CHAPTER 23 Pulse Oximetry
5 How is oxygen saturation determined from the amount of red and infrared light received and absorbed?
6 How does the pulse oximeter determine the degree of arterial hemoglobin saturation?
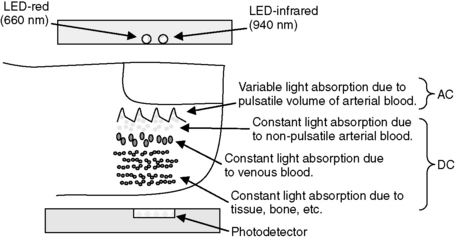
In the vascular bed being monitored, the amount of blood is constantly changing because of the pulsation caused by each heart beat. Thus the light beams pass not only through a relatively stable volume of bone, soft tissue, and venous blood, but also through arterial blood, which is made up of a nonpulsatile portion and a variable, pulsatile portion. By measuring transmitted light several hundred times per second, the pulse oximeter is able to distinguish the changing, pulsatile component (AC) of the arterial blood from the unchanging, static component of the signal (DC) made up of the soft tissue, venous blood, and nonpulsatile arterial blood. The pulsatile component (AC), generally comprising 1% to 5% of the total signal, can then be isolated by canceling out the static components (DC) at each wavelength (Figure 23-1).
8 How does the R/IR ratio relate to the oxygen saturation?
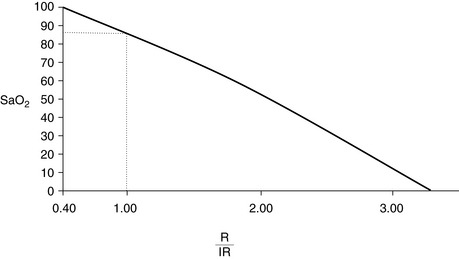
The normalized R/IR ratio is compared to a preset algorithm that gives the microprocessor the percentage of oxygenated hemoglobin in the arterial blood (the oxygen saturation percentage), and this percentage is displayed. This algorithm is derived from volunteers, usually healthy individuals who have been desaturated to a level of 75% to 80%; their arterial blood gas is drawn, and saturation measured in a standard laboratory format. Manufacturers keep their algorithms secret, but in general an R/IR ratio of 0.4 corresponds to a saturation of 100%, an R/IR ratio of 1.0 corresponds to a saturation of about 87%, and an R/IR ratio of 3.4 corresponds to a saturation of 0% (Figure 23-2).
9 What is the oxyhemoglobin dissociation curve?
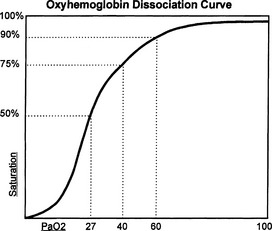
It is a curve that describes the relationship between oxygen tension and binding (percentage oxygen saturation of hemoglobin) (Figure 23-3). Efficient oxygen transport relies on the ability of hemoglobin to reversibly load and unload oxygen. The sigmoid shape of the curve facilitates unloading of oxygen in the peripheral tissues, where the PaO2 is low. At the capillary level a large amount of oxygen is released from the hemoglobin, resulting in a relatively small drop in tension. This allows an adequate gradient for diffusion of oxygen into the cells and limits the degree of hemoglobin desaturation. The curve may be shifted to the left or right by many variables (Table 23-1).
TABLE 23-1 Left and Right Shifts of the Oxyhemoglobin Dissociation Curve
| Right Shift | Left Shift |
|---|---|
| Effects: |
Hb = hemoglobin, 2, 3-DPG = 2, 3-diphosphoglycerate.
10 Why might the pulse oximeter give a false reading? Part 1—not R/IR related
 The algorithm that the pulse oximeter uses to determine the saturation loses significant accuracy as saturation drops below 80% because, as mentioned, healthy volunteers have historically been used to establish these algorithms, and it would be unethical to desaturate someone below 80%. Therefore the percentage saturation below 75% to 80% is extrapolated from these data. As the saturation lowers, it becomes less accurate.
The algorithm that the pulse oximeter uses to determine the saturation loses significant accuracy as saturation drops below 80% because, as mentioned, healthy volunteers have historically been used to establish these algorithms, and it would be unethical to desaturate someone below 80%. Therefore the percentage saturation below 75% to 80% is extrapolated from these data. As the saturation lowers, it becomes less accurate. Saturation is averaged over a time period of anywhere from 5 to 20 seconds. As a patient is desaturating, the reading on the monitor screen will be higher than the actual saturation. This becomes critical as the patient enters the steep part of the oxyhemoglobin desaturation curve because the degree of desaturation increases dramatically and may exceed the ability of the monitor to change rapidly enough to show the true level of oxygen saturation. Likewise, as a person’s saturation increases, the displayed reading on the screen will be lower than the actual saturation.
Saturation is averaged over a time period of anywhere from 5 to 20 seconds. As a patient is desaturating, the reading on the monitor screen will be higher than the actual saturation. This becomes critical as the patient enters the steep part of the oxyhemoglobin desaturation curve because the degree of desaturation increases dramatically and may exceed the ability of the monitor to change rapidly enough to show the true level of oxygen saturation. Likewise, as a person’s saturation increases, the displayed reading on the screen will be lower than the actual saturation. Response time to changes in saturation is related to probe location. Response time is less with ear probes and greater with finger probes and may increase with hypoxia and vasoconstriction.
Response time to changes in saturation is related to probe location. Response time is less with ear probes and greater with finger probes and may increase with hypoxia and vasoconstriction. If the monitor is not able to detect a good pulse during a period of desaturation, it may display an artificially high saturation reading. This is so because when the pulse oximeter cannot find a good pulsation, the prior saturation reading may freeze on the screen while the monitor continues to search for a pulse. Once that patient enters the steep part of the oxyhemoglobin dissociation curve, the difference in the displayed reading and the true saturation can be significant.
If the monitor is not able to detect a good pulse during a period of desaturation, it may display an artificially high saturation reading. This is so because when the pulse oximeter cannot find a good pulsation, the prior saturation reading may freeze on the screen while the monitor continues to search for a pulse. Once that patient enters the steep part of the oxyhemoglobin dissociation curve, the difference in the displayed reading and the true saturation can be significant.11 Why might the pulse oximeter give a false reading? Part 2—R/IR related
 Optical shunting takes place when some of the light from the LED does not pass through the vascular bed before reaching the detector and is a result of poor, incomplete probe placement. The R/IR number trends toward 1.0 (87%) and results in a falsely low measurement for a patient who is actually better saturated. However, if it occurs in a patient who is difficult to ventilate and is desaturating, falsely high measurement will be displayed regardless of how hypoxic the patient becomes.
Optical shunting takes place when some of the light from the LED does not pass through the vascular bed before reaching the detector and is a result of poor, incomplete probe placement. The R/IR number trends toward 1.0 (87%) and results in a falsely low measurement for a patient who is actually better saturated. However, if it occurs in a patient who is difficult to ventilate and is desaturating, falsely high measurement will be displayed regardless of how hypoxic the patient becomes. The penumbra effect, similar to optical shunting, occurs when the probe is not positioned appropriately and the path length between each of the LEDs and the photodetector are not equal, causing a relative distortion in the absorption reading. The R/IR ratio is driven toward 1.0.
The penumbra effect, similar to optical shunting, occurs when the probe is not positioned appropriately and the path length between each of the LEDs and the photodetector are not equal, causing a relative distortion in the absorption reading. The R/IR ratio is driven toward 1.0. Motion artifact causes a low signal-to-noise ratio, alters the absorption detection of both the red and infrared light by the photodetector, drives the R/IR ratio toward 1.0, and results in false saturation readings.
Motion artifact causes a low signal-to-noise ratio, alters the absorption detection of both the red and infrared light by the photodetector, drives the R/IR ratio toward 1.0, and results in false saturation readings. If the probe does not fit well on the finger or ear, fluorescent lighting and operating room lights, because of their phased light production (which is too fast for the human eye to detect) can cause false R/IR readings. When ambient light from either of the above sources is not eliminated, it is detected in both the red and infrared range and fools the microprocessor. As this occurs, the R/IR number is driven toward 1.0 (87% saturation). To minimize false readings from outside lights, pulse oximeters work in three phases, hundreds of times per second. During the first phase a wavelength of 660 nm is emitted, during the second phase a wavelength of 940 nm is emitted, and during the third phase no wavelength is emitted. This third phase allows the photodetector to measure ambient light contamination. The microprocessor then discards the ambient light contamination from its measurements. However, this solution to the ambient light problem is not totally effective; this is why manufacturers recommend placing opaque material over the oximeter probe.
If the probe does not fit well on the finger or ear, fluorescent lighting and operating room lights, because of their phased light production (which is too fast for the human eye to detect) can cause false R/IR readings. When ambient light from either of the above sources is not eliminated, it is detected in both the red and infrared range and fools the microprocessor. As this occurs, the R/IR number is driven toward 1.0 (87% saturation). To minimize false readings from outside lights, pulse oximeters work in three phases, hundreds of times per second. During the first phase a wavelength of 660 nm is emitted, during the second phase a wavelength of 940 nm is emitted, and during the third phase no wavelength is emitted. This third phase allows the photodetector to measure ambient light contamination. The microprocessor then discards the ambient light contamination from its measurements. However, this solution to the ambient light problem is not totally effective; this is why manufacturers recommend placing opaque material over the oximeter probe. Dyshemoglobinemias carboxyhemoglobin (COHb) and methemoglobin (MetHb) pose a problem for accurate oxygen saturation measurement. At 660 nm, COHb absorbs light, much like oxygenated hemoglobin, causing an overestimation of true saturation. The influence of methemoglobinemia on SpO2 readings is more complicated. MetHb looks much like reduced Hb at 660 nm. However, more important, at 940 nm the absorbance of MetHb is markedly greater than that of either reduced or oxygenated Hb. Therefore the monitor reads it as absorption of both species, driving the R/IR number toward 1.0 and the saturation toward 87%. Therefore at a high SaO2 level the probe underestimates the true value; at a low SaO2 the value is falsely elevated.
Dyshemoglobinemias carboxyhemoglobin (COHb) and methemoglobin (MetHb) pose a problem for accurate oxygen saturation measurement. At 660 nm, COHb absorbs light, much like oxygenated hemoglobin, causing an overestimation of true saturation. The influence of methemoglobinemia on SpO2 readings is more complicated. MetHb looks much like reduced Hb at 660 nm. However, more important, at 940 nm the absorbance of MetHb is markedly greater than that of either reduced or oxygenated Hb. Therefore the monitor reads it as absorption of both species, driving the R/IR number toward 1.0 and the saturation toward 87%. Therefore at a high SaO2 level the probe underestimates the true value; at a low SaO2 the value is falsely elevated.15 Since the patient is oxygenated before anesthetic induction, if the pulse oximeter reaches 100%, does this indicate complete denitrogenation?
17 Are there complications associated with the use of pulse oximetry probes?
KEY POINTS: Pulse Oximetry 
1. Barker S. Motion-resistant pulse oximetry: a comparison of new and old models. Anesth Analg. 2002;95:967-972.
2. Moyle J. Pulse oximetry, ed 2. London: BMJ Publishing Group, 2002.
3. Pedersen T., Moller A., Pedersen B. Pulse oximetry for perioperative monitoring: systematic review of randomized, controlled trials. Anesth Analg. 2003;96:426-431.