamin A is given in high doses for a long time, the treatment should be stopped at times to avoid hypervitaminosis. Any patient receiving 25,000 International Units or more should be closely supervised. Pregnant women should not receive more than 6000 International Units daily, or they may risk fetal abnormalities.
Drug Interactions
Women taking oral contraceptives often show elevated plasma vitamin A levels and should be closely monitored for hypervitaminosis. Mineral oil interferes with the absorption of fat-soluble vitamins. Certain antihyperlipidemic agents may also affect absorption of this product.
 Nursing Implications and Patient Teaching
Nursing Implications and Patient Teaching
One International Unit of vitamin A is equivalent to 0.6 mcg of beta-carotene or 0.3 mcg of retinol. This medication may be given orally, intravenously, or intramuscularly, depending on the rapidity of needed replacement.
Recommended daily allowances (RDAs) are as follows:
Children 0 to 9 years: 300 to 450 mcg/day
Children 9 to 18 years: 575 to 750 mcg/day
Adults 18 to 75 years and older: 750 mcg/day
Some foods rich in vitamin A are animal products such as dairy products; eggs; and organ meats (all contain preformed vitamin A); and deep orange, yellow, and green fruits and vegetables (these contain carotene). In addition, some fortified sources of vitamin A are infant formula, skim milk, margarine, and some cereals.
Vitamin B1 (Thiamine)
Action And Uses
Vitamin B1, or thiamine, is water soluble and functions as a coenzyme that is closely involved with carbohydrate metabolism. Thiamine is involved in 24 different reactions, including the citric acid cycle. It also has been thought to have a role in neurophysiologic function. Thiamine is excreted in the urine.
Vitamin B1 is used to treat beriberi, which is rare but not unknown in the United States. Vitamin B deficiency is usually found in patients with alcoholism, gastric lesions, or hyperemesis of pregnancy. Symptoms include anorexia (lack of appetite), vomiting, fatigability, aching muscles, ataxia (poor coordination) of gait, and emotional disturbances such as moodiness, depression, or excess alcohol use.
Adverse Reactions
Adverse reactions to thiamine include sensitivity (allergy) reactions, particularly after parenteral administration, which can be severe, including anaphylaxis (shock). Fatalities may occur. Sensitivity tests should be done before the therapeutic dose is given. Intravenous (IV) doses should be given very slowly. Feelings of warmth, pruritus (itching), urticaria (hives), nausea, angioneurotic edema (abnormal collection of fluid in deep layers of skin, often with lip swelling and hives), pulmonary edema, sweating, tightness of the throat, malaise (weakness), and cyanosis (blue color to the skin) are also seen.
Drug Interactions
Products that have neutral or alkaline solutions will produce poor stability of thiamine preparations.
 Nursing Implications and Patient Teaching
Nursing Implications and Patient Teaching
Thiamine is easily leached (lost) out of food and is destroyed when food is heated to more than 100° C, fried in hot pans, or cooked for a long time under pressure. There is some loss of thiamine during dehydration of vegetables. Thiamine is also sensitive to ultraviolet light. Foods rich in thiamine include pork, whole grains, enriched breads, cereals, and legumes. Satisfactory sources include green vegetables, fish, meats, fruits, and milk.
Vitamin B2 (Riboflavin)
Action And Uses
Vitamin B2, or riboflavin, is water soluble and acts as a precursor of two essential enzymes that deal with metabolism of proteins, fats, and carbohydrates. It is related to the release of energy to the cells and is active in tissue respiratory systems. It is used for the prophylaxis or treatment of riboflavin deficiency with symptoms which include soreness and burning of the tongue, lips, and mouth; discomfort in eating and swallowing; and photophobia (sensitivity to light), lacrimation (excess tear production), burning and itching of the eyes, visual fatigue, and the loss of visual acuity.
Drug Interactions
Riboflavin is only slightly soluble in water. Riboflavin levels in the body can be decreased by oral contraceptives, even in low doses. This loss has been shown through studies to be greater when patients have been taking oral contraceptives for at least 3 years.
 Nursing Implications and Patient Teaching
Nursing Implications and Patient Teaching
B2 or riboflavin supplements should be protected from light by keeping it in a tightly closed, light-resistant container. The medication turns urine a yellow color. Food sources naturally rich in riboflavin include milk; eggs; liver; kidney; heart; green, leafy vegetables; and enriched breads and cereals.
Niacin
Action And Uses
Niacin, previously called vitamin B3, is water soluble and an essential part of two coenzymes involved with intracellular respiration. These coenzymes convert lactic acid to pyruvic acid and function in energy release and in amino acid metabolism.
Niacin is used to prevent or treat deficiency states caused by a limited dietary intake of niacin, excessive dietary intake of leucine (which increases the daily need for niacin), general anorexia related to disease or other problems, or malabsorption syndrome. The deficiency state known as pellagra is rare but may be more prevalent in geographic regions where corn is the major staple food. Pellagra is usually found along with other vitamin deficiencies.
Pellagra symptoms are seen as changes in mucous membranes, skin, the gastrointestinal (GI) tract, and the central nervous system (CNS). Anorexia, irritability, anxiety, and mental changes such as hallucinations, lassitude (weariness), apprehension, and depression may be noticed.
GI symptoms include glossitis (swollen, beefy, red tongue), stomatitis (inflammation of the mouth), and diarrhea. Dermatitis of different body parts exposed to sun or trauma may develop, as well as lesions on the skin that result from sun, fire, or heat. Mental changes that are mild early in deficiency may progress to disorientation, loss of memory, confusion, hysteria, and, sometimes, manic outbursts.
Adverse Reactions
Adverse reactions to niacin include dry skin, pruritus, skin rash, GI disorders, allergies, feelings of warmth, headache, tingling of the skin, and transient flushing (red color in the face and neck).
Drug Interactions
Sympathetic blocking agents (antihypertensives) may increase the vasodilatory effect of niacin, leading to postural hypotension (low blood pressure when a person suddenly stands up).
 Nursing Implications and Patient Teaching
Nursing Implications and Patient Teaching
Flushing is a frequent side effect of niacin. If patients feel weak or dizzy, they should lie down until they feel better. Usually this reaction does not require stopping the drug. The usual dose is 8 mg/1000 kcal for infants and 6.6 mg/1000 kcal for children and adolescents. Less than 8 mg/day should not be given. The recommended intake for adults is 13 mg/day for women and 18 mg/day for men.
Foods rich in niacin are lean meats, peanuts, yeast, and cereal (especially bran and wheat germ). Other good sources include eggs, liver, red meat, whole grains, and enriched bread.
Pantothenic Acid
Action And Uses
Pantothenic acid, previously known as vitamin B5, is essential for the synthesis of coenzyme A, which has a role in the release of energy in fats, proteins, and carbohydrates. This vitamin has been used to treat paralytic ileus after surgery, possibly acting to stimulate GI motility. Deficiency states are produced only in the laboratory.
 Nursing Implications and Patient Teaching
Nursing Implications and Patient Teaching
When food is cooked to more than the boiling point, considerable loss of pantothenic acid occurs. The loss is smaller when food is moderately cooked or baked.
This vitamin is available naturally in all plant and animal tissues. Much of the original vitamin content is lost from frozen meat in the liquid that drips off during thawing. Rich sources include yeast, liver, kidney, egg yolk, wheat bran, and fresh vegetables. Human milk contains 2.2 mg/L and cow’s milk contains 3.4 mg/L.
Vitamin B6
Action And Uses
Vitamin B6, or pyridoxine hydrochloride, is water soluble and functions as a coenzyme in the metabolism of protein, carbohydrates, and fat.
Pyridoxine is used to treat pyridoxine deficiency seen in patients with inborn errors of metabolism, such as vitamin B6 dependency; vitamin B6-responsive chronic anemia; and other rare vitamin problems.
Pyridoxine deficiency is most likely to develop in the older adult population and in women of childbearing age, especially those who are pregnant or breastfeeding. Women taking oral contraceptives, alcoholics, and those whose diets are of poor quality and quantity or are high in refined foods are also at risk.
Symptoms of deficiency include malaise, nervousness, irritability, and difficulty in walking. There may also be personality changes in adults, such as depression and a loss of sense of responsibility. High doses of pyridoxine may produce neurotoxicity—ataxia, numb feet, and clumsiness.
Adverse Reactions
Adverse effects are not commonly seen in patients taking pyridoxine. Pyridoxine dependency (a state of conditioned need) may develop in adults taking doses exceeding 200 mg/day for a month.
Drug Interactions
Oral contraceptives may induce pyridoxine deficiency. Concurrent use with levodopa will neutralize CNS effects. Pyridoxine may prevent chloramphenicol-induced optic neuritis. Some drugs interfere with vitamin activity enough to block action and produce symptoms of deficiency.
 Nursing Implications and Patient Teaching
Nursing Implications and Patient Teaching
Pyridoxine should be kept in a tightly sealed, light-resistant container. Good food sources of vitamin B6 include yeast, wheat, corn, egg yolk, liver, kidney, and muscle meats; limited amounts are available from milk and vegetables. It is also found in liver, whole-grain breads and cereals, and soybeans.
Appropriate food preparation is important in preserving this vitamin. Freezing of vegetables results in a 20% loss of pyridoxine, and the milling of wheat results in a 90% loss.
Folic Acid
Action And Uses
Folic acid (also known as vitamin B9) is required for normal erythropoiesis, or red blood cell formation, and nucleoprotein synthesis. It is metabolized in the liver, where it is changed to its more active form. Folic acid is used to treat anemias caused by folic acid deficiency; it is also used in alcoholism, hepatic disease, hemolytic anemia, infancy (especially for infants receiving artificial formulas), lactation, oral contraceptive use, and pregnancy. Folic acid supplements may be needed in low-birth-weight infants, infants nursed by mothers deficient in folic acid, or infants with infections or prolonged diarrhea.
Recent guidelines have emphasized the importance of increased folic acid intake by all women of childbearing age, especially in those women intending to get pregnant and in early pregnancy to help prevent spinal cord malformations in the fetus (neural tube defects). The folic acid additives in commercial bread and grain products have been increased in an attempt to provide more adequate supplies of this important vitamin.
Research has suggested that concentrations of the amino acid homocysteine increases in the body with age and low levels of folate and vitamins B6 and B12. High homocysteine levels may be involved in the development of occlusive vascular disease (atherosclerosis), which may increase the risk of myocardial infarction. Therefore the level of folate in persons younger than 65 years of age should be measured.
Adverse Reactions
Folic acid is not toxic. An allergic reaction may produce bronchospasm, erythema (redness or irritation), malaise, pruritus, and rash; large amounts may discolor the urine.
Drug Interactions
Chloramphenicol and methotrexate are folate antagonists, and they may cause decreased folic acid activity. Para-aminosalicylic acid and sulfasalazine may cause symptoms of folic acid deficiency. Use with many anticonvulsants may decrease the anticonvulsant effect, leading to increased seizure activity. Use of oral contraceptives may lead to folic acid deficiency.
 Nursing Implications and Patent Teaching
Nursing Implications and Patent Teaching
The RDAs of folic acid are as follows:
These RDAs are usually provided by an adequate diet.
Folic acid for parenteral use must be protected from light.
Proper nutrition is essential, and dietary measures are preferable to drug therapy. The patient should be counseled to eat foods high in folic acid to prevent a deficiency problem in the future.
Blood for hematologic laboratory tests should be drawn before beginning therapy. Drug therapy should improve the blood test results within 2 to 5 days.
Patient education should include the importance of remaining under medical supervision while receiving therapy. The patient may need to have the dose increased or decreased. Patients often fail to return for follow-up visits when they begin to feel better.
Diet is important in restoring proper folic acid levels and preventing deficiencies in the future. The patient should eat foods high in folate, including fresh, leafy green vegetables; other vegetables and fruits; yeast; and organ meats.
Vitamin B12
Action And Uses
Vitamin B12 is water soluble and contains cobalt. It is produced by the bacterium Streptomyces griseus. It functions in many metabolic processes in protein, fat, and carbohydrate metabolism. The coenzymes of B12 are also part of the erythrocyte-maturing factor of the liver and are required in the synthesis of deoxyribonucleic acid (DNA). Vitamin B12 has a hemopoietic activity identical to the antianemia factor of the liver, and it is essential for growth, cell reproduction, and nucleoprotein and myelin synthesis. Intrinsic factor must be present in the stomach and small intestine to absorb B12. Vitamin B12 interacts with folate in metabolic functions, and a deficiency in B12 makes folate useless in the body.
Vitamin B12 is used to treat all B12 deficiency conditions, including pernicious anemia (with or without neurologic symptoms), certain other anemias, malabsorption syndromes, hemorrhage, blind loop syndrome, chronic liver disease complicated by deficiency of vitamin B12, malignancy, and pregnancy and thyrotoxicosis (in which deficiency is seen because of increased metabolic rate), and renal disorders. Vitamin B12 is also used as the flushing dose in Schilling test (a specific test used for pernicious anemia). Symptoms of deficiency are rare, occurring mainly in people on strict vegetarian diets, because although vitamin B12 is water soluble, it is found only in animal products. Symptoms include dyspepsia, sore tongue, breathlessness, and a characteristic stiff back, often dubbed a “poker” or “vegan” back. Most patients with Vitamin B12 deficiency have a malabsorption problem in the GI tract, and the vitamin replacement is injected which bypasses the GI tract. Parenteral, nasal, or oral therapy may be used to maintain normal B12 levels.
Nascobal is a vitamin B12 nasal spray used as a maintenance drug for persons in remission after undergoing intramuscular (IM) therapy for pernicious anemia. The dose is usually 500 mcg intranasally once weekly. If the patient develops adverse effects such as infection, headache, glossitis, nausea, and rhinitis after taking the nasal spray, it is often necessary to start IM vitamin B12 again.
Adverse Reactions
Allergy to vitamin B12 is rare. The patient may report pruritus, a feeling of swelling of the entire body, or a severe anaphylactic reaction. A few patients may experience mild pain, localized skin irritation, or mild transient diarrhea after an injection of cyanocobalamin.
Drug Interactions
Alcohol, colchicine, and para-aminosalicylic acid lower the absorption of vitamin B12. Some antibiotics lower the response to vitamin B12 therapy.
 Nursing Implications and Patient Teaching
Nursing Implications and Patient Teaching
Irreparable neurologic damage may occur if a deficiency state continues longer than 3 months or when treatment for pernicious anemia includes only folic acid. If colchicine, para-aminosalicylic acid, or excessive alcohol intake occurs for more than 2 weeks, malabsorption of vitamin B12 may occur.
The recommended daily intake of cyanocobalamin for adults is 3 mcg. The best food sources of B12 include organ meats; bivalves such as clams and oysters; nonfat dry milk; fermented cheese such as Camembert and Limburger; and seafood such as lobster, scallops, flounder, haddock, swordfish, and tuna.
Vitamin C
Action And Uses
Vitamin C, or ascorbic acid, has multiple functions, some of which are understood better than others. Vitamin C functions in a number of enzyme systems and is involved in intracellular oxidation-reduction potentials. It aids in the change of folic acid and the metabolism of certain amino acids, assists the absorption of iron and calcium, and blocks the absorption of copper in the GI tract. Ascorbic acid protects vitamins A and E and polyunsaturated fatty acids. It is also necessary for the formation of the ground substance of bones, teeth, connective tissue, and capillaries and for the synthesis of collagen. Ascorbic acid aids in wound healing and may be involved in blood clotting.
Ascorbic acid is used to treat debilitated (weak) patients, especially after surgery in older adult patients with fractures, and as a supplement for burn victims or patients undergoing severe stress. Infection, smoking, chronic illness, and febrile states may increase the need for vitamin C. It is used along with iron therapy and in patients on prolonged IV therapy. Premature infants require relatively large doses. It is also used for the prophylaxis and treatment of scurvy, the deficiency state.
With modern refrigeration and processing methods of citrus fruits, scurvy is rarely seen in the United States, but it may be found when other vitamin deficiencies are present. Symptoms include tender, painful muscles, joints, and bones; muscle cramps; anorexia; fatigue; malaise; and sore gums. Wound healing is impaired, and hemorrhagic manifestations are demonstrated by subperiosteal bleeding and petechial hemorrhages. Vasomotor instability, bruising, faulty bone and tooth development, loosened teeth, and gingivitis also may develop.
Adverse Reactions
The patient may experience mild, brief soreness at injection sites if the medication is given intramuscularly or subcutaneously. Patients may also experience brief episodes of faintness or dizziness when IV injections are given too rapidly. Excessive doses are usually rapidly excreted into the urine. Doses in excess of 1 to 3 g daily may result in GI complaints, glycosuria, oxaluria, and development of renal stones, especially in patients prone to these problems. Patients who chronically overuse vitamins may develop dependency.
Drug Interactions
Ascorbic acid may have varying effects on anticoagulants, blocking the action of some and prolonging the intensity and duration of others. Ascorbic acid increases the effect of salicylates through increased renal tubular reabsorption. There is also an increased chance of crystallization of sulfonamides in the urine when ascorbic acid is given at the same time. Ascorbic acid decreases the effect of tricyclic antidepressants by decreasing renal tubular reabsorption. Calcium ascorbate may cause cardiac dysrhythmias (irregular heartbeats) in patients receiving digitalis. Ascorbic acid is chemically incompatible with potassium penicillin G and should not be mixed in the same syringe. Smoking may lead to an increased need for vitamin C by decreasing ascorbic acid serum levels. Intermittent use of ascorbic acid in patients taking ethinyl estradiol may increase the risk of contraceptive failure. Large doses of vitamin C may interfere with urine testing in some diabetic testing methods.
 Nursing Implications and Patient Teaching
Nursing Implications and Patient Teaching
Vitamin C comes in three major forms that may be given orally or parenterally: ascorbic acid, sodium ascorbate, and calcium ascorbate. The recommended daily intake is 60 mg for adults.
Vitamin C is easily destroyed by air, heat, and light. This medication should be kept tightly capped in its own container. Foods high in vitamin C should not be boiled for long periods or left uncovered in the refrigerator.
Good food sources of vitamin C include oranges; grapefruit; strawberries; cauliflower; cantaloupe; beef liver; asparagus; green, leafy vegetables; and potatoes.
Vitamin D
Action And Uses
“Vitamin D” is a label used for a group of fat-soluble, chemically similar sterols. The three main categories within this group are:
3. Other lesser compounds (vitamins D4, D5, D6, and D7), which are formed by irradiation of sterols.
Therefore the term vitamin D has become rather ambiguous.
The main action of this group of sterols is the movement of calcium and phosphorus ions into three main sites: the small intestine (to promote absorption of calcium and phosphorus from the gut), the kidneys (to cause phosphate reabsorption in the proximal convoluted tubules and, to a lesser extent, to stimulate calcium and sodium reabsorption), and bone (to help increase the mineralization of newly formed bone). Vitamin D3 has been shown to inhibit the spread of fibroblasts and keratinocytes in the skin and to promote epidermal keratinocyte differentiation. It is used in the treatment of some skin disorders.
Vitamin D preparations are used to treat childhood rickets and adult osteomalacia, hypoparathyroidism, and familial hypophosphatemia. In childhood, rickets may be diagnosed by complaints of excessive sweating and GI disturbances. These may be the first symptoms, appearing before any objective findings. In adult cases of osteomalacia, patients may complain of skeletal pain and progressive muscular weakness.
Adverse Reactions
Symptoms of vitamin D toxicity include anorexia, nausea, malaise, weight loss, vague aches and stiffness, constipation, diarrhea, convulsions, anemia, mild acidosis, and impairment of renal function. The renal effects are usually reversible. A variety of more serious systemic effects may be seen in adults. Dwarfism may be present in infants and children. Most toxic effects persist for several months in adults at doses of 100,000 International Units or more daily or in children at doses of 20,000 International Units or more daily. Reactions gradually disappear if treatment is discontinued at the first sign of symptoms.
Drug Interactions
Mineral oil and some of the antihyperlipidemic agents may interfere with the absorption of fat-soluble vitamins. Thiazide diuretics and vitamin D together contribute to hypercalcemia. There is a possible connection between phenytoin (Dilantin) and phenobarbital use leading to hypocalcemia, which, in turn, may contribute to rickets or osteomalacia.
 Nursing Implications and Patient Teaching
Nursing Implications and Patient Teaching
The dosage of vitamin D must be planned for each patient and given under close supervision, because the range between the therapeutic and the toxic levels is narrow. Calcium intake should be enough to give a serum calcium level between 9 and 10 mg/dL. In rickets, 12,000 to 500,000 International Units/day can be taken. In hypoparathyroidism, the initial dose is typically 50,000 to 200,000 International Units/day, with a maintenance dosage of 50,000 to 400,000 International Units/day. Most people obtain all the vitamin D they need from the food in their diets. Natural sources of vitamin D are few, so the majority of vitamin D is obtained from fortified sources. Fortified foods high in this vitamin are milk, evaporated milk, infant formula, and powdered skim milk. Cereals, margarine, and diet foods also contain vitamin D supplements. Breast milk is usually already Vitamin D rich. Vitamin D should be protected from light in a light-resistant container.
Vitamin E
Action And Uses
Vitamin E is fat soluble and consists of naturally occurring tocopherols. Vitamin E is considered an essential nutrient for humans, even though its specific functions are not yet understood. Vitamin E may function as an antioxidant to prevent damage to cell membranes. It stabilizes red-blood-cell walls and protects them from hemolysis or destruction. It may also increase vitamin A use and stop platelet aggregation.
Many suggested uses of vitamin E are controversial and unproved. The only established use is to prevent or treat vitamin E deficiency. Vitamin E has been touted as a powerful antioxidant. New evidence suggests that vitamin E supplements do not reduce the risk of cancer or major cardiovascular disease and may even increase the risk of heart failure. High intake of vitamin E from food as tocopherol may be inversely related to Alzheimer disease. Vitamin E in supplements is usually present as alpha-tocopherol and is less helpful in decreasing risk of Alzheimers.
Adverse Reactions And Drug Interactions
Vitamin E appears to be the least toxic of the fat-soluble vitamins. No signs and symptoms of toxicity or hypervitaminosis have been identified as yet in humans. However, results of a 2004 metaanalysis of research studies suggests that doses over 150 International Units/day increase the risk of all-cause mortality. The higher the dose taken, the higher the mortality rate. The most common marketed dose in the United States is 400 International Units. Many individuals take up to 2000 International Units/day.
 Nursing Implications and Patient Teaching
Nursing Implications and Patient Teaching
Food sources of vitamin E are primarily from plants. The highest amounts are found in vegetable oils such as soybean and corn and in nuts; wheat germ; rice germ; and green, leafy vegetables. Meat and dairy products provide less. An accurate assessment of tocopherol levels in food is difficult to obtain. The amount in the body depends on the initial concentration of vitamin E and the processing, storage, and preparation of the food. Vitamin E products should be stored in tightly closed, light-resistant containers.
Vitamin K
Action And Uses
Vitamin K helps hepatic formation of active prothrombin (factor II), proconvertin (factor VII), plasma thromboplastin component (factor IX), and the Stuart factor (factor X), which are essential for normal blood clotting. The exact mechanism is unknown. Menadione (K3) and phytonadione (K1) are synthetic lipid-soluble forms of vitamin K. Menadiol sodium diphosphate (K4) is changed in the body to menadione. Menadione is not commonly available now.
Vitamin K is used to treat or prevent various blood clotting disorders that result in damaged formation of factors II, VII, IX, and X. The American Academy of Pediatrics recommends routine phytonadione (K1) injection at birth to prevent hemorrhagic disease of the newborn. Vitamin K does not counteract the anticoagulant activity of heparin, although it is helpful in reversing the effects of warfarin (Coumadin) overdosage.
Adverse Reactions
Specific adverse reactions to menadione (K3)/menadiol sodium diphosphate (K4) include headache, rash, urticaria, gastric upset, redness, and pain or swelling at injection site. Specific adverse reactions to phytonadione (K1) include brief hypotension (low blood pressure), rapid and weak pulse, dizziness, flushing, sweating, unusual taste sensations, redness, and pain or swelling at injection site. Severe reactions, including fatalities, have occurred with the use of IV phytonadione, even when caution is used (dilution of drug, slow infusion).
Drug Interactions
Concurrent use of vitamin K with oral anticoagulants may decrease the effects of the anticoagulant. Mineral oil and cholestyramine inhibit GI absorption of oral vitamin K.
 Nursing Implications and Patient Teaching
Nursing Implications and Patient Teaching
The preferred routes of administration of vitamin K are subcutaneous or IM. IV administration is not recommended because of the risk of anaphylaxis. Naturally occurring vitamin K is found in liver and green, leafy vegetables.
A summary of selected vitamin preparations on the market is presented in Table 24-1.
Table 24-1
| GENERIC NAME | TRADE NAME | COMMENTS AND DOSAGE |
| vitamin A | Aquasol A | Adults: Give 50,000-100,000 International Units/day for 3 days to 2 wk, followed by 10,000-20,000 International Units/day for 2 mo. |
| vitamin B1 | — | Medications may be given PO, IM, or IV. Daily average dose is 0.5 mg/1000 kcal intake, or usually 1-1.4 mg/day PO. Usual dosage is 50 mg IM for deficiency states, 5-10 mg PO. |
| vitamin B2 (riboflavin) | Infants: Give 0.3-0.4 mg/day. Children: Give 0.5-0.9 mg/day. Adult Men: Give 1.3-1.6 mg/day. Adult Women: Give 1-1.1 mg/day. For deficiency states, usually 50 mg IM and 5-10 mg daily as dietary supplement for adults and children older than 12. |
|
| niacin (vitamin B3) niacinamide (nicotinamide) |
Niacor | May be given IM, subcutaneously, or IV; IV route with slow drip preferred when parenteral medication is necessary. Deficiency states: Give 50-100 mg daily. Pellagra: Give up to 500 mg/day. Adults: Give 500 mg PO daily, or 100-200 mg 1 to 5 times daily. |
| pantothenic acid (vitamin B5) |
Pantothenic 250 | NOTE: A RECOMMENDED DAILY ALLOWANCE IS NOT ESTABLISHED. FOR SUPPLEMENTATION GIVE: Infants (0-1 yr): 1.7-1.8 mg/day PO. Children (1-13 yr): 2-4 mg/day PO. Adults and adolescents 14 yr or older: 5 mg/day PO. Adult or adolescent lactating and pregnant women: 6-7 mg/day PO. |
| vitamin B6 (pyridoxine) | Neuro-K | Recommended daily allowances range from 2 to 2.2 mg. Preparation may be given PO, IM, or IV. Dietary deficiency: Give 10-20 mg/day for 3 wk, then 2-5 mg/day for several weeks. Vitamin B6 dependency states: up to 600 mg/day initially, dropping to 50 mg/day for life. |
| folic acid and derivatives (vitamin B9) | Folvite | Dietary supplement: 100 mcg (0.1 mg)/day (up to 1 mg/day in pregnancy); may be increased to 500 mcg (0.5 mg) to 1 mg daily or more if underlying condition causes increased requirements (for example, in tropical sprue, 3-15 mg daily may be needed). Treatment of deficiency: 250 mcg (0.25 mg) initially to 1 mg daily PO, IM, IV, or deep subcutaneous until hematologic response occurs; maintenance 400 mcg-1 mg/day. |
| vitamin B12 (cyanocobalamin) | Crystamine | Nutritional deficiency: Give 100-250 mcg/day PO. Vitamin B12 deficiency: PO: Give 1000 mcg/day. |
| IM, subcutaneously: Give 15 mcg/day. If patients have normal GI absorption, give along with other multiple vitamins. In other cases, give 30 mcg daily for 5-10 days, and then 100-200 mcg monthly for life. |
||
| Nascobal | Intranasal spray: Give 500 mcg once weekly. | |
| vitamin C (ascorbic acid) | Cevi-Bid Cecon |
Adults: Give 60 mg/day. |
| vitamin D | Calcifediol | Adults: Give 20-50 mcg/day or 100-200 mcg every other day. |
| Calcijex | Adults: Give 300-350 mcg/wk administered daily or every other day. | |
| D-Tabs | Initial: Give 0.25 mcg/day, increased by 0.25 mcg/day at 2- to 4-wk intervals until satisfactory response obtained. Some patients may respond to doses of 0.25 mcg every other day. Patients undergoing hemodialysis may require doses of 0.5 to 1 mcg/day. Initial: Give 0.75-2.5 mg daily for several days. |
|
| DHT | Maintenance: Give 0.2-1 mg daily, titrated by serum calcium levels. Average dose 0.6 mg. | |
| ergocalciferol | Vitamin D–resistant rickets: Give 50,000-500,000 | |
| Calciferol drops | International Units daily. Hypoparathyroidism: Give 50,000-400,000 International Units of vitamin D daily. |
|
| vitamin E | Aquavit-E | A range of 10-20 International Units of vitamin E should provide adequate levels. |
| vitamin K | AquaMEPHYTON | Anticoagulant-induced prothrombin deficiency: 2.5-10 mg or up to 25 mg initially. Frequency and dosage of subsequent therapy determined by prothrombin time response. |
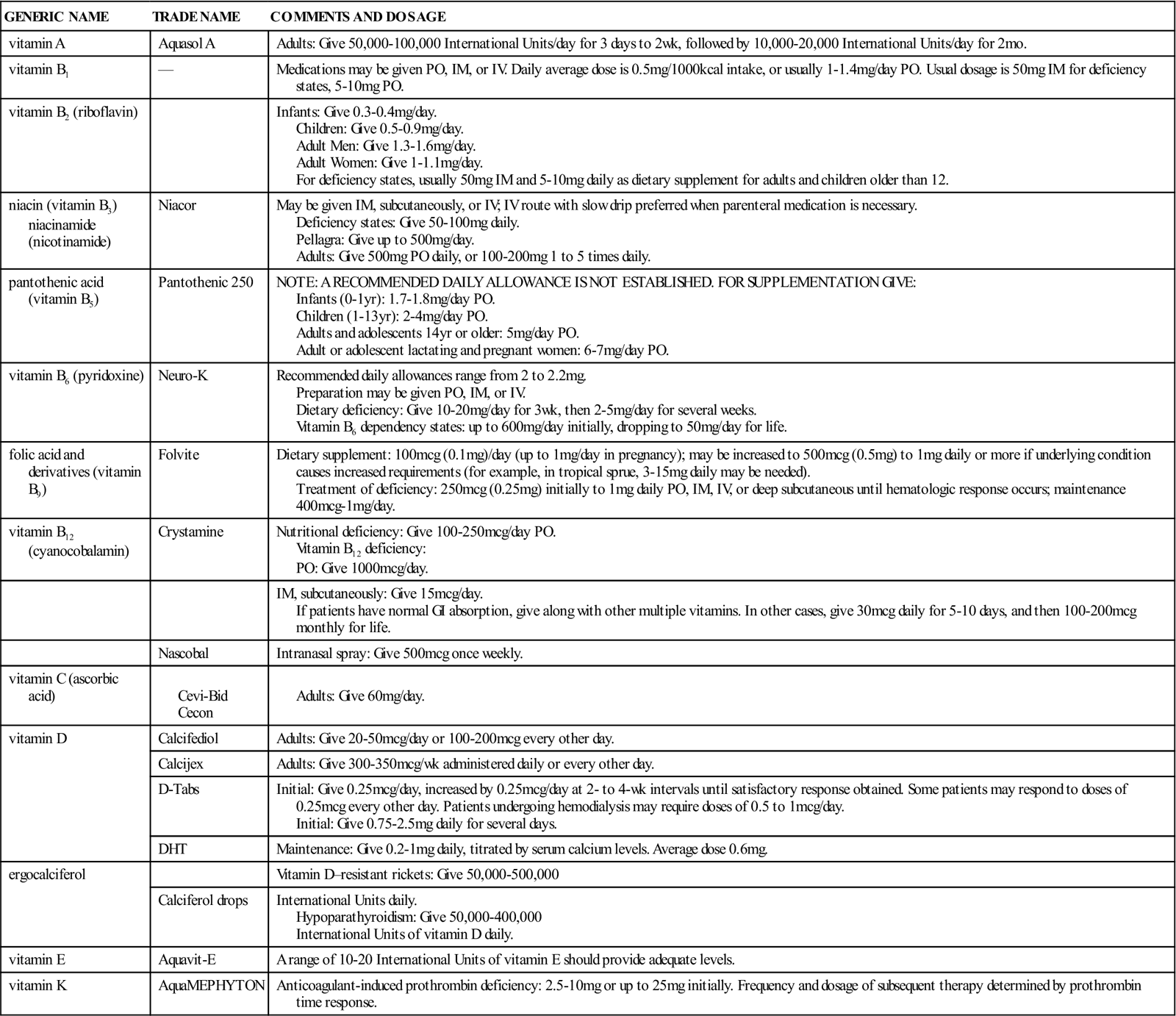
GI, gastrointestinal; IM, Intramuscular; IV, intravenous; PO, by mouth.
Minerals
Overview
There are 19 inorganic substances called minerals present in the body, at least 13 of which are essential to normal metabolism and function. These minerals are present as ions with positive and negative charges, leading to the formation of salts. They act as catalysts to speed up various biochemical reactions. Minerals are obtained from a diet that includes a variety of animal and vegetable products and meets the energy and protein needs of the body. The Food and Nutrition Board of the National Research Council has established recommended daily intakes for calcium and iron. Calcium, iron, and iodine are the three elements most frequently missing in the diet. Zinc, iron, copper, magnesium, and potassium are the five minerals most frequently involved in disturbances of metabolism. As electrolytes, these preparations are commonly infused to critically ill patients unable to take food orally.
Calcium
Action And Uses
Calcium is a major mineral in the body and is essential for muscular and neurologic activity, especially in the cardiac system. Calcium functions in the formation and repair of skeletal tissues (bones and teeth); activates several enzymes that influence cell membrane permeability and muscle contraction; aids in blood clotting by stimulating the release of thromboplastin and the conversion of fibrinogen to fibrin; activates pancreatic lipase; influences the intestinal absorption of cobalamin; and, in extracellular fluids, is involved in the transmission of neurotransmitters and in metabolic processes. Calcium is also involved in the regulation of lymphocyte and phagocyte function through interaction with calmodulin.
Calcium is used as a supplement when dietary levels of calcium are not adequate. Calcium requirements may be increased during adolescence, pregnancy, breastfeeding, and for postmenopausal women. Calcium is also used to treat neonatal hypocalcemia and to prevent and treat postmenopausal and senile osteoporosis. It may also be used as a supplement to parenterally administered vitamin D in cases of hypoparathyroidism, pseudohypoparathyroidism, rickets, and osteomalacia.
Adverse Reactions
Watch for symptoms of hypercalcemia, such as polyuria (excretion of a large amount of urine), constipation, abdominal pain, dryness of mouth, anorexia, nausea, and vomiting.
Drug Interactions
Vitamin D is essential for the absorption of calcium in the body. Calcium status is affected by the calcium-to-phosphorus ratio in the body and by the level of protein in the diet. Phytic acid (found in bran and whole-grain cereals) and oxalic acid (found in spinach and rhubarb) may interfere with calcium absorption by combining with calcium to form insoluble salts in the intestine. Calcium compounds and calcium-rich substances such as milk interfere with the absorption of oral tetracycline, so their use together should be avoided. Use of corticosteroids may also decrease the absorption of calcium.
 Nursing Implications and Patient Teaching
Nursing Implications and Patient Teaching
In patients with low calcium levels, carpal spasm may be elicited by compressing the upper arm with a blood pressure cuff, causing ischemia (decreased blood supply) to the distal nerves. The patient may report a tingling sensation and may inadvertently flex the arm. Excessive amounts of calcium may lead to hypercalcemia and hypercalciuria, especially in hyperthyroid patients. Serum and renal calcium levels should be followed to detect the development of renal stones; calcium should not be given to patients who already have renal stones.
Calcium products come in combination with various other chemicals, with a concentration of between 6% and 40%. Preparations come in both parenteral and oral forms. OTC antacids containing calcium (i.e. Tums) are composed of calcium carbonate, the most elemental form of calcium. It is better absorbed than many calcium products and is a smaller tablet than many other calcium products, making administration easier.
The recommended daily intake of calcium is 1200 mg/day for adults and for adolescents, 800 mg/day for children, 360 to 540 mg/day for infants from birth to 1 year, and 1500 mg/day for nursing mothers. Milk and dairy products are the richest sources of calcium. Egg yolks and most dark green, leafy vegetables are also good sources.
Fluoride
Action And Uses
Fluoride is concentrated in bones and teeth and is present in soft tissues only in very small amounts. It is an essential trace element but has not been proven to be essential to life. Fluoride is taken into the surface enamel of teeth in higher concentrations than in deeper layers. This strengthening of the enamel provides greater resistance to damage by acids produced in dental plaque. Fluoride has therefore been found useful in reducing dental caries.
Fluoride is recommended for the prevention of dental caries in all age groups. It may be used topically or systemically. It is primarily administered in places without fluoride in the water supply or to individuals with a genetic tendency for dental caries.
Adverse Reactions
Gastric distress, headache, urticaria, and malaise may be seen in hypersensitive individuals. Excessive salivation, mottling of teeth, GI disturbances, and nausea are seen in acute overdosage.
Drug Interactions
Fluoride in the water supply may produce calcium fluoride, a poorly absorbed product, when taken with dairy foods.
 Nursing Implications and Patient Teaching
Nursing Implications and Patient Teaching
Fluoride is available in gels, pastes, drops, tablets, capsules, and mouth rinses. The preparation and quantity chosen should be adjusted to the fluoride level of the local water supply. The county water commissioner may be contacted for this information. Fluoride products should be taken as ordered. Tablets and drops may be dissolved in water used for making infant formula or added to food or juices. Tablets may also be swallowed, chewed, or allowed to dissolve slowly in the mouth. Products are best taken after meals. For rinses and gels, teeth should be brushed thoroughly, and then the coating should be applied to clean teeth. The fluoride coating should not be swallowed. The patient should not rinse the mouth, eat, or drink for 30 minutes after treatment. Plastic containers should be used for diluting fluoride drops or rinses, and glass should be avoided. Milk may decrease absorption of oral fluoride products, so the patient should avoid taking fluoride with milk or dairy products.
Iodine
Action And Uses
Iodine is a trace mineral found in most parts of the body. Its presence is essential to the normal function of the thyroid gland. Goiter is the classic symptom of iodine deficiency and can appear after several months of inadequate iodine. This deficiency is prevalent in the US and has an increasing rate in pregnant women where the deficiency can be dangerous to a forming fetus. Potassium iodine was once commonly administered to patients with excessive bronchiolar mucus production but this indication has fallen into disfavor. It is used as an antithyroid agent in the treatment of hyperthyroidism and thyrotoxicosis and preoperatively to induce the shrinking of the thyroid. It has also been used in some dermatologic conditions. Because certain brands of these products can provide protection against radioactive iodine exposure, they have been approved by the FDA for use in case of a nuclear plant accident or ‘dirty bomb’ containing 131 I exposure.
Adverse Reactions
Gastric distress is common and includes nausea/vomiting and diarrhea. Acneiform rash may develop from prolonged use and may be fatal. Iodine toxicity, or iodism, symptoms include metallic taste; sore gums, teeth, and mouth; burning in the throat or mouth; ulcerated mucous membranes; acute rhinitis; sneezing; and irritation of the eyes with swelling of the eyelids. Severe headache, productive cough, pulmonary edema, and tenderness and swelling of the parotid and submaxillary glands may also occur. Hypersensitivity reactions may also be seen with symptoms suggestive of serum sickness.
Drug Interactions
Potassium iodide should not be administered with the thyroid hormones due to their opposite effects. Potassium iodide should be given cautiously with any other drugs that contain potassium because of the problem of producing hyperkalemia.
 Nursing Implications and Patient Teaching
Nursing Implications and Patient Teaching
The RDAs of iodine are as follows:
Infants 0-6 months: 110 mcg/day
Infants 7-12 months: 130 mcg/day
Children 1-8 years: 90 mcg/day
In case of a nuclear reaction, the patient should stop taking any other medications or supplements that might interfere with the iodide uptake into thyroid tissue.
Iron
Action And Uses
Iron is an essential mineral for the synthesis of myoglobin and hemoglobin. It stimulates the hematopoietic system and increases hemoglobin to correct iron deficiency. Iron from cellular hemoglobin is recycled and most is used again. During pregnancy, the reabsorption of iron increases to 15% as the body’s way of adapting to physiologic anemia.
Iron is used to treat symptomatic iron deficiency anemia only after the cause of the anemia has been identified, and it is used to prevent hypochromic anemia during infancy, childhood, pregnancy, and breastfeeding; in patients recovering from other anemias; and after some GI surgeries.
Adverse Reactions
Adverse reactions to iron supplements include constipation, cramping, diarrhea, epigastric or abdominal pain, GI irritation, and allergic reactions to any component of the iron preparation. Symptoms of overdosage may occur after 30 minutes to several hours and include lethargy (sleepiness), nausea, vomiting, abdominal pain, diarrhea, melena (blood in stools), and dyspnea (uncomfortable breathing). Coma and metabolic acidosis may occur, as well as symptoms of systemic absorption. Children who mistake vitamins for candy are particularly sensitive to large amounts of iron and may die from overdoses.
Drug Interactions
Large iron doses may cause a false-positive test result for occult blood using the toluidine test (Hematest, Occultist, Clinistix). Absorption of oral iron is inhibited by tannic acid in tea, antacids (particularly magnesium trisilicate–containing antacids), milk, and eggs. Patients receiving chloramphenicol concurrently with iron may show a delayed response to iron therapy. Absorption of iron increases when given with ascorbic acid (Vitamin C) in doses of 200 mg per 30 mg of iron. Iron interferes with absorption of oral tetracycline. Vitamin E decreases the response to iron therapy. Many other medications may have interactions.
 Nursing Implications and Patient Teaching
Nursing Implications and Patient Teaching
The cause of the anemia must be identified and treated. Help collect stools for occult blood tests after the patient has been on a red meat–free diet for at least 3 days. Although dietary lack may contribute to iron deficiency, especially in those older than 75 years of age, blood loss is the primary cause. Heavy menstrual periods and multiple pregnancies may produce anemia in women. Hematologic laboratory values are often normally lower in older adults, leading to overprescribing of iron for geriatric patients. Liquid preparations can discolor teeth and should be taken through a straw after dilution with liquid.
Replacement of iron in iron deficiency anemia requires 90 to 300 mg of elemental iron daily in divided doses (6 mg/kg/day). Symptoms should go away within 2 weeks, and laboratory studies should be normal within 2 months, if diagnosis and treatment are adequate. Therapy for 4 to 6 months after the anemia has been corrected is advised to replenish iron stores. More iron is absorbed if the iron is taken on an empty stomach with water or in an acid environment, although taking it after meals can reduce stomach irritation. Taking iron after a meal can reduce the absorption by 40% to 50%. Different oral preparations vary in cost and percentage of elemental iron. Product selection must be based on how well it is absorbed, how well it is tolerated, and the individual needs of the patient. All simple oral iron preparations are available OTC. The absorption of iron taken orally or through dietary foods is generally about 10%. The body does have the capability to increase iron absorption during times of physiologic stress, such as pregnancy and severe blood loss.
The recommended daily intake of elemental iron in adult males is 10 mg; in adult women, 18 mg (with an additional 10 mg during pregnancy or lactation); and in children, 10 to 15 mg. A diet high in natural iron should be encouraged to meet these needs. Fish, red meat, spinach, and dried fruits are the best sources of dietary iron.
Iron supplements can cause dark green or black stools. The patient should report constipation, diarrhea, nausea, or abdominal pain to the health care provider.
Magnesium
Action And Uses
Magnesium is an electrolyte that is essential to several enzyme systems. It is important in maintaining osmotic pressure, ion balance, bone structure, muscular contraction, and nerve conduction. This mineral has been determined to be especially important in cardiac function, and only slight deficiencies may prolong the Q-T interval and lead to a very dangerous form of ventricular tachycardia (rapid heartbeat) called torsades de pointes.
Adverse Reactions
Excessive magnesium intake may produce diarrhea.
 Nursing Implications and Patient Teaching
Nursing Implications and Patient Teaching
Magnesium deficiencies are seen primarily when malabsorption syndromes are present. Magnesium is usually used with other vitamins as a general dietary supplement when multiple deficiencies are suspected. Deficiency states have been associated with convulsions, slowing of growth, digestive disturbances, spasticity of muscles and nerves, accelerated heartbeat, dysrhythmias, nervous conditions, and vasodilation (opening of blood vessels). Magnesium is available in adequate quantities in meat, milk, fruits, and vegetables, and special dietary planning is unnecessary.
Manganese
Action And Uses
Manganese activates many enzymes, assists in normal skeletal and connective tissue development, helps in the initiation of protein synthesis, and plays a part in the synthesis of cholesterol and fatty acids. It is found throughout all body tissues and fluids. No precise RDA has been established.
Manganese is used in dietary supplements. Usually it is used with other vitamins when multiple deficiencies are suspected. Research subjects with manganese deficiency experienced weight loss, changes in beard and hair growth (usually slowing of growth), and occasional nausea and vomiting. There are no known adverse effects or drug interactions.
Nuts, whole-wheat cereals, and grains are the foods richest in manganese. Tea and cloves are exceptionally rich. Meat, fish, and dairy products have low amounts of manganese.
Potassium
Action And Uses
Potassium is the principal intracellular cation of most body tissues, acting in the maintenance of normal renal function, contraction of muscle, and transmission of nerve impulses. It is found in the body within a very narrow range.
Potassium may be taken prophylactically (for prevention) when the patient has nephrotic syndrome, in hepatic cirrhosis with ascites, and in patients with hyperaldosteronism who have normal renal function. Potassium products are used prophylactically or to replace potassium that may be lost as a result of long-term diuretic therapy, digitalis intoxication, or low dietary intake of potassium. Supplementation may also be necessary for deficits resulting from vomiting and diarrhea, diabetic acidosis, metabolic alkalosis, corticosteroid therapy, or to counteract increased renal excretion of potassium because of acidosis, certain renal tubular disorders, or diseases that produce increased secretion of glucocorticoids or aldosterone.
Adverse Reactions
Either excess or deficit of potassium causes symptoms. Adverse reactions to potassium supplements include nausea, vomiting, diarrhea, abdominal discomfort, and GI bleeding. Potassium intoxication or hyperkalemia (increased potassium in the blood) may result from overdosage of potassium or from a change in the patient’s underlying condition, which may make potassium buildup possible. Signs and symptoms of potassium intoxication include flaccid paralysis, paresthesias (numbness and tingling) of the hands and feet, mental confusion, restlessness, listlessness, malaise, and heaviness of the legs. Hypotension and cardiac dysrhythmias leading to heart block may also develop. Potentially fatal dysrhythmias may develop if potassium cannot be excreted (or if it is administered too rapidly IV). When it is detected, hyperkalemia requires immediate treatment because lethal levels of potassium may be reached in a few hours in untreated patients. Potentially lethal dysrhythmias may also occur with hypokalemia (decreased potassium in the blood).
Drug Interactions
Potassium should not be used in patients receiving potassium-sparing agents such as aldosterone antagonists or triamterene, because overdosage may develop.
 Nursing Implications and Patient Teaching
Nursing Implications and Patient Teaching
All potassium supplements must be diluted properly or taken with plenty of liquid to avoid producing GI ulcers. The usual adult dietary intake of potassium ranges between 40 and 60 mEq/day. The loss of 200 or more mEq of potassium from the total body store is enough to produce hypokalemia.
The dosage must be titrated (increased or decreased slowly) based on the individual’s needs and the patient should be closely watched during therapy, especially in the initial stages of therapy. For patients receiving diuretic therapy, 20 mEq/day is usually adequate for the prevention of hypokalemia. In cases of potassium depletion, 40 to 100 mEq/day or more may be required for replacement. Blood levels must be monitored closely.
Potassium comes in various salt combinations; potassium chloride is the form most frequently prescribed. It may be ordered either by percentage of potassium chloride or in milliequivalents of potassium chloride, with 10 mEq KCl per 15 mL equivalent to 5% KCl. Other salt combinations are potassium gluconate, potassium citrate, potassium acetate, and potassium bicarbonate. Potassium is also available in combination with vitamin C, ammonium chloride, citric acid, betaine HCl, and L-lysine monohydrochloride.
Many health care providers tell patients to eat a potassium-rich diet in addition to taking a potassium supplement. A potassium-rich diet includes foods such as bananas, citrus fruits (especially tomatoes and oranges), apricots, and dried fruits such as raisins, prunes, and dates. Fresh cantaloupe and watermelon, nuts, dried beans, beef, and fowl also contain ample quantities of potassium.
Zinc
Action And Uses
Zinc is a part of many enzymes and is essential for normal growth and tissue repair. Zinc functions in the mineralization of bone and in the detoxification and oxidation of methanol and ethylene glycol. It plays a role in the creation of DNA and the synthesis of protein from amino acids. It is important in wound healing and functions in moving vitamin A from liver stores.
Zinc supplements are used to prevent zinc deficiency and to treat delayed wound healing. There is some evidence to support the use of zinc OTC products in reducing the severity of symptoms of the common cold.
Patients taking zinc may complain of abnormalities of taste and smell, rough skin, and anorexia with profound disinterest in food. Patients who lack zinc may demonstrate sexual immaturity, delayed wound healing, and decreased absorption of dietary folate.
Adverse Reactions
Adverse reactions to zinc supplements include gastric ulceration, nausea, and vomiting. Doses in excess of 2 g produce emesis (vomiting). Acute zinc intoxication produces drowsiness, lethargy, light-headedness, staggering gait, restlessness, and vomiting leading to dehydration.
Drug Interactions
Calcium competes with zinc for absorption. Phytates form insoluble complexes with zinc and interfere with its absorption. Zinc impairs the absorption of tetracycline derivatives.
 Nursing Implications and Patient Teaching
Nursing Implications and Patient Teaching
The RDAs for zinc are as follows:
Infant to 12 months: 3 to 5 mg/day
Children 1-10 years: 10 mg/day
Seafood and meats are rich sources of natural zinc; cereals and legumes also have significant amounts of this mineral.
Table 24-2 presents a summary of minerals discussed as supplements plus phosphorus and sodium chloride that are occasionally included with other mineral preparations.
Table 24-2
| GENERIC NAME | TRADE NAME | COMMENTS AND DOSAGE |
| Calcium | ||
| calcium acetate | PhosLo | Has 25% calcium. Adults: Give 1200-1800 mg daily. |
| calcium carbonate | Os-Cal 500 | Has 40% concentration of calcium, the largest of any calcium. |
| calcium citrate | Citracal | Has 21% calcium. Adults: Give 1200-1800 mg qd. |
| calcium glubionate | Calciquid | Oral preparation contains 6% calcium. Administer before meals to increase absorption. Adults: (including pregnant and breastfeeding women) and children 4 yr or older: Give 15 mL 3 times daily. |
| calcium gluconate | Calcium Gluconate | Comes in both oral and parenteral forms. IV infusion preferred over IM injection; used frequently in emergency situations. Check equivalency of all oral products, because they vary from preparation to preparation. In parenteral forms, 10 mL contains 90 mg (4.5 mEq) calcium. |
| calcium lactate | Calcium Lactate | Contains 13% calcium and is given orally. Available without prescription. |
| tricalcium phosphate | Posture | Has 39% calcium. Adults: Give 1200-1800 mg daily. |
| Fluoride | ||
| fluoride (oral) | Fluoritab | Adjust dosage according to local water fluoride level. General oral dosages is 1 g daily. |
| fluoride (topical) | Fluorigard Fluorinse Prevident |
Products used between professional dental fluoride treatments for patients who have excessive problems with tooth decay. After brushing, hold preparation in mouth for at least 1 min, then spit out. To obtain maximum benefit, do not swallow; do not eat, drink, smoke, or rinse mouth for at least 15-30 min after treatment to obtain maximum benefit. |
| Iodine | ||
| potassium iodide | PI | Most products are off the market. The government has stockpiles of PI which they distribute to communities that have nuclear reactors to keep on hand in the event of a nuclear disaster. |
| Saturated solution potassium iodide | SSKI | Oral drops given to help relieve bronchial mucus. Now only rarely ordered. |
| Iron | ||
| ferrous fumarate | Femiron | Few reported side effects with this product. Better tolerated than sulfate or gluconate. Contains 33% elemental iron. |
| ferrous gluconate | Fergon | Less corrosive than ferrous sulfate. Indicated for those who cannot tolerate sulfate because of gastric irritation. Contains 11.6% elemental iron. Adults: Give 320-640 mg PO 3 times daily. Children 6-12 yr: Give 100-300 mg PO 3 times daily. |
| ferrous sulfate | Feosol Fer-In-Sol |
Ferrous sulfate is the standard preparation against which all other iron salts are compared. Optimal compound because it is the least expensive and contains 20% elemental iron. Timed-release capsules are more expensive and less well absorbed but reportedly have fewer side effects. Liquid Feosol cannot be mixed with juice. |
| ferrous sulfate | FeroSul Feratab |
Product contains more elemental iron per milligram of compound than other products. More expensive than plain ferrous sulfate. |
| iron dextran | DexFerrum INFeD Infurfer |
Used when oral iron administration is impossible or unsatisfactory. Parenteral iron has caused fatal anaphylactic-type reactions and must be used with care. Test dose: Give 0.5 mL IV or IM 1 hr before the therapeutic dose (to rule out hypersensitivity). Calculate total dose required using the following formula: 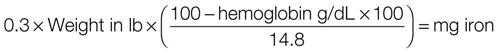 For patients weighing less than 30 lb, reduce to 80% total calculated. The Z-track method should be used for injection into the gluteus maximus muscle only. Inject deeply using a 2- or 3-inch 19- or 20-gauge needle. |
| Magnesium | ||
| magnesium gluconate | Magonate Magtrate |
RDA for adult men is 350 mg; adult women, 330 mg. As a dietary supplement: 27-133 mg daily to 3 times daily |
| Manganese | ||
| manganese sulfate | Mangimin | No RDA has been determined. Suggested daily intakes include 0.5-0.7 mg PO for infants, 2.5-5.0 mg PO for adolescents, and 3-7 mg PO for adults. |
| Potassium | ||
| potassium chloride liquid powder | Cena-K Kaon K-Lor K-Lyte |
Wide variation in concentration, price, flavor. Make certain medication is diluted with water or juice or is taken with adequate quantities of liquid. Titrate to individual requirements. Usual dosage is 20 mEq/day for prophylaxis and 40-100 mEq/day for treatment of potassium depletion. |
| Combinations of Potassium Gluconate, Potassium Citrate, Potassium Acetate, Potassium Bicarbonate | ||
| effervescent tablets | Effer-K K-Lyte |
These products, most of which require prescriptions, are used primarily in patients in whom chloride is restricted. Because some of these products do contain chloride, it is important to carefully choose the potassium salt desired. There is wide variability in the cost of these products, with most tending to be more expensive than potassium chloride products. Effervescent tablets must be dissolved completely in water before administration. Dosage should be titrated to individual needs. Usual dosage is 20 mEq/day for prophylaxis and 40-100 mEq/day for treatment of potassium depletion. |
| liquids | Cena-K Kaon Kaylixir |
|
| powders | Klorvess Kolyum |
|
| Zinc | ||
| zinc sulfate | Orazinc | Adults: Give 15 mg daily. |
| Phosphorus | ||
| phosphate (sodium, potassium) | Neutra-Phos | Adults: Give 800-1200 mg. May have mild laxative effect. |
| Sodium Chloride | ||
| sodium chloride | Slo-Salt | Provide supplementation on rare occasions. |
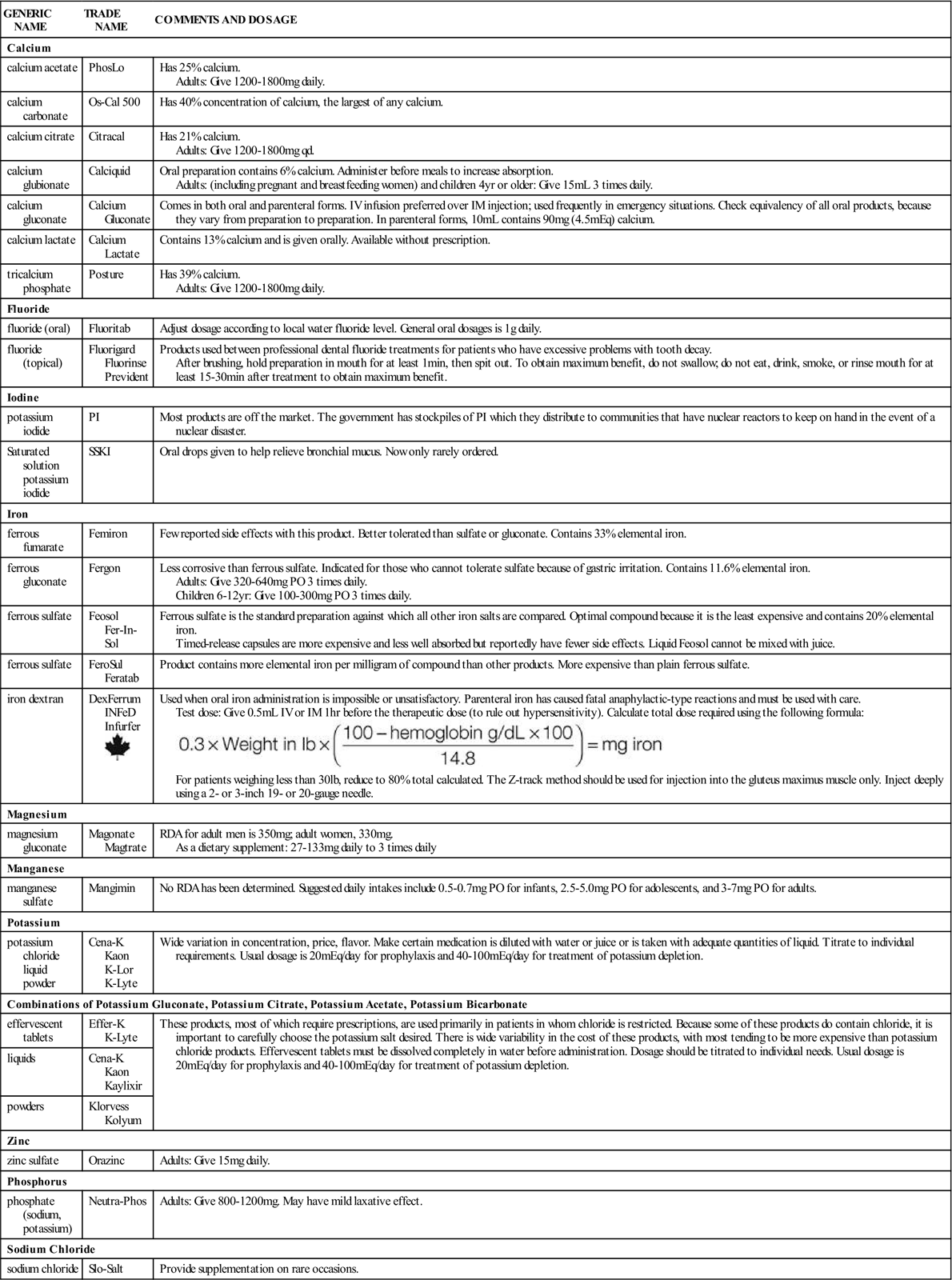
IM, Intramuscular; IV, intravenous; PO, by mouth; qd, every day; RDA, recommended daily allowance.
Vitamin And Mineral Deficiencies
Overview
In accepting that many people in the United States eat poorly, the American Medical Association has for the first time recommended the use of a daily multiple vitamin supplement if patients do not eat a well-balanced diet and eat lots of high-fat or “empty calorie” foods. Supplements or vitamins cannot make up for a poor diet or other unhealthful lifestyle practices such as smoking or lack of exercise. If patients cannot tolerate certain foods such as dairy products, they may need to supplement their diet to ensure they are getting the nutrients provided by that food group.
A deficiency of one vitamin in a diet that is otherwise adequate is rare. Deficiency signs and symptoms in a patient may point to a lack of one vitamin, but usually a deficiency of several vitamins will be found. Because of the vast number of multiple-vitamin preparations that are easily available to consumers, as well as television and magazine advertisements, hypervitaminosis (excess amounts of several vitamins) is more likely to occur than are deficiencies of single vitamins.
 Nursing Implications and Patient Teaching
Nursing Implications and Patient Teaching
n Assessment
Try to learn as much as possible about the patient’s health history, including the presence of hypersensitivity, pregnancy, breastfeeding, underlying systemic disease, hereditary disorders, and use of other medications that may cause drug interactions. The patient should be assessed for symptoms of multiple deficiency or disease states.
n Diagnosis
In addition to the medical problems resulting in the need for vitamin or mineral products, does the patient have financial, cultural, or nutritional problems or attitudes that contribute to the problem? Does the patient have a lack of knowledge about how to prepare, store, or use water- or fat-soluble vitamins? Does the patient do things that would interfere with getting vitamins from the food normally eaten? Does the patient try to make up for poor diet by taking vitamins or nutritional supplements?
n Planning
Many vitamin and mineral supplementation regimens require baseline laboratory assessment before starting therapy so that progress may be monitored.
Make certain the medication or supplement is stored properly and protected from light and heat to avoid destruction of the essential nutrient.
n Implementation
Confirm the route of administration for the medication before the product is given. Many products must be given very slowly or only by certain routes.
n Evaluation
Watch for the therapeutic effect or to see if the patient has adverse effects. The nurse may need to help arrange for the patient to get follow-up laboratory studies to measure improvement.
n Patient and Family Teaching
Tell the patient and family the following:

