Case 23
Medications: aspirin, furosemide, lisinopril, carvedilol, atorvastatin, spironolactone, and digoxin.
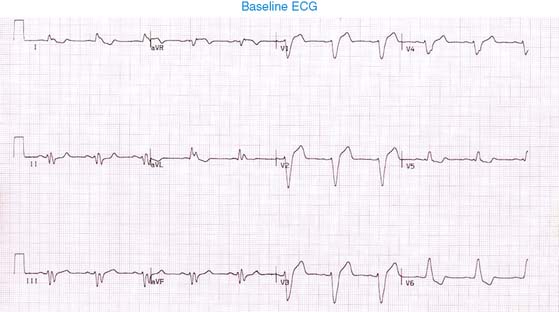
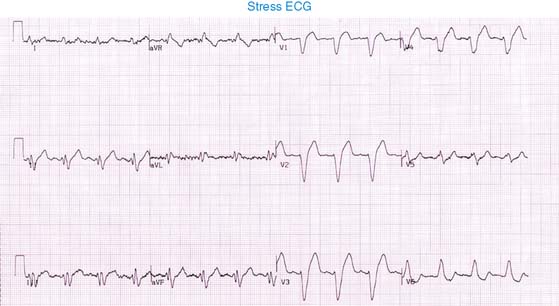
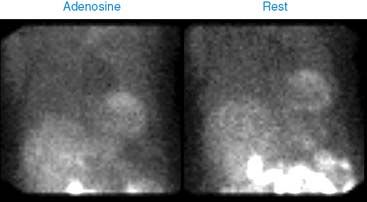
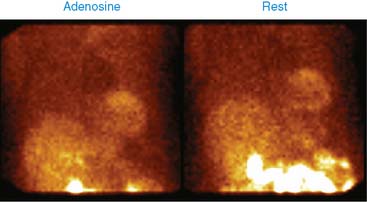
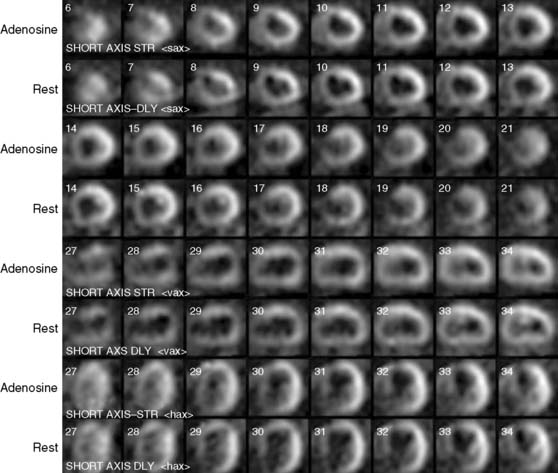
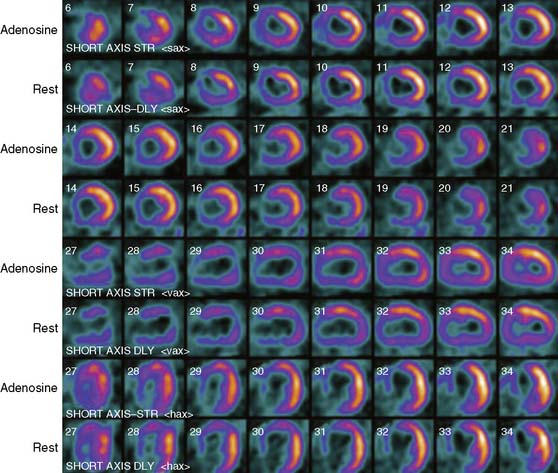
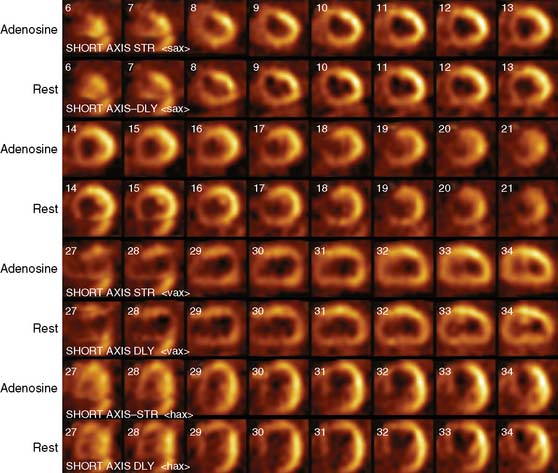
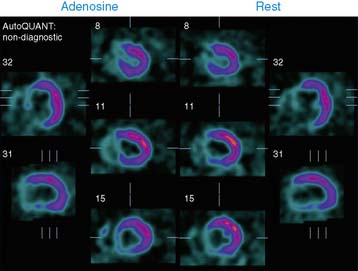
His 99mTc-sestamibi stress and rest images are shown next. What is your interpretation?
1. Tang A.S., Wells G.A., Arnold M., et al. Resynchronization/defibrillation for ambulatory heart failure trial: Rationale and trial design. Curr Opin Cardiol. 2009;24:1-8.
2. Reynolds M.R., Josephson M.E. MADIT II (second Multicenter Automated Defibrillator Implantation Trial) debate: Risk stratification, costs, and public policy. Circulation. 2003;108:1779-1783.