Procedure 20 Tendon Transfers for Radial Nerve Palsy
![]() See Video 16: Standard Tendon Transfer Sequence for Radial Nerve Palsy
See Video 16: Standard Tendon Transfer Sequence for Radial Nerve Palsy
See Video 17: Alternate Tendon Transfer Sequence for Radial Nerve Palsy When PL Is Absent
Examination/Imaging
Clinical Examination
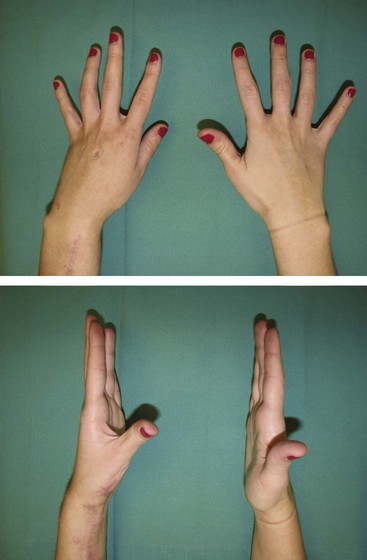
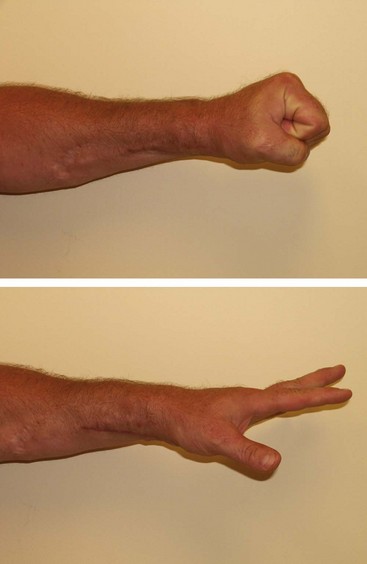
 Functional deficit: The loss of function in radial nerve palsy results from the wrist drop deformity, which causes an inability to extend the wrist and the finger metacarpophalangeal (MCP) joints and to extend and abduct the thumb (Fig. 20-1). The loss of wrist extension weakens power grip, and the loss of finger and thumb extension makes it difficult to grasp objects. It is important to differentiate radial nerve palsy (above the elbow) from posterior interosseous nerve (PIN) palsy (below the elbow). The extensor carpi radialis longus (ECRL) receives its innervation by a branch of the radial nerve that arises above the elbow. It is therefore spared in a lesion of the PIN, and patients can extend the wrist, although with radial deviation (Fig. 20-2).
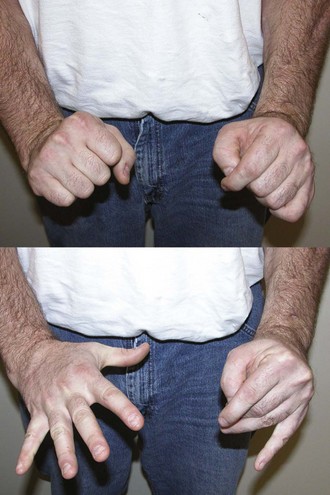
Functional deficit: The loss of function in radial nerve palsy results from the wrist drop deformity, which causes an inability to extend the wrist and the finger metacarpophalangeal (MCP) joints and to extend and abduct the thumb (Fig. 20-1). The loss of wrist extension weakens power grip, and the loss of finger and thumb extension makes it difficult to grasp objects. It is important to differentiate radial nerve palsy (above the elbow) from posterior interosseous nerve (PIN) palsy (below the elbow). The extensor carpi radialis longus (ECRL) receives its innervation by a branch of the radial nerve that arises above the elbow. It is therefore spared in a lesion of the PIN, and patients can extend the wrist, although with radial deviation (Fig. 20-2).
 Sensation: Sensory loss in the areas innervated by the superficial radial nerve (anatomic snuffbox and dorsum of first web) can help differentiate a radial nerve lesion from a lesion of the PIN, which should have preserved sensation over the dorsum of the first web (Fig. 20-3).
Sensation: Sensory loss in the areas innervated by the superficial radial nerve (anatomic snuffbox and dorsum of first web) can help differentiate a radial nerve lesion from a lesion of the PIN, which should have preserved sensation over the dorsum of the first web (Fig. 20-3).
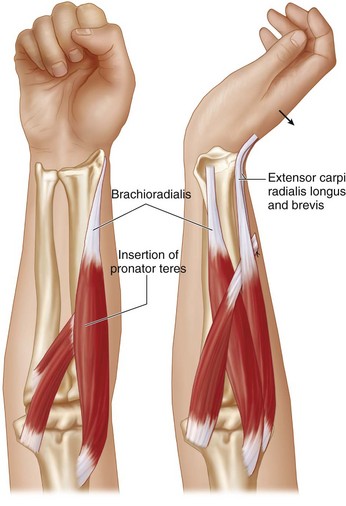
 Joints: To get a good result from the tendon transfer, patients must have good passive range of motion at the wrist and the MCP joint. One of the common transfers uses wrist flexors for obtaining finger and thumb MCP joint extension. The excursion of wrist flexors is approximately 33 mm, whereas finger extension requires a tendon excursion of 50 mm. This difference in excursion is obtained by the natural tenodesis effect, and patients are able to obtain full finger extension when the wrist is flexed.
Joints: To get a good result from the tendon transfer, patients must have good passive range of motion at the wrist and the MCP joint. One of the common transfers uses wrist flexors for obtaining finger and thumb MCP joint extension. The excursion of wrist flexors is approximately 33 mm, whereas finger extension requires a tendon excursion of 50 mm. This difference in excursion is obtained by the natural tenodesis effect, and patients are able to obtain full finger extension when the wrist is flexed.
 Selection of motor: Our preferred motors are as follows. Patients with PIN palsy do not require a transfer for wrist extension because the ECRL is functional.
Selection of motor: Our preferred motors are as follows. Patients with PIN palsy do not require a transfer for wrist extension because the ECRL is functional.
Imaging
 Electrodiagnostic studies are often used to confirm the diagnosis of a nerve problem. For radial nerve palsy, these nerve studies are not particularly useful because muscle testing and careful examination should be able to identify the functional deficits and the available tendons that can be transferred.
Electrodiagnostic studies are often used to confirm the diagnosis of a nerve problem. For radial nerve palsy, these nerve studies are not particularly useful because muscle testing and careful examination should be able to identify the functional deficits and the available tendons that can be transferred.
Surgical Anatomy
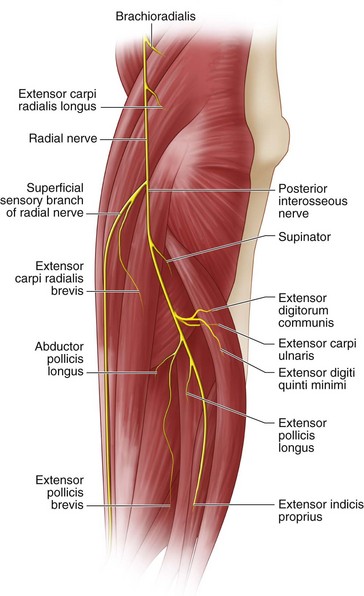
 The radial nerve divides into the superficial radial nerve and the posterior interosseous nerve at the level of the lateral epicondyle (about 1 to 2 cm above the elbow joint). It gives off branches that innervate the brachioradialis (BR) and the ECRL before this division. The ECRB has variable innervation that can arise from the radial nerve, superficial radial nerve, or PIN. The remaining extensor compartment muscles are innervated in the following order by the PIN: supinator, EDC, extensor carpi ulnaris (ECU), extensor digiti quinti minimi (EDQM), abductor pollicis longus (APL), extensor pollicis longus (EPL), extensor pollicis brevis (EPB), and extensor EIP (Fig. 20-4).
The radial nerve divides into the superficial radial nerve and the posterior interosseous nerve at the level of the lateral epicondyle (about 1 to 2 cm above the elbow joint). It gives off branches that innervate the brachioradialis (BR) and the ECRL before this division. The ECRB has variable innervation that can arise from the radial nerve, superficial radial nerve, or PIN. The remaining extensor compartment muscles are innervated in the following order by the PIN: supinator, EDC, extensor carpi ulnaris (ECU), extensor digiti quinti minimi (EDQM), abductor pollicis longus (APL), extensor pollicis longus (EPL), extensor pollicis brevis (EPB), and extensor EIP (Fig. 20-4).
Exposures
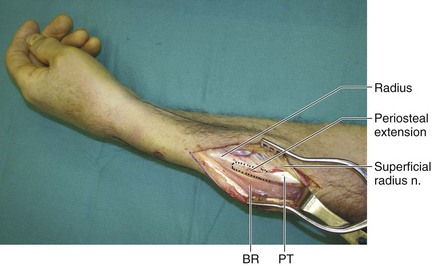
 A 6-cm longitudinal incision is made over the volar radial aspect of the mid-forearm (Fig. 20-5). This incision is centered over the palpable musculotendinous junction of the ECRB and ECRL. The forearm fascia is divided, and the tendons of ECRB and ECRL are identified. The BR is identified radial to the ECRL and retracted ulnarly along with the ECRL. The superficial branch of the radial nerve should be identified under the BR and protected. This will bring into view the insertion of the PT (Fig. 20-6).
A 6-cm longitudinal incision is made over the volar radial aspect of the mid-forearm (Fig. 20-5). This incision is centered over the palpable musculotendinous junction of the ECRB and ECRL. The forearm fascia is divided, and the tendons of ECRB and ECRL are identified. The BR is identified radial to the ECRL and retracted ulnarly along with the ECRL. The superficial branch of the radial nerve should be identified under the BR and protected. This will bring into view the insertion of the PT (Fig. 20-6).
 A 4-cm longitudinal incision is made over the Lister tubercle (see Fig. 20-5). The extensor retinaculum is exposed and the third compartment opened to free the EPL. The EIP, EDC, and EDQM tendons are identified proximal to the extensor retinaculum.
A 4-cm longitudinal incision is made over the Lister tubercle (see Fig. 20-5). The extensor retinaculum is exposed and the third compartment opened to free the EPL. The EIP, EDC, and EDQM tendons are identified proximal to the extensor retinaculum.
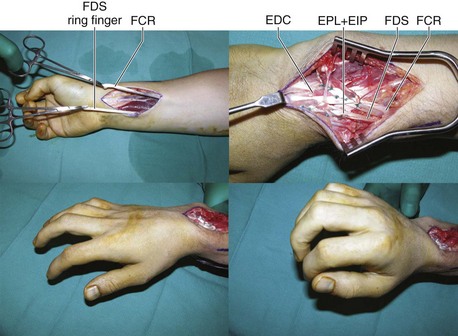
 A 6-cm longitudinal incision is made over the volar aspect of the distal forearm beginning at the proximal wrist crease in line with the FCR (see Fig. 20-5). The tendons of the FCR and the PL are identified, taking care to protect the radial artery, the palmar cutaneous branch of the median nerve, and the median nerve. If the PL is absent, the FDS to the long finger is identified by deeper dissection through the same incision. The long finger is used instead of the ring finger to preserve the strength of the power grip by the ring finger. The FDS tendons to the long and ring fingers lie in a plane superficial to the FDS tendons to the index and small fingers.
A 6-cm longitudinal incision is made over the volar aspect of the distal forearm beginning at the proximal wrist crease in line with the FCR (see Fig. 20-5). The tendons of the FCR and the PL are identified, taking care to protect the radial artery, the palmar cutaneous branch of the median nerve, and the median nerve. If the PL is absent, the FDS to the long finger is identified by deeper dissection through the same incision. The long finger is used instead of the ring finger to preserve the strength of the power grip by the ring finger. The FDS tendons to the long and ring fingers lie in a plane superficial to the FDS tendons to the index and small fingers.
Procedure
Step 1
Step 1 Pearls
A 3- to 4-cm strip of periosteum distal to the insertion of the PT should be harvested in continuity with the PT (see Fig. 20-6). The length of the PT is usually just enough to reach the ECRB, and harvesting this additional periosteal extension makes a strong repair of the PT to the ECRB possible.
A portion of the ECRL tendon can also be used as a tendon graft to strengthen the repair site, given that the ECRL is redundant.
Step 2
Step 4
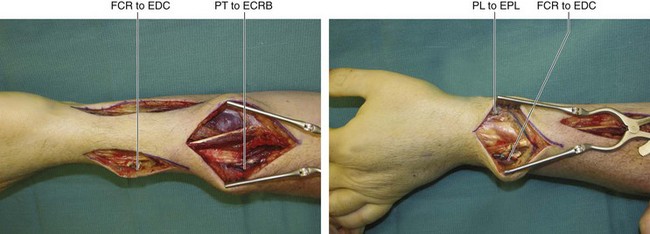
 The PT is sutured end to side to the ECRB using a Pulvertaft weave with multiple 4-0 nonabsorbable sutures (Fig. 20-7). During this suture, the wrist is maintained in 45 degrees of extension by the assistant. A single preliminary suture is placed first, and the tension is confirmed by determining whether the position is maintained without being held by the assistant.
The PT is sutured end to side to the ECRB using a Pulvertaft weave with multiple 4-0 nonabsorbable sutures (Fig. 20-7). During this suture, the wrist is maintained in 45 degrees of extension by the assistant. A single preliminary suture is placed first, and the tension is confirmed by determining whether the position is maintained without being held by the assistant.
Step 4 Pearls
Although dividing the ECRB and doing an end-to-end repair will allow a straighter line of pull, we prefer to do an end-to-side repair. The length of the PT is usually just enough to reach the ECRB, and we feel it is safer to do an end-to-side repair to avoid excessive tension in the tendon repair juncture. An end-to-side repair is also better in patients whose recovery of the radial nerve is expected and in whom the transfer has been done as an internal splint to provide wrist extension in the intervening period.
It is better to err on the side of suturing the extensor tendon transfers too tightly rather than too loosely because the extensors tend to stretch out with time.
Step 5
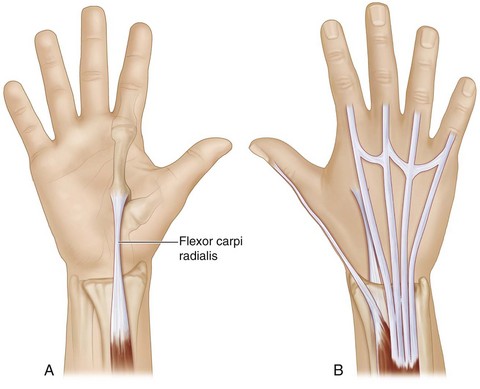
 The FCR tendon (Fig. 20-8A) is divided at the wrist crease and mobilized up to the mid-forearm. A subcutaneous tunnel is made around the radial border of the forearm using a blunt-tipped mosquito forceps that will redirect the FCR tendon in a straight line to the previously exposed EDC tendons (Fig. 20-8B).
The FCR tendon (Fig. 20-8A) is divided at the wrist crease and mobilized up to the mid-forearm. A subcutaneous tunnel is made around the radial border of the forearm using a blunt-tipped mosquito forceps that will redirect the FCR tendon in a straight line to the previously exposed EDC tendons (Fig. 20-8B).
Step 6
 With an assistant holding the wrist in 45 degrees of extension and the finger MCP joint in full extension, the FCR tendon is weaved in an end-to-side fashion to the EDC tendons to the index, long, ring, and small fingers using 4-0 nonabsorbable suture (Fig. 20-9).
With an assistant holding the wrist in 45 degrees of extension and the finger MCP joint in full extension, the FCR tendon is weaved in an end-to-side fashion to the EDC tendons to the index, long, ring, and small fingers using 4-0 nonabsorbable suture (Fig. 20-9).
Step 6 Pearls
The EDQM needs to be included in the transfer only if traction of the EDC does not result in adequate extension of the small finger MCP joint.
The FCR tendon should be sutured to each EDC slip separately, and the tension must be adjusted for each slip individually.
Correct tension can be confirmed by the wrist tenodesis. The fingers should extend fully with the wrist in flexion, and passive flexion of the fingers should be possible with the wrist in full extension (Fig. 20-9).
Some authors have suggested dividing the EDC proximal to the extensor retinaculum, withdrawing it, rerouting it superficial to the retinaculum, and doing an end-to-end repair to allow a straighter line of pull. We do not feel this step is necessary, and our results have been consistently acceptable with our suggested approach.
Step 9
Step 10
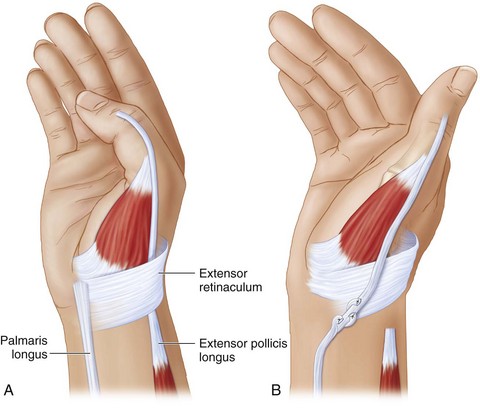
 An end-to-end Pulvertaft weave of the EPL and PL tendons is done with an assistant maintaining the wrist in 45 degrees of extension and the thumb in full extension and abduction (Fig. 20-10).
An end-to-end Pulvertaft weave of the EPL and PL tendons is done with an assistant maintaining the wrist in 45 degrees of extension and the thumb in full extension and abduction (Fig. 20-10).
Step 10 Pearls
Correct tension can be confirmed by wrist tenodesis. The thumb should abduct and extend fully with the wrist in flexion, and passive flexion and adduction of the thumb should be possible with the wrist in full extension (Fig. 20-11; see Fig. 20-9).
If the PL is absent, we transfer the FDS of the long finger to the EIP and EPL (both divided proximal to the extensor retinaculum, withdrawn out, and rerouted superficially). In these cases, the FCR is transferred only to the EDC (including the index finger) and the EDQM (if indicated) (see Fig. 20-9).
Postoperative Care and Expected Outcomes
 A long-arm plaster of Paris splint is applied that keeps the wrist in 45 degrees of extension, the finger MCP joint in full extension, and the thumb in maximum abduction and extension. The finger interphalangeal joints are left free.
A long-arm plaster of Paris splint is applied that keeps the wrist in 45 degrees of extension, the finger MCP joint in full extension, and the thumb in maximum abduction and extension. The finger interphalangeal joints are left free.
 Ten days after surgery, the wound is inspected, sutures are removed, and the position previously described is maintained using a removable splint for 4 weeks. After this time, the splint can be worn as needed and the patient is started on tenodesis exercises under the guidance of a therapist. (Figures 20-12 and 20-13 show the late results of patients shown in Figures 20-1 and 20-2, respectively.)
Ten days after surgery, the wound is inspected, sutures are removed, and the position previously described is maintained using a removable splint for 4 weeks. After this time, the splint can be worn as needed and the patient is started on tenodesis exercises under the guidance of a therapist. (Figures 20-12 and 20-13 show the late results of patients shown in Figures 20-1 and 20-2, respectively.)
 Most reports suggest that tendon transfer procedures for radial nerve palsy are rewarding, with patients demonstrating improved thumb, wrist, and finger extension. On average, patients regained 50% of the power grip and pinch of the normal side. The limitations included difficulty in grasping or releasing large objects and early fatigue.
Most reports suggest that tendon transfer procedures for radial nerve palsy are rewarding, with patients demonstrating improved thumb, wrist, and finger extension. On average, patients regained 50% of the power grip and pinch of the normal side. The limitations included difficulty in grasping or releasing large objects and early fatigue.
Chotigavanich C. Tendon transfer for radial nerve palsy. Bull Hosp Joint Dis Orthop Inst. 1990;50:1-10.
Chuinard RG, Boyes JH, Stark HH, et al. Tendon transfers for radial nerve palsy: use of superficialis tendons for digital extension. J Hand Surg [Am]. 1978;3:560-570.
Skoll PJ, Hudson DA, de Jager W, et al. Long term results of tendon transfers for radial nerve palsy in patients with limited rehabilitation. Ann Plast Surg. 2000;45:122-126.