Procedure 24 Superficialis-to-Profundus Tendon Transfer
Indications
 This procedure is indicated for fixed finger deformities secondary to flexor digitorum superficialis and flexor digitorum profundus tendon spasticity. The muscle properties have been permanently altered owing to the contracture severity and chronicity.
This procedure is indicated for fixed finger deformities secondary to flexor digitorum superficialis and flexor digitorum profundus tendon spasticity. The muscle properties have been permanently altered owing to the contracture severity and chronicity.
 These patients have marked functional impairment and have expected limited upper extremity use. The procedure is often used for facilitating skin care and hand hygiene problems.
These patients have marked functional impairment and have expected limited upper extremity use. The procedure is often used for facilitating skin care and hand hygiene problems.
 The determination between this type of transfer and a fractional lengthening needs to be evaluated by preoperative assessment. Comanagement with the family and caregivers is essential for identifying the preoperative needs.
The determination between this type of transfer and a fractional lengthening needs to be evaluated by preoperative assessment. Comanagement with the family and caregivers is essential for identifying the preoperative needs.
 It should be explained that finger stiffness is common after surgery and that a different type of contracture may be present. The position of the contracture is changed to a posture that aids in maintaining hygiene and overall care.
It should be explained that finger stiffness is common after surgery and that a different type of contracture may be present. The position of the contracture is changed to a posture that aids in maintaining hygiene and overall care.
Examination/Imaging
Clinical Examination
 Preoperative evaluation is important to determine the contribution of the different volar flexor muscles to the finger contracture. Examine finger extension at both maximum wrist flexion and maximum wrist extension.
Preoperative evaluation is important to determine the contribution of the different volar flexor muscles to the finger contracture. Examine finger extension at both maximum wrist flexion and maximum wrist extension.
 The finger flexion deformity will be worse with maximum wrist extension than with maximum wrist flexion if the deformity is secondary to contracture of the flexor digitorum superficialis and flexor digitorum profundus tendons. In different neurologic conditions, the wrist flexor musculature may also be spastic.
The finger flexion deformity will be worse with maximum wrist extension than with maximum wrist flexion if the deformity is secondary to contracture of the flexor digitorum superficialis and flexor digitorum profundus tendons. In different neurologic conditions, the wrist flexor musculature may also be spastic.
 Assess the metacarpophalangeal, proximal interphalangeal, and distal interphalangeal joints of each digit because fixed contractures may require concomitant treatment (closed manipulation, open capsulotomies, or joint fusions).
Assess the metacarpophalangeal, proximal interphalangeal, and distal interphalangeal joints of each digit because fixed contractures may require concomitant treatment (closed manipulation, open capsulotomies, or joint fusions).
Surgical Anatomy
 Pertinent surgical structures include all volar forearm muscles (palmaris longus, flexor carpi radialis [FCR], flexor carpi ulnaris [FCU], flexor digitorum superficialis [FDS], flexor digitorum profundus [FDP], pronator teres, pronator quadratus), median nerve, ulnar nerve and artery, and radial artery.
Pertinent surgical structures include all volar forearm muscles (palmaris longus, flexor carpi radialis [FCR], flexor carpi ulnaris [FCU], flexor digitorum superficialis [FDS], flexor digitorum profundus [FDP], pronator teres, pronator quadratus), median nerve, ulnar nerve and artery, and radial artery.
Positioning
 The patient is positioned supine with the arm extended onto a surgical arm board.
The patient is positioned supine with the arm extended onto a surgical arm board.
 A nonsterile tourniquet is placed high on the arm to permit better manipulation of the elbow during the procedure. If an elbow procedure is also necessary, a sterile tourniquet is used. Visualization of the volar forearm can be difficult if there is elbow flexion and forearm pronation contracture. In these instances, sterile bumps are necessary under the dorsal forearm. General anesthesia with muscle relaxation is also helpful to overcome the deforming force of the pronator teres.
A nonsterile tourniquet is placed high on the arm to permit better manipulation of the elbow during the procedure. If an elbow procedure is also necessary, a sterile tourniquet is used. Visualization of the volar forearm can be difficult if there is elbow flexion and forearm pronation contracture. In these instances, sterile bumps are necessary under the dorsal forearm. General anesthesia with muscle relaxation is also helpful to overcome the deforming force of the pronator teres.
Exposures
 A longitudinal volar forearm approach from the mid-forearm to the proximal wrist crease is used.
A longitudinal volar forearm approach from the mid-forearm to the proximal wrist crease is used.
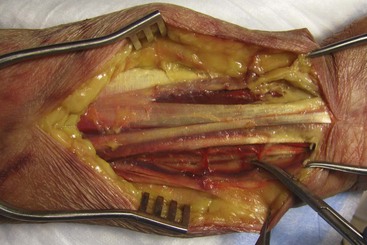
 The FDS and FDP need to be visualized from the level of the musculotendinous junction to the level of the entrance into the carpal tunnel. The incision should be extended as necessary to identify the flexor tendons and median nerve (Fig. 24-1).
The FDS and FDP need to be visualized from the level of the musculotendinous junction to the level of the entrance into the carpal tunnel. The incision should be extended as necessary to identify the flexor tendons and median nerve (Fig. 24-1).
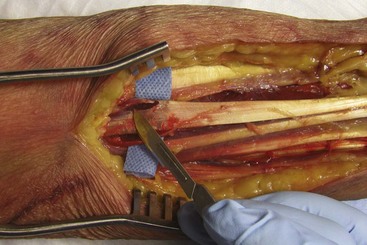
 Meticulous hemostasis is necessary with ligation of the small perforating vessels (Fig. 24-2).
Meticulous hemostasis is necessary with ligation of the small perforating vessels (Fig. 24-2).
Procedure
Step 1
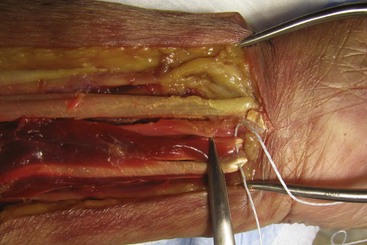
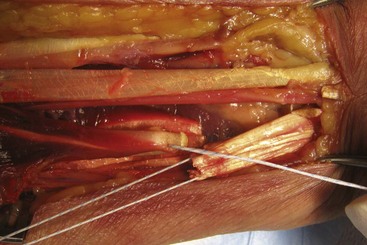
 The palmaris longus is identified, and a tenotomy is performed proximally within the incision. Identify the FDS and FDP tendons, the median nerve as it courses between the FDS and FDP muscle bellies, and the ulnar neurovascular bundle adjacent to the deep FDP muscle belly. Protect these neurovascular structures throughout the tenotomy procedures (Figs. 24-3 and 24-4).
The palmaris longus is identified, and a tenotomy is performed proximally within the incision. Identify the FDS and FDP tendons, the median nerve as it courses between the FDS and FDP muscle bellies, and the ulnar neurovascular bundle adjacent to the deep FDP muscle belly. Protect these neurovascular structures throughout the tenotomy procedures (Figs. 24-3 and 24-4).
 Just proximal to the transverse carpal ligament, a nonabsorbable suture is placed across the FDS tendons of the index, long, ring, and small fingers in a running, locking manner. This creates a single tendon unit (Fig. 24-5).
Just proximal to the transverse carpal ligament, a nonabsorbable suture is placed across the FDS tendons of the index, long, ring, and small fingers in a running, locking manner. This creates a single tendon unit (Fig. 24-5).
 Wrist flexion facilitates the exposure of the distal FDS tendons.
Wrist flexion facilitates the exposure of the distal FDS tendons.
 The FDS tendons are then sharply transected as distally as possible (Fig. 24-6).
The FDS tendons are then sharply transected as distally as possible (Fig. 24-6).
Step 1 Pearls
Maintain the superficialis tendons in the position of a normal cascade when placing the stay stitch.
Maximum finger flexion delivers the tendons into the surgical field and takes advantage of the full accessible tendon length.
A myotendinous recession or fractional lengthening may be necessary for the FCR and FCU when there is excessive wrist flexion (similar to fractional lengthening of finger flexors described in previous section). Likewise, if there is an excessive forearm pronation contracture, a release of the pronator teres insertion from the radius can be performed.
Step 2
Step 3
 The FDP tendons are then sharply transected as proximally as possible so that the FDS tendons proximally can be transferred to the FDP tendons distally. The muscle of the FDP will now provide the force for the tendons of the FDS.
The FDP tendons are then sharply transected as proximally as possible so that the FDS tendons proximally can be transferred to the FDP tendons distally. The muscle of the FDP will now provide the force for the tendons of the FDS.
 Suture the distal ends of the superficialis tendons to the proximal ends of the profundus tendons while holding the fingers and wrist in a position of maximum extension. Check finger position and evaluate for corrected finger extension and maintenance of normal finger cascade before wound closure (Fig. 24-9).
Suture the distal ends of the superficialis tendons to the proximal ends of the profundus tendons while holding the fingers and wrist in a position of maximum extension. Check finger position and evaluate for corrected finger extension and maintenance of normal finger cascade before wound closure (Fig. 24-9).
 A nonabsorbable, braided suture is used to secure the transfer. Multiple horizontal mattress sutures or a running, locking technique is used (Fig. 24-10).
A nonabsorbable, braided suture is used to secure the transfer. Multiple horizontal mattress sutures or a running, locking technique is used (Fig. 24-10).
 A layered closure of the subcutaneous tissue with absorbable sutures is performed. The skin is approximated with a monofilament, nonabsorbable suture.
A layered closure of the subcutaneous tissue with absorbable sutures is performed. The skin is approximated with a monofilament, nonabsorbable suture.
Postoperative Care and Expected Outcomes
 Postoperative immobilization is achieved with dorsal and volar splints that hold the fingers and wrist in near-full extension. After swelling subsides (7 to 10 days), the wound is inspected and sutures are removed. Cast immobilization is used for a further 4 weeks.
Postoperative immobilization is achieved with dorsal and volar splints that hold the fingers and wrist in near-full extension. After swelling subsides (7 to 10 days), the wound is inspected and sutures are removed. Cast immobilization is used for a further 4 weeks.
 The patient is then placed into a full-time fabricated forearm-based splint to keep the wrist and fingers in extension. The splint is removed for bathing and hand therapy exercises. Active finger flexion and extension are permitted.
The patient is then placed into a full-time fabricated forearm-based splint to keep the wrist and fingers in extension. The splint is removed for bathing and hand therapy exercises. Active finger flexion and extension are permitted.
 After 1 month of full-time wear, the patient is advanced to wearing the splint at night only. If the patient is skeletally mature, the splint can be discontinued 3 to 6 months postoperatively.
After 1 month of full-time wear, the patient is advanced to wearing the splint at night only. If the patient is skeletally mature, the splint can be discontinued 3 to 6 months postoperatively.
Braun RM, Vise GT, Roper B. Preliminary experience with superficialis to profundus tendon transfer in the hemiplegic upper extremity. J Bone Joint Surg [Am]. 1974;56:466-472.
Keenan MAE, Korchek JI, Botte MJ, et al. Results of transfer of the flexor digitorum superficialis tendons to the flexor digitorum profundus tendons in adults with acquired spasticity of the hand. J Bone Joint Surg [Am]. 1987;69:1127-1132.