Procedure 23 Fractional Lengthening of the Flexor Tendons
![]() See Video 20: Fractional Lengthening of the Flexor Tendons
See Video 20: Fractional Lengthening of the Flexor Tendons
Indications
 Wrist and finger flexion deformity due to spastic muscle contracture in which the fingers cannot be passively extended fully despite positioning the wrist in flexion.
Wrist and finger flexion deformity due to spastic muscle contracture in which the fingers cannot be passively extended fully despite positioning the wrist in flexion.
 Situation in which flexor lengthening up to 15% to 20% of the muscle is required; otherwise, superficialis-to-profundus tendon transfer is necessary.
Situation in which flexor lengthening up to 15% to 20% of the muscle is required; otherwise, superficialis-to-profundus tendon transfer is necessary.
 Conditions in which finger and hand flexion is to be preserved for functional purposes. The preoperative condition is functionally limiting, especially with activities of daily living.
Conditions in which finger and hand flexion is to be preserved for functional purposes. The preoperative condition is functionally limiting, especially with activities of daily living.
Examination/Imaging
Clinical Examination
 Preoperative examination is helpful in determing the contribution of the finger and wrist contracture from the spastic properties of the finger flexor tendons.
Preoperative examination is helpful in determing the contribution of the finger and wrist contracture from the spastic properties of the finger flexor tendons.
 Examine the involvement of all muscles that contribute to wrist flexion: palmaris longus, flexor carpi radialis, and flexor carpi ulnaris (FCU), and those primarily responsible for finger flexion: flexor digitorum sublimis and flexor digitorum profundus (FDP).
Examine the involvement of all muscles that contribute to wrist flexion: palmaris longus, flexor carpi radialis, and flexor carpi ulnaris (FCU), and those primarily responsible for finger flexion: flexor digitorum sublimis and flexor digitorum profundus (FDP).
 Excessive flexion of distal interphalangeal (DIP) joints indicates FDP involvement.
Excessive flexion of distal interphalangeal (DIP) joints indicates FDP involvement.
 Excessive flexion of proximal interphalangeal (PIP) joints without significant contracture of DIP joints suggests flexor digitorum sublimis involvement.
Excessive flexion of proximal interphalangeal (PIP) joints without significant contracture of DIP joints suggests flexor digitorum sublimis involvement.
 Examining the wrist in flexion may aid in delineating the effect of the flexor digitorum sublimis from the FDP on the contracture.
Examining the wrist in flexion may aid in delineating the effect of the flexor digitorum sublimis from the FDP on the contracture.
 It is also necessary to examine the small hand articulations to determine the effect of fixed joint contractures. This may represent an articular arthrofibrosis and would not improve with a muscle/tendon procedure.
It is also necessary to examine the small hand articulations to determine the effect of fixed joint contractures. This may represent an articular arthrofibrosis and would not improve with a muscle/tendon procedure.
Surgical Anatomy
 Pertinent surgical anatomy includes the volar forearm muscles (palmaris longus, flexor carpi radialis, flexor carpi ulnaris, flexor digitorum superficialis, FDP, pronator teres, pronator quadratus), median nerve, ulnar nerve and artery, and radial artery. Cross-sectional anatomy should be reviewed before intervention.
Pertinent surgical anatomy includes the volar forearm muscles (palmaris longus, flexor carpi radialis, flexor carpi ulnaris, flexor digitorum superficialis, FDP, pronator teres, pronator quadratus), median nerve, ulnar nerve and artery, and radial artery. Cross-sectional anatomy should be reviewed before intervention.
Exposures
 A longitudinal volar incision over the junction of the mid to distal third of the forearm is used. This corresponds to the myotendinous junction of the volar flexor musculature.
A longitudinal volar incision over the junction of the mid to distal third of the forearm is used. This corresponds to the myotendinous junction of the volar flexor musculature.
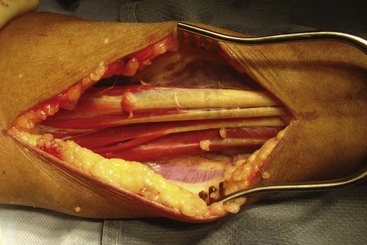
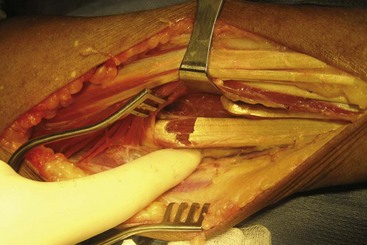
 Division of the volar forearm fascia exposes the underlying musculotendinous junctions (Fig. 23-1).
Division of the volar forearm fascia exposes the underlying musculotendinous junctions (Fig. 23-1).
 Cutaneous volar veins should be mobilized and ligated as necessary.
Cutaneous volar veins should be mobilized and ligated as necessary.
Pearls
The ulnar nerve is more volar and ulnar than the ulnar artery. The FDP tendons are supplied by segmental arterioles from the ulnar artery. Hemostasis of these vessels is important in preventing postoperative hematoma.
Identify the median nerve before any musculotendinous recessions. It can be difficult to differentiate the median nerve from the finger flexor tendons, especially under tourniquet application. The vascularity of the nerve is different from the tendon. The nerve is typically supplied by longitudinal vessels. One cannot rely on the tension of the structures in these severe contracture situations.
Procedure
Step 1
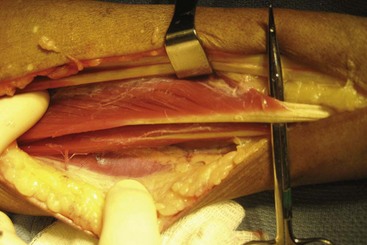
 The tendinous portion of the myotendinous structure is identified, carefully verifying that the muscular portion is in continuity. The tendon is then identified into the distal muscle belly, without disturbing the muscle fibers (Fig. 23-2).
The tendinous portion of the myotendinous structure is identified, carefully verifying that the muscular portion is in continuity. The tendon is then identified into the distal muscle belly, without disturbing the muscle fibers (Fig. 23-2).
 The tendon will be divided at the transition from muscle to tendon. Some of the superficial muscle fibers may need dissection to adequately identify this location.
The tendon will be divided at the transition from muscle to tendon. Some of the superficial muscle fibers may need dissection to adequately identify this location.
 With a wrist flexion contracture, the tendons for the FCR and FCU are first divided. A proximal and distal division of the FCU tendon may be necessary because the myotendinous portion of the FCU extends very distally and over a wide range.
With a wrist flexion contracture, the tendons for the FCR and FCU are first divided. A proximal and distal division of the FCU tendon may be necessary because the myotendinous portion of the FCU extends very distally and over a wide range.
Step 2
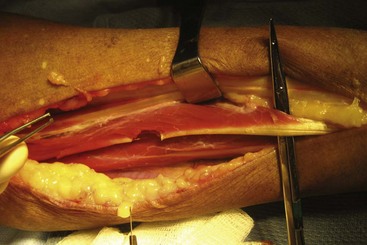
 A sharp tendon division is made at the musculotendinous junction in each flexor digitorum superficialis tendon (Fig. 23-3).
A sharp tendon division is made at the musculotendinous junction in each flexor digitorum superficialis tendon (Fig. 23-3).
 Each digit is passively stretched into extension, allowing the tendon and muscle fibers to slide distally. A 2- to 3-cm gap between the two ends of the tendon will be visualized (Fig. 23-4).
Each digit is passively stretched into extension, allowing the tendon and muscle fibers to slide distally. A 2- to 3-cm gap between the two ends of the tendon will be visualized (Fig. 23-4).
Step 3
 Once all flexor digitorum superficialis tendons are lengthened appropriately, lengthening of the FDP tendons is usually necessary to obtain better digital extension. The examination under anesthesia is helpful in determining the preoperative need to lengthen the FDS and FDP.
Once all flexor digitorum superficialis tendons are lengthened appropriately, lengthening of the FDP tendons is usually necessary to obtain better digital extension. The examination under anesthesia is helpful in determining the preoperative need to lengthen the FDS and FDP.
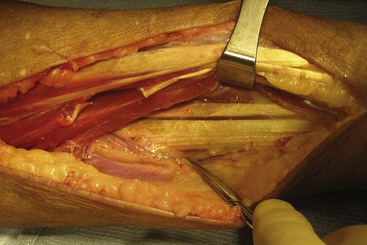
 Meticulous dissection deep to the FDP tendons includes hemostasis of segmental arterioles from the ulnar artery (Fig. 23-5).
Meticulous dissection deep to the FDP tendons includes hemostasis of segmental arterioles from the ulnar artery (Fig. 23-5).
 The FDP tendons are completely visualized and isolated for lengthening (Fig. 23-6).
The FDP tendons are completely visualized and isolated for lengthening (Fig. 23-6).
 A similar tendon division is made at the musculotendinous junction of each FDP tendon (Fig. 23-7).
A similar tendon division is made at the musculotendinous junction of each FDP tendon (Fig. 23-7).
Postoperative Care and Expected Outcomes
 The patient is positioned with the wrist and fingers in extension, as determined by the stretch on the neurovascular structures. A dorsal and volar plaster splint is applied intraoperatively.
The patient is positioned with the wrist and fingers in extension, as determined by the stretch on the neurovascular structures. A dorsal and volar plaster splint is applied intraoperatively.
 After the postoperative swelling has subsided (7 to 10 days), the wound is inspected. A fiberglass cast is applied to maintain the finger and wrist position. The cast is maintained for an additional 4 weeks to allow the muscle and tendon structures to heal in a lengthened position.
After the postoperative swelling has subsided (7 to 10 days), the wound is inspected. A fiberglass cast is applied to maintain the finger and wrist position. The cast is maintained for an additional 4 weeks to allow the muscle and tendon structures to heal in a lengthened position.
 After the cast is removed, a custom wrist-hand orthosis is fabricated to maintain the passive extension achieved intraoperatively. The orthosis is worn for an additional month on a full-time basis, then advanced to night wear only for an additional 3 to 6 months.
After the cast is removed, a custom wrist-hand orthosis is fabricated to maintain the passive extension achieved intraoperatively. The orthosis is worn for an additional month on a full-time basis, then advanced to night wear only for an additional 3 to 6 months.
 The expected outcome of the surgery is improved passive wrist and finger extension.
The expected outcome of the surgery is improved passive wrist and finger extension.