IDENTIFYING THE PROBLEM
At the start of the 1980s the economic vitality of the state of Victoria was compromised by a range of problems associated with the rising cost of industrial accidents and diseases (estimated nationally to be double the cost of more widely published road accidents). Many of the funds established to pay compensation benefits to injured employees were in financial trouble (see Office of the Insurance Commissioner of Australia 1979, 1983 in Considine 1991). Moreover, the legal system was failing in its ability to efficiently resolve work-injury disputes. Lawyers were widely accused of prolonging disputes, seeking inappropriate settlements, and often being in league with either the trade unions or the employers (Considine 1991 p 21). Finally, the healthcare system was also failing to manage the complexities of work-related injuries and diseases effectively. Consistently, for the same injury, work-injured employees were more costly and achieved slower recovery (see, for example, Caramona et al. 1998) than did patients whose injury was not covered by workers compensation.
This chapter analyses a range of problems associated with two no-fault compensation policies adopted by the state Australian Labor Party government of the day. Both policies are notable for being inadequately implemented. We also describe the consequences of state government policy on the return-to-work outcomes achieved by those receiving benefits and services to support the return to work of those injured at work or in a transport accident.
In terms of health planning and policy, the focus of the chapter is at the operational, rather than the policy formulation, level. The focus is on the specific activities to be undertaken to achieve the policy adopted or social reform desired, and the resources required for effective implementation. Thus, this chapter aims to elucidate the capacity of the service delivery system to produce service outputs (rehabilitation outcomes) in line with the rehabilitation policies adopted by the relevant government or governmental authority.
Dealing with problems of policy implementation also requires effective monitoring of key outcomes – in this case, return-to-work achievements. As seen below, such evaluation revealed no demonstrable improvement to post-injury return-to-work rates when the clients receiving compensation benefits were compared with those on the less generous benefits of government invalid pensions.
The focus of this chapter is deliberately limited. First, the chapter uses ‘return to work’ as an index of ‘successful’ rehabilitation, and thus ignores information about such important matters as quality of life and community reintegration post-injury. Second, the chapter is primarily concerned with policy developments in Victoria, although comparisons with other states are made. The rationale for the focus on Victoria, rather than on other jurisdictions, is provided below.
THE POLICY CONTEXT
Before detailing the policies and return-to-work achievements in Victoria, two broader issues need to be addressed so that the significance of the chapter’s focus on vocational rehabilitation can be properly appreciated. The first is the nexus between vocational reestablishment and effective rehabilitation, and the second, the health benefits of employment.
The salience of vocational goals within rehabilitation
A long line of rehabilitation authorities have specified the vocational domain as essential in the effective rehabilitation of those with chronic conditions or impairments (see Rusk 1949, Britell 1991, Yarkony 1991). One reason that vocational services are prominent within rehabilitation is because it is essentially historically based. In many Western nations, including the United States and Australia, the original legislative basis for rehabilitation services provided services to defined groups, such as the occupationally displaced or returning members of armed forces whose careers had been disrupted by war service. Rehabilitation services to these groups initially had clear and primary vocational goals. Thus Neff in 1971 wrote that, largely because of a societal emphasis on gainful employment as a condition of full citizenship, in the United States “‘rehabilitation” and “vocational rehabilitation” were virtually synonymous terms’ (Neff 1971 p 113).
While the place of work-related services has declined in prominence over the ensuing 20 years (see Murphy 1991), the centrality of work in the rehabilitation process has continued to be stressed by writers in the areas of rehabilitation counselling and rehabilitation medicine or ‘physiatry’. Physiatry is the branch of medicine that uses physical therapy and mechanical apparatus in the diagnosis, prevention and treatment of bodily disorders. Britell clearly presented her view of this:
It is our responsibility to support rehabilitation to its completion. If our patients fail to attain successful employment we have not adequately carried out that responsibility.
The health benefits of employment
Scientific support for the claimed health benefits of employment for the overwhelming majority of individuals is now substantial (see Murphy & Athanasou 1999, McKee et al. 2005). The impact on an individual’s general health and well-being of a move from unemployment to employment is, on average, associated with an effect size of 0.51. The impact of a loss of employment, while significant, is of less magnitude (0.33). The theoretical explanations for these observed effects are less clear. Many theories have been advanced, largely by social psychologists, but no dominant theory has emerged. For those involved in rehabilitation, however, the facts are clear: most employees deteriorate in mental and physical health when they lose their job; and most unemployed persons’ health improves on the gaining of a job. The importance of these facts for those involved in occupational or workers compensation rehabilitation lies in the problems that start to occur when an injured employee is away from the workplace for more than a few weeks. Problems such as depression and disruption of social relationships regularly emerge. If these are not attended to by health professionals involved in occupational rehabilitation, then a relatively minor injury can lead to prolonged periods of work absence, with reducing chances of a successful long-term outcome, such as a stable return to the pre-injury job or suitable alternative.
Most health and rehabilitation professionals are ignorant of the importance of employment in facilitating individual adjustment and community integration. Further, even if they understand the general importance of employment, they generally lack knowledge of the social psychology of work groups and are not skilled in techniques to elicit cooperation from co-workers in the design of a suitable return-to-work plan for particular injured employees (see Murphy et al. 1997a). Additional deficits include a lack of expertise in techniques to facilitate effective job seeking if a new job is required, and in techniques to assist the maintenance of employment gained post-injury. The authors have observed little change to the situation described by Murphy in 1991 as a situation of minimal overlap between the fields of rehabilitation and vocational or organisational behaviour. The service delivery problems caused by such a lack of overlap are serious enough in general rehabilitation, but they are a major impediment to the delivery of effective occupational rehabilitation services. Effective services are those that lead to the overwhelming majority of injured employees returning to work in a timely and satisfactory manner.
WORKERS COMPENSATION POLICY AND POST-INJURY RETURN-TO-WORK ACHIEVEMENTS
The contemporary policy debate about the aims of workers compensation and the benefits, including health and rehabilitation services, available to Australians injured at work started in the years leading up to the Victorian Government’s changes to workers compensation arrangements contained in the 1985 Accident Compensation Act. This legislation ushered in a string of similar ‘no-fault’ workers compensation schemes across the nation. The key players, their goals and their tactics have been well described by Considine (1991). What the Act and subsequent legislation have achieved in terms of optimal return-to-work rates is less clear.
The 1985 Victorian WorkCare scheme
The workers compensation and rehabilitation scheme known as WorkCare was established by the Victorian Government Occupational Health and Safety Act 1985 and involved the creation of a state government authority – the Accident Compensation Commission. This agency was to be responsible for premium collection and benefit allocations, and the establishment of the Victorian Accident and Rehabilitation Council (VARC) whose centres would provide services for up to 40,000 injured or ill workers per year. Politically, the new Act was broadly acceptable because it promised reduced premium costs for employers and guaranteed generous weekly benefits for injured employees regardless of the ‘cause’ of the work-related accident or illness. Significantly, in the negotiations leading to finalisation of the bill, rehabilitation was not to be compulsory, notwithstanding the commitment to rehabilitation established by the creation of the VARC centres.
The economic and operational problems of the WorkCare scheme have been well described elsewhere (see Considine 1991, Rowe 1988), but some of the characteristics of the scheme relevant to its contributions to optimal return-to-work outcomes are as follows:
- There was a lack of agreement regarding the meaning of ‘rehabilitation’ and, thus, for the determination of services to be provided. While employers regarded rehabilitation as services to facilitate a timely return to work, ideally to the same job even if modified to suit the injured employee, the unions had a more social view of rehabilitation. Unions regarded rehabilitation as services for injured workers that would help them overcome or adjust to their injuries and if necessary foster the development of new skills. The unions believed that those whose injuries prevented a return to work would need some form of social rehabilitation. This lack of agreement on the key characteristics of effective rehabilitation led to many services being provided (for example, pain-related treatments) that were not linked to an injured employee’s increased work capacity. Many rehabilitation service plans were approved by VARC which included no workplace visits or input from the employer or local workplace representatives.
- Health professionals and their employing organisations had little understanding of the world of work, and few established the working relationships with employers and unions that would be necessary if rehabilitation was to contribute to lowering workers compensation costs. This was essential if WorkCare was to be financially viable, since employer premiums had been substantially lowered. At the technical level, few health professionals had any training in the analysis of work performance and thus had little understanding of the ways that workplace factors contributed, either positively of negatively, to the ‘on the job’ productivity of any individual employee. Thus the average health professional, whether employed in private practice or in a health or rehabilitation organisation, had little understanding of how to engage organisational members to create individual return-to-work plans that would enable the injured worker to minimise work absence, a factor known to lead to depressed affect and other sequelae, and a key driver of high work-injury costs.
- The VARC, as an organisation, was motivated by clearly articulated welfare values. Many of its staff were recruited from human service professions and viewed their role as providing every support to injured workers. As the proportion of employees receiving benefits, especially those receiving benefits for more than 6 months, increased, VARC came under increased pressure. While there were many contributors to increased claims’ costs, including particularly over-servicing by some health and rehabilitation organisations, the availability of generous income maintenance (80% of regular pre-injury earnings), with no requirement for assessment by rehabilitation professionals, obviously made it more attractive for some to fraudulently claim to be injured or unable to work because of pain. Additionally, the availability of generous income maintenance reduced the pressure on those with chronic ill-health to continue to work in roles they found unsatisfactory.
- Health professionals and their employing organisations had little understanding of the world of work, and few established the working relationships with employers and unions that would be necessary if rehabilitation was to contribute to lowering workers compensation costs. This was essential if WorkCare was to be financially viable, since employer premiums had been substantially lowered. At the technical level, few health professionals had any training in the analysis of work performance and thus had little understanding of the ways that workplace factors contributed, either positively of negatively, to the ‘on the job’ productivity of any individual employee. Thus the average health professional, whether employed in private practice or in a health or rehabilitation organisation, had little understanding of how to engage organisational members to create individual return-to-work plans that would enable the injured worker to minimise work absence, a factor known to lead to depressed affect and other sequelae, and a key driver of high work-injury costs.
The problem of the ‘leaking bucket’
From the first months of implementation it was clear that it would be difficult for the WorkCare scheme to meet its financial targets (see Considine 1991 p 91). Various Victorian Government initiatives were proposed in an April 1986 set of amendments to the scheme (Accident Compensation (Amendment) Bill, 1986) and later that year a formal review of the scheme was undertaken by the Department of Management and Budget (DMB). That review identified two persistent causes of cost pressures. First, the number of claims was higher than expected and second, more importantly, recipients were staying on benefits longer than expected. The implications of these events for the financial viability of WorkCare were obvious. Weekly wage replacement benefits were the major component in calculation of the cost of long-term claims. The bulk of the DMB’s suggestions concerned procedures to reduce the number of workers still on benefits after 6 months. The specific amendments were contained in the Accident Compensation (Amendment) Bill 1987. These amendments gave new powers to the Accident Compensation Commission to terminate benefits where workers were not engaged in rehabilitation or actively seeking work.
The perilous financial situation of an unfunded WorkCare liability—estimated at around $2.7 billion—forced the Victorian Labor Government to agree to a joint committee of both houses to be chaired by a government parliamentarian, Barry Rowe (Rowe 1988). Although the Rowe Committee was required by the government to make its first concern the issue of insurance industry contributions to WorkCare costs, the committee made a number of clear determinations about the quality of rehabilitation service provision. These are central to this chapter’s focus on the effects of workers compensation policy on the return to work of injured employees.
In section 5.4, the committee reported on the ‘Return-to-work performance of the rehabilitation system’. In reviewing the low return-to-work rates achieved (43.8%) when injured workers received rehabilitation through an approved WorkCare rehabilitation provider, the committee explicitly called for ‘A greater vocational emphasis for WorkCare Rehabilitation’ (see Rowe 1988, section 5.4.2). The observations of the committee about the predicted capacity of WorkCare rehabilitation to achieve high return-to-work rates among the group of work-injured people for whom a rehabilitation plan was raised, were clear:
All providers of rehabilitation services in Victoria are required by contract to focus on vocational rehabilitation outcomes. It appears, however, that the weighting given to vocational rehabilitation has not been sufficient. There appears to be a number of reasons for this. One important factor is the medically-orientated training and experience of most of those providing rehabilitation services … Another factor has been the tendency of rehabilitation to proceed without a satisfactory degree of contact with, and involvement of, the worker’s employer.
While the committee made a general recommendation (recommendation 5.32) about the development of options for upgrading the current level of vocational skills in rehabilitation, it is in its preamble to that recommendation that most clearly demonstrates one of the key weaknesses of the WorkCare scheme in terms of its capacity to achieve optimal return-to-work rates. The following skills were said to be in ‘extremely short supply’ within the rehabilitation system:
- skill profiling and occupational assessment of injured workers
- occupational and career counselling
- job search, matching and placement
- knowledge of training and retraining programs
- knowledge of the labour market and job availability on an industry basis
- employer negotiation and advocacy skills on behalf of the worker
- industrial relations knowledge
- job redesign skills.
- occupational and career counselling
Holding aside any consideration of a rehabilitation provider’s patient-communication skills, or skills in communicating with treating doctors, the list probably represents a reasonable summary of the skills and knowledge that one might expect to be essential for a rehabilitation provider to be granted a licence to provide occupational rehabilitation services to an injured worker. Such a lack of skills and knowledge among service providers in any occupational rehabilitation system, regardless of employers’ premium rates and the behaviour of insurance agents, renders the system severely limited in what can be expected to be achieved with respect to return-to-work rates.
Replication of the weaknesses of the Victorian scheme in other jurisdictions
Although the Victorian WorkCare scheme had inherent limitations in its capacity to delivery satisfactorily high, early return-to-work rates, other jurisdictions quickly adopted essentially similar schemes (see Table 20.1).
|
Table 20.1 Jurisdictions and relevant workers compensation legislation |
|
| Jurisdiction | Legislation |
|---|---|
| Victoria | Accident Compensation Act, 1985 |
| NSW | Workers Compensation Act, 1986 |
| SA | Workplace Rehabilitation and Compensation Act, 1986 |
| Commonwealth Government Employees | Commonwealth Employees’ Rehabilitation and Compensation Act, 1988 |
While each scheme had some unique features, all shared a common weakness in terms of capacity to deliver optimal return-to-work rates. This weakness was the use of approved rehabilitation providers who typically had little understanding of work environments, and gave low priority to the full involvement of workplace representatives. The Commonwealth scheme (Comcare) had some advantages over the others in that it at least specified a workplace-based rehabilitation case manager. However, all assessments and most services were still delivered by health professionals who concentrated on ‘therapy’ or other interventions planned by clinicians with little appreciation of the need for the involvement of co-workers or local supervisors and managers in the development and implementation of any return-to-work plan.
Motor vehicle accident insurance and rehabilitation
As well as its national leadership in reform of workers compensation, Victoria was also a policy leader in the area of compensation and rehabilitation for those whose accident involved a registered vehicle. In 1986, the Victorian Government’s Transport Accident Act introduced a no-fault scheme which involved a generous salary-replacement provision for those who lost time from work because of their injury or illness, and virtually full coverage of all hospital, medical and rehabilitation costs. The objects of that legislation are to:
- lessen the cost to the Victorian community of compensation for transport accidents
- provide in the most socially and economically appropriate manner suitable and just compensation in respect of persons injured or who die as a result of transport accidents
- determine claims for compensation speedily and efficiently
- reduce the incidence of transport accidents
- provide suitable systems for the effective rehabilitation of persons injured as a result of transport accidents.
- provide in the most socially and economically appropriate manner suitable and just compensation in respect of persons injured or who die as a result of transport accidents
As an operator of a personal injury insurance scheme, the Transport Accident Commission (TAC) has been successful, not just at operating the scheme profitably, but also by the reductions in traffic accidents achieved. However, in respect of the final aim listed above, almost nothing is known about the effectiveness or otherwise of the rehabilitation offered to those injured in transport accidents in Victoria. Thus, while the commission’s annual reports regularly provide data about the sound financial situation of the scheme, and achievements made in improved road safety, none of its annual reports has ever included any information about the return-to-work achievements of its clients.
While the delivery of rehabilitation services for those with accepted TAC claims is less complicated than in the case of injured workers with a workers compensation claim, in that two major groups (employers and unions) had no formal role in the development and implementation of rehabilitation service plans, the rehabilitation providers approved to deliver services to transport accident victims were almost invariably the same providers involved in delivering occupational (workers compensation) rehabilitation. As such, there was the same lack of understanding of the importance of vocational services in any rehabilitation program and there was minimal involvement of workplace representatives to facilitate post-injury work opportunities. Such lacks weakened the likelihood of high return–to-work rates being achieved by those injured in a traffic accident involving a vehicle registered in the state of Victoria. Some insight into what the TAC’s rehabilitation services contribute to post-injury return to work is suggested by an analysis of the return-to-work achievements of the traumatic spinal cord injury group presented below.
Vocational achievement following work-related or transport accidents
As discussed in Chapter 1, insufficient or inappropriate information is a common problem in both policy formulation and evaluation. There has been little well-controlled research with clearly interpretable results into the return-to-work achievements of those Victorians injured at work or injured through the involvement of a registered motor vehicle. There are many reasons for this lack of reliable information about post-injury return-to-work achievements and post-injury vocational potential, but two of the most persistent limitations of research in this area are: (a) a lack of agreement about the proper measurement of ‘return-to-work’; and (b) the use of research participants whose injuries or health conditions have not been reliably or validly assessed. These limitations are frequently observed internationally and are not unique to the Victorian context. For example, internationally, Knutsdottir (1993) reported a so-called post-injury employment rate of 71%, but this related to those working or studying.
The second methodological limitation frequently observed is the use of study participants whose ‘injury’ is difficult to assess. Frequently, studies are made of those with chronic back pain. As pain is a perception, the homogeneity of these pain patients can neither be assumed, nor can the individual differences in terms of degree of pain be reliably assessed. From the beginning of its no-fault workers compensation reforms, the Victorian Government’s support for research into the outcomes of its occupational rehabilitation scheme was predominantly focused on research into the return-to-work achievements of workers compensation claimants experiencing back injuries, vide the government priority given to the research project undertaken by a university in partnership with a teaching hospital (Victorian WorkCover Authority 1997). In a similar vein, the authority’s main support for rehabilitation service development was focused on two pain management centres, both of which were hospital-based. The ability of such hospital facilities to produce high return-to-work rates among service clients and to provide insights into the full range of factors, including workplace factors, influencing return to work is extremely limited, largely because the hospital staff are disconnected from typical work settings and the health professionals working in pain management centres are generally lacking in skills in vocational counselling and/or job seeking.
Research design for understanding post-injury vocational achievements
The Victorian Government’s Accident Compensation Commission and VARC were not alone in having a limited understanding of the range of factors that impacted on the return-to-work rates achieved following work injury. Internationally, rehabilitation researchers have consistently designed studies which assessed too few of the relevant variables to enable the relative influence on return to work of different sets of relevant factors to be identified. These include the characteristics of the injury and of the individual worker, of the compensation system, of the service delivery system, and of the work place. Unless enough of these sets of factors are assessed, research findings usually will not usefully guide system managers about where to put additional resources in order to achieve higher return-to-work rates.
In the area of workers compensation rehabilitation, an initial framework for the design of appropriate research programs has been described by Foreman and Murphy (2006). These authors recommend that, as a minimum, research projects involving workers compensation rehabilitation clients need to be designed to include assessments of at least three of the following sets of factors: injury severity, individual psychosocial as well as demographic characteristics, service delivery characteristics, and workplace characteristics. Because few research projects in the area of workers compensation rehabilitation assess more than two of the sets of factors, little has been learnt about rehabilitation services beyond the possible identification of those that might or might not lead to improved function in the clinical setting. Usually, it ignores the assessment both of the characteristics of the workplace and of the injured employee’s social environment. A functional capacity in the clinical setting has regularly failed to demonstrate a clear linear relationship with actual improvements in return-to-work behaviour.
Unrealised vocational potential following work or transport accident injury
The previously described methodological problems influenced the design of the rehabilitation research program of Murphy, Young and colleagues (see, for example, Murphy et al. 1997b, Murphy et al. 2003). While their key research questions did not involve comparisons of return-to-work rates achieved by the two populations that are the focus of the current chapter (the populations of work-injured employees, and those injured in traffic accidents) data from their research do suggest underperformance of both the relevant Victorian schemes. Using the most simple ‘comparable’ index of successful rehabilitation outcome (return-to-work status at 6 months post-claim as reported to industry consultants, Campbell Research, versus labour force status as reported to La Trobe researchers by discharged patients when followed up at least 18 months post-injury) the following rates were achieved (see Tables 20.2 and 20.3).
|
Table 20.2 Post-injury labour force status of three groups |
|
| Sub-sample | Post-injury LFS* |
|---|---|
| Workers compensation (n=61) | In the labour force=54% |
| No insurance compensation (n=202) | In the labour force=59% |
| Traffic accident compensation (n=133) | In the labour force=48% |
| *LFS = labour force status | |
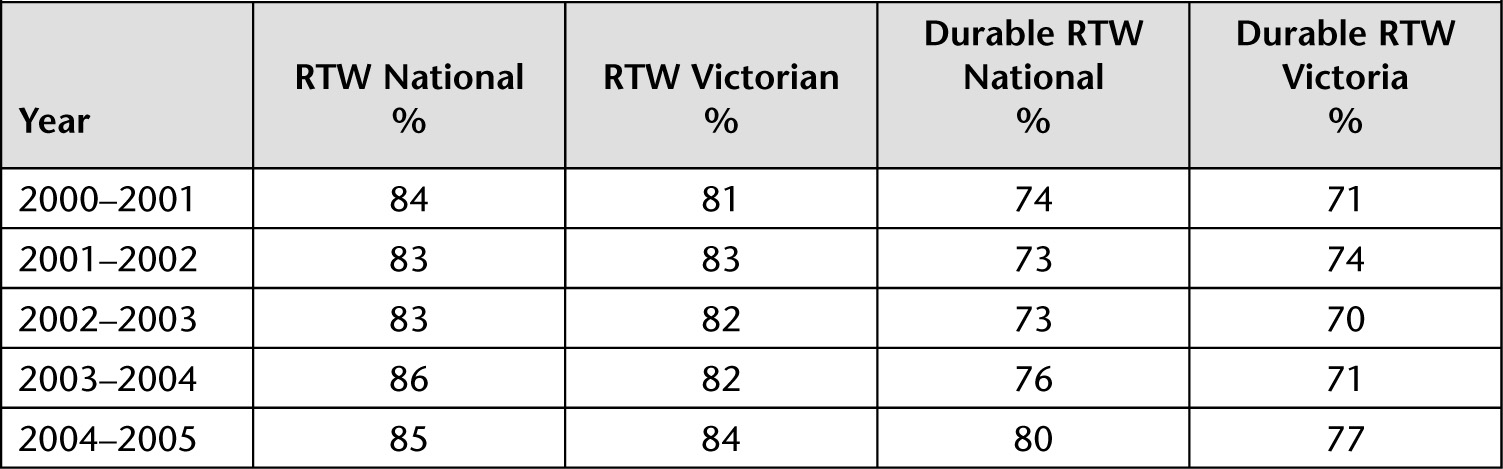
Table 20.3 Return-to-work achievements of those claiming workers compensation 2000–2005: National rates and rates for Victoria
To aid the interpretation of results, Murphy and colleagues first concentrated their studies on those suffering from traumatic spinal cord injury. As there is a well-accepted set of criteria for determining the type of spinal cord injury (see ASIA scale, American Spinal Injury Association 2002), the identification of non-injury factors influencing post-injury return-to-work achievements is relatively straightforward. Additionally, the Australian spinal cord injury population receives treatment that is consistent, regardless of where the injury occurs or where the treatment is delivered. Again, this homogeneity of treatment means that any observed variation in vocational achievements post-injury cannot be attributed to differences in the treatments received by the various study participants; thus, again, the interpretations of study results is more straightforward.
The second characteristic of the research program of Murphy and colleagues that contributes to more interpretative results is the use of an internationally agreed index of post-injury employment – labour force status (see Murphy & Athanasou 1994). Thus, when subjects’ post-injury status is assessed, subjects are reliably classified as either ‘in’ or ‘not in’ the labour force. The rationale for, and validity of, the use of labour force status in these studies of post-injury vocational achievement has been described by Murphy (1999). Table 20.2 provides the figures for vocational achievement post-injury of three sub-samples from the research undertaken by Murphy and colleagues into vocational achievement following traumatic spinal cord injury by those admitted to the Victorian Spinal Cord Service (see Murphy et al. 2003).
The simple percentages displayed in Table 20.2 need, of course, to be interpreted after allowing for any differences between the sub-samples in terms of other factors influencing labour force participation. By using multivariate analyses, one can obtain a clearer picture of the role played by the two insurance schemes. After controlling statistically for age, pre-injury occupation, functional capacity and impairment type (paraplegia versus tetraplegia), there is no reliable effect of either insurance scheme in terms of their impact on labour force participation rates.
While the research program of Murphy and colleagues was not focused specifically on identifying the influence of compensation system status on rehabilitation outcomes achieved following injury, the design of the research does allow for an examination of the influence on rehabilitation outcome of individual and environment factors including insurance system influences. From the analysis of the labour force status of the 396 patients from the Victorian Spinal Cord Service summarised above, there is no evidence of either insurance scheme’s positive impact on post-injury labour force status.
The recent return-to-work performance of the Victorian workers compensation scheme
Over the two decades following the introduction of the WorkCare policy reform, many economic, health system, and government administrative changes have occurred that have affected the return-to-work rates achieved by those receiving occupational rehabilitation. Table 20.3 summarises data from the last 5 years available (see Campbell 2001, 2002, 2003, 2004, 2005). The return-to-work rates, and the data on the durability of returns to work, provide a simple summary of outcomes achieved by work-injured claimants under the relevant state government or Australian government scheme. Note that data come from the population of all those injured and not just from the population of those who received services under an approved rehabilitation plan. Generally, those on a formal rehabilitation plan are more seriously injured and, thus, can be expected to have lower return-to-work achievements and less durability of any return to work initially achieved.
The data in Table 20.3 reveal a simple, consistent fact: Victoria tends to have inferior return-to-work achievements. Particularly noteworthy are the low rates of durable returns to work achieved. Depending on the year, 23–30% of Victorians with a workers compensation claim do not achieve a durable return to work. That is, they either have not returned to work at all when followed up approximately 6 months post-injury, or, if they have returned to work, they have not persisted with that work.
CONCLUSION
The poor return-to-work achievements of the Victorian workers compensation scheme, and the virtually unknown return-to-work achievements of the Victorian transport accident scheme, are clearly the result of a combination of problems. Some are related to the inadequate development of the original policies, and others are clearly related to inadequacies in implementation, including the education and training of various groups of health professionals central to the delivery of services authorised by each scheme.
Two policy issues demand further analysis if solutions to the problem of less than optimal return-to-work rates are to be achieved. First, the level of weekly compensation must be set so that it is both adequate and fair, and yet does not act as a perverse incentive to remain away from work. If set too high, it can mean that some employees become financially worse off when they return to work. It is unknown by what process WorkCare policy makers originally arrived at its figure of 80% of regular pre-injury weekly wage.
Second, attention is needed to deal with the failure to mandate ‘rehabilitation assessment’ as a precondition for receipt of scheme benefits. While there are obvious competing interests in respect of which professional group is best equipped to make such assessments, the fact that there is no common metric for assessing the severity of injury precludes even the simplest analyses of rehabilitation outcomes achieved by various providers or with various injury groups (or indeed analyses of the relative performance of the Victorian scheme as opposed to similar schemes in other jurisdictions).