Hematologic Products
Objectives
1. Describe the influence of anticoagulants on blood clotting.
2. Develop a teaching plan for patients taking anticoagulants on a long-term basis.
3. Identify at least three adverse reactions associated with hematologic products.
4. Identify drugs that act in the formation, repair, or function of red blood cells.
Key Terms
anticoagulants (ăn-tĭ-kō-ĂG-ū-lĕnts, p. 354)
fibrin (FĪ-brĭn, p. 354)
fibrinogen (fī-BRĬN-ō-jĕn, p. 354)
thrombi (THRŎM-bī, p. 354)
thromboplastin (thrŏm-bō-PLĂS-tĭn, p. 354)
Overview
![]() http://evolve.elsevier.com/Edmunds/LPN/
http://evolve.elsevier.com/Edmunds/LPN/
Hematologic products act in the formation, repair, or function of red blood cells. There are four major groups of medications that have hematologic effects. They include the anticoagulants (heparin and warfarin [Coumadin]) and the heparin antagonist protamine sulfate. Thrombolytic agents and antiplatelet factors also have a major influence on blood clotting. Related vitamins and minerals needed for red blood cell development are iron, vitamin K, vitamin B12, and folic acid; these are presented in Chapter 24.
Anticoagulants
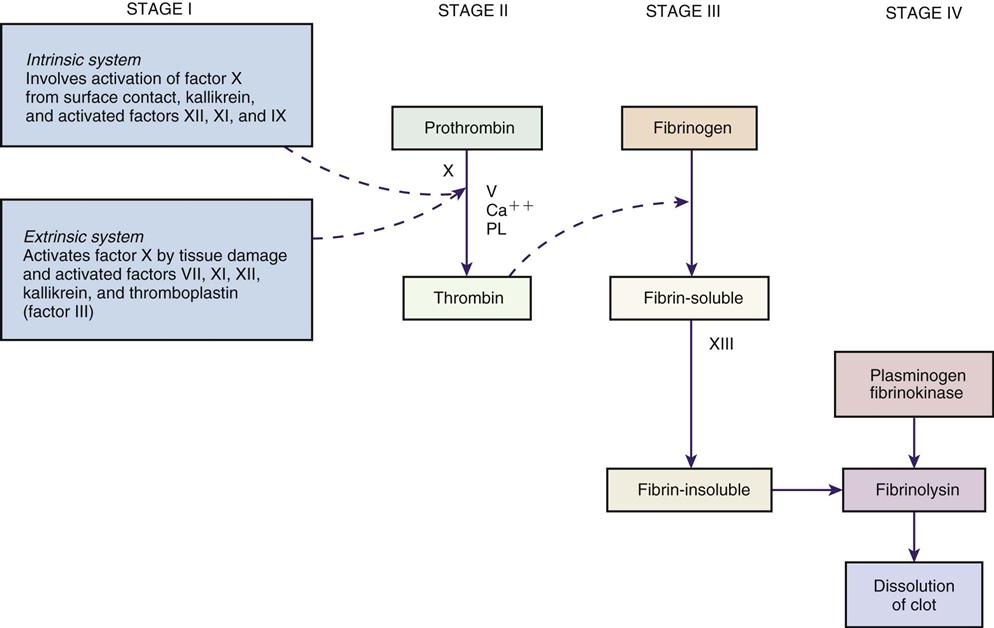
One of the body’s protective functions is to clot blood in response to tissue injury. Any damage to the cells starts a series of chemical reactions to protect the body (Figure 20-1). Cellular damage results in the formation of thromboplastin, which then acts on prothrombin to form thrombin. Calcium must be present for this reaction to occur. Thrombin then acts on fibrinogen (a protein found in the blood plasma) to produce fibrin, a netlike substance in the blood that traps red and white blood cells and platelets and forms the matrix, or skeleton, of the clot. Vitamin K must be present to produce prothrombin and other clotting factors that are made in the liver. All anticoagulants prevent the formation of blood clots, or thrombi, by interfering with this complex clotting mechanism of blood and increasing the time it takes for blood to clot. In cases of overdose, protamine sulfate is given to counteract the effect of heparin. In response to some bleeding disorders, vitamin K may be given either orally or parenterally to manufacture prothrombin and serve as an anticoagulant antagonist (see Chapter 24).
Action 
There are two major categories of anticoagulants. The first category, the coumarin and indanedione derivatives, limits formation of blood coagulation factors II, VII, IX, and X in the liver by interfering with vitamin K. These drugs do not destroy existing blood clots; however, they may limit the extension of existing blood clots or thrombi.
The second category, heparin sodium, acts at multiple sites in the normal coagulation system to stop reactions that lead to the clotting of blood and the formation of fibrin clots. It increases the action of antithrombin III (heparin cofactor) on several other coagulation factors, primarily activated factor X (Xa), to slow new clot development. Heparin does not dissolve existing clots either, although thrombolytic agents do. Low-molecular-weight heparin is a special formulation used in special circumstances, such as to prevent deep vein thrombosis (DVT) after surgery.
Uses
As part of the circulatory system, the arterial vessels carry oxygenated blood throughout the body. If these small arteries become plugged with thrombi (clots made of fibrin, platelets, and cholesterol), oxygen cannot get to the tissues, and death may result. Abnormal blood clotting may produce a thrombus in the coronary artery, which nourishes the heart muscle. Emboli (small pieces of a blood clot) may break off from a site of thrombophlebitis (inflammation and blood clot in a vein) in the lower extremities and travel through the bloodstream to block vessels in areas of the heart, brain, or lung. (See Chapter 15, Figure 15-7.) This blockage can cause stroke or death. Drugs that can slow or reduce clotting, then, are very helpful.
Anticoagulant therapy is used to prevent new clot formation or to stop existing clots from growing in size. Anticoagulant therapy is used prophylactically during and after many types of surgery, especially surgery involving the heart or circulation. It is also used in patients with heart valve disease, in patients with some dysrhythmias (irregular heartbeats), and in patients receiving hemodialysis. Any patient on bed rest for a long time is at risk for development of blood clots, especially patients with a history of clotting problems or recent orthopedic, thoracic, or abdominal surgery.
Heparin is the anticoagulant of choice when an immediate effect is needed. For long-term therapy, a coumarin or indanedione derivative is used. The U.S. Food and Drug Administration has classified coumarin preparations as “possibly” effective as part of the therapy for treatment of transient cerebral ischemic attacks. Indanedione derivatives (phenindione) are used to treat pulmonary emboli and as prophylaxis to treat DVT, myocardial infarction, rheumatic heart disease with valve damage, and atrial dysrhythmias. Low-intensity warfarin therapy (prothrombin time [PT] ratio between 1.2 and 1.5) greatly decreases the risk of stroke from nonrheumatic atrial fibrillation and has few side effects.
Adverse Reactions
By far, the most common adverse reactions from heparin and warfarin are excessive bleeding and thrombocytopenia. Early signs of overdose or internal bleeding include bleeding from gums while brushing teeth, excessive bleeding or oozing from cuts, unexplained bruising or nosebleeds, and unusually heavy or unexpected menses in women. These are the “must know” symptoms that suggest the patient needs prompt attention.
There are a number of other adverse reactions that may occasionally be seen. Warfarin may produce alopecia (hair loss), rash, urticaria (hives), cramping, diarrhea, intestinal obstruction, nausea, paralytic ileus, vomiting, excessive uterine bleeding, hemorrhage with excessive dosage, leukopenia, and fever. Heparin sodium may produce hypertension (high blood pressure); headache; hematoma, irritation, and pain at the injection site; conjunctivitis; tearing of eyes; rhinitis; frequent or persistent erection; hemorrhage; thrombocytopenia; shortness of breath; wheezing; chills; fever; alopecia; and hypersensitivity (allergic) reaction.
Drug Interactions
Other anticoagulants (coumarin or indanedione derivatives), methimazole, and propylthiouracil increase the anticoagulant effect of heparin.
Antihistamines, digitalis, nicotine, and tetracycline decrease the anticoagulant effect of heparin.
Acetylsalicylic acid (ASA), coumarin-derivative anticoagulants, dextran, nonsteroidal antiinflammatory drugs (NSAIDs), and other selected drugs increase the risk of bleeding and hemorrhage in a patient receiving heparin.
ASA, corticotropin, ethacrynic acid, glucocorticoids, and NSAIDs increase the risk of gastrointestinal (GI) bleeding and hemorrhage in a patient receiving heparin.
Allopurinol, ASA, anabolic steroids, antibiotics, androgens, many sedatives, some antacids, dextran, disulfiram, drugs affecting blood elements, glucagon, heparin, narcotics (with prolonged use), phenylbutazone, propylthiouracil, quinidine, quinine, salicylates, thyroid drugs, and vitamin E increase the PT response of patients receiving warfarin.
Adrenocorticosteroids, antacids, antihistamines, barbiturates, contraceptives (oral), estrogens, griseofulvin, haloperidol, meprobamate, primidone, rifam-pin, thiazide diuretics, and vitamin K decrease the PT/International Normalized Ratio (INR) response of a patient on warfarin.
Anticoagulant effects may be increased with acute alcohol intoxication and decreased with chronic alcohol abuse. Oral hypoglycemics taken with anticoagulants may increase the effect of either the hypoglycemic or anticoagulant.
Alkylating agents, antimetabolites, corticosteroids, ethacrynic acid, indomethacin, quinidine, and salicylates increase the risk of bleeding in a patient taking warfarin.
 Nursing Implications and Patient Teaching
Nursing Implications and Patient Teaching
Patients requiring rapid anticoagulation are commonly hospitalized. Coagulation and PT/INR tests are ordered when the patient is started on anticoagulants. Heparin is usually started for an immediate effect and gradually replaced by oral anticoagulants. Thereafter, the physician or other health care provider orders coagulation and PT/INR tests at regular intervals. When the oral anticoagulant shows proper effect, and the prothrombin activity is in the therapeutic range, heparin therapy may be stopped and the oral anticoagulant therapy continued.
Standard heparin dosing protocols have been controversial for many years. Weight-based dosing is now the standard of care for determining the dosing of heparin. Weight-based dosing uses the patient’s body weight in kilograms, infusing 80 units/kg as an intravenous (IV) bolus. The maintenance infusion is 18 units/kg/hr through an infusion pump. There are indications that weight-based dosing is safer, achieves therapeutic levels in less time than with standard dosing, and results in fewer bleeding complications and a lower rate of thromboembolic recurrences.
The standard tests for determining the general effect of heparin on clotting are the Lee-White coagulation time, the whole-blood activated partial thromboplastin time, and the activated partial thromboplastin time (aPTT). The most commonly used test is the aPTT. The dosage of heparin is considered adequate when the whole blood clotting time is approximately 1.5 to 2.5 times the control value. The recommended method for establishing the unfractionated therapeutic range is by the anti-Xa method. This method is the most specific and is least affected by the variables inherent to the in vitro technique. Samples are collected from patients on unfractionated heparin. The samples are tested with aPTT and anti-Xa assays. The range of aPTT values correlate to anti-Xa levels in a range of 0.3-0.7 U/mL of heparin.
PTs are used to determine the dosage for coumarin preparations. These PT tests are done daily until the results stabilize in the therapeutic range ( to
to  times the normal control value). After stabilization, tests are performed at 1-week to 4-week intervals, depending on patient status. Unfortunately, these test results vary from laboratory to laboratory and from day to day because of variations in the reagent chemical used to perform the test. However, this test is still used in many countries.
times the normal control value). After stabilization, tests are performed at 1-week to 4-week intervals, depending on patient status. Unfortunately, these test results vary from laboratory to laboratory and from day to day because of variations in the reagent chemical used to perform the test. However, this test is still used in many countries.
To avoid test variation, a system called the International Normalized Ratio (INR) is used to standardize PT reporting so that all laboratory reports are the same. The INR is based on the PT ratio supplied by the drugmaker that would be obtained if a standard reference testing chemical was used. PT numbers are changed to INR measurements by a standard math equation. Laboratories commonly report both numbers (PT/INR) when a PT is ordered.
The goal of prolonging the PT to 1.5 to 2.5 times the normal has largely been replaced in the United States and some other countries by specific INR goal recommendations for each clinical indication. The typical INR goal is 2 to 3, except in mechanical cardiac valve replacement, in which a higher INR is necessary to prevent clot formation.
n Assessment
Learn as much as possible about the patient’s health history, including the presence of hypersensitivity, underlying systemic disease, the current nature of the problem, and use of other medications. Inquire about conditions that contraindicate use of some anticoagulants, such as alcoholism; blood dyscrasias; bleeding tendencies of the GI, genitourinary, or respiratory tracts; or malignant hypertension. Patients with congestive heart failure may be more sensitive to coumarin anticoagulants and indanedione derivatives.
Heparin is derived from animal tissue and should be used with caution in any patient with a history of allergy. This drug should be used cautiously in patients with hepatic or renal disease or hypertension, during menses, after delivery, or in patients with indwelling catheters. A higher incidence of bleeding may be seen in women older than the age of 60. Make absolutely sure that female patients taking a coumarin or indanedione derivative are not pregnant or breastfeeding. These drugs are usually not given to children.
n Diagnosis
There are many medical and surgical contraindications to the use of anticoagulant drugs, particularly in patients who have recently had surgery, trauma, or obstetric complications. Review the patient’s problems and make certain that none of these contraindications exist.
n Planning
The dosages listed for heparin are given in United States Pharmacopeia heparin units. Heparin is not effective if given orally and should be given by IV injection, IV infusion, or deep subcutaneous (intrafat) injection. Heparin should not be given via intramuscular (IM) injection because these injections produce hematomas, irritation, and pain at the injection site. Use a small (25-gauge) needle and a tuberculin syringe for the subcutaneous intrafat injection.
n Implementation
Anticoagulant drugs should not be used if good laboratory facilities are not available, or if the patient is not compliant in taking medications or keeping appointments for laboratory and health assessment. Coumarin derivatives should not be used in a patient undergoing diagnostic or therapeutic procedures with risk for uncontrolled bleeding.
The sites of intrafat injections of heparin should be rotated to avoid formation of hematomas. (See Chapter 10, Figure 10-16, for rotation site suggestions.) Because of the adverse effects if inaccurate doses are given, once the heparin is drawn into the syringe, double check the dose with another nurse. There are several things to remember about heparin injection that make the process unique. First, do not attempt to pull back on the plunger or aspirate blood before injection. Second, the nurse must be extra careful to not move the needle while the heparin is being injected. Third, injection sites should not be massaged before or after injection. Patients receiving heparin are not good candidates for IM injections of other medications, because hematomas and bleeding into nearby areas may occur.
If the heparin solution is discolored or contains a precipitate (solid at the bottom), it must not be used. Heparin is strongly acidic and is chemically incompatible with many other medications in solution, so it must not be piggybacked with other drugs into an infusion line. Never mix any drug with heparin in a syringe when bolus therapy is given.
If intermittent IV therapy is being given, blood for partial thromboplastin time determination should be drawn  hour before the next scheduled heparin dose. Blood for partial thromboplastin times can be drawn anytime after 8 hours of continuous IV heparin therapy. However, blood should not be drawn from the tubing of the heparin infusion line or from the vein being used for infusion. Blood should always be drawn from the arm not being used for heparin infusion.
hour before the next scheduled heparin dose. Blood for partial thromboplastin times can be drawn anytime after 8 hours of continuous IV heparin therapy. However, blood should not be drawn from the tubing of the heparin infusion line or from the vein being used for infusion. Blood should always be drawn from the arm not being used for heparin infusion.
If heparin is being given at the same time as a coumarin or an indanedione derivative, blood should not be drawn for PTs within 5 hours of IV heparin administration or 24 hours if heparin is given subcutaneously. IV heparin infusions should be checked frequently, even if pumps are in good working order, to make sure the proper dose is being given.
If anticoagulant therapy is started with heparin and continued with a coumarin or indanedione derivative, it is recommended that both drugs be given until the PT or INR results indicate an adequate response to the coumarin or indanedione derivative.
A summary of anticoagulants is provided in Table 20-1.
![]() Table 20-1
Table 20-1
Anticoagulants and Other Drugs Affecting the Blood
| GENERIC NAME | TRADE NAME | COMMENTS |
| Anticoagulants | ||
| Coumarin and Indanedione Derivatives | ||
| warfarin (sodium) |
Coumadin | Dosage individualized for patient and problem. Usual initiation dose is 2-5 mg/day, with dosage adjustments based on the results of INR and/or PT ratio determinations. Store tablets at 59° F to 86° F, and protect from air and light. |
| Heparin | ||
| heparin |
Heparin |
Dosage is adjusted according to patient’s coagulation time. q4h |
| Low-Molecular-Weight Heparins | ||
| dalteparin sodium | Fragmin | Given SQ for DVT prophylaxis and treatment for DVT/PE, MI. |
| enoxaparin | Lovenox |
Given SQ for DVT prophylaxis and treatment for DVT/PE, MI. |
| tinzaparin | Innohep | Given for DVT/PE treatment. |
| Heparin Antagonist | ||
| protamine sulfate | Protamine Sulfate | The onset of action for protamine sulfate is 0.5-1 min. The duration of action is 2 hr. Adults and children: 1 mg of protamine sulfate for every 90 USP units of beef lung heparin or for every 115 USP units of porcine intestinal mucosa heparin to be neutralized. Administer IV at a slow rate over 1-3 min (limit is 50 mg given in 10 min). Additional doses may be given if need is indicated by coagulation studies. |
| Thrombolytic Agents | ||
| Tissue Plasmogen Activators | ||
| alteplase, recombinant | Activase | For lysis of coronary artery thrombi (accelerated infusion): Best results if given IV within 6 hr of onset of symptoms of MI. Dosage is determined by patient weight. An IV bolus is given first followed by IV infusion over 60 min. May be slightly more effective but costs 10 times more than other products. Pulmonary embolism or acute ischemic stroke: Must administer within 3 hr after onset of symptoms. 10% of the total dose is given as an IV bolus over 1 min then the remaining dose is administered over 60 min. |
| reteplase | Retavase | Given as a double bolus with first bolus IV over 2 min then another IV bolus 30 min later. |
| tenecteplase | TNKase | Dose is weight based. Do not give more than 50 mg; by IV administration only. Do not exceed recommended volume per 5 sec when giving as IV bolus. |
| Antiplatelet Agents | ||
| abciximab | ReoPro | Give IV bolus administered 10-60 min before the start of PTCA, followed by a continuous IV infusion for 12 hr. |
| acetylsalicylic acid |
ASA | Give 325-650 mg PO (chewed) stat with first indication of MI. Do not give ASA in addition to coumarin anticoagulants. |
| anagrelide | Agrylin | Used in treating essential thrombocythemia to reduce elevated platelet count and the risk of thrombosis. Give daily for about 1 wk and then adjust to lowest effective dosage required to reduce and maintain platelet count, 600,000/mL. |
| cilostazol | Pletal | For intermittent claudication, give daily approximately 30 min before or 2 hr after breakfast and dinner. May need a smaller dose if concurrent administration of some CYP3A4 drugs. |
| clopidogrel | Plavix | Give with or without food. No adjustment necessary for older adult patients or those with renal disease. |
| dipyridamole | Persantine | Give daily as adjunct to warfarin therapy. |
| ticlopidine | Ticlid | Give with food. |
| Other Miscellaneous Products | ||
| antihemophilic factor | Hemofil M/E Koate-HPMonoclate P | Used in treating patients with hemophilia A. Individualize dosage based on needs of patient. |
| antiinhibitor coagulant complex | Autoplex T/E Feiba VH | Individualize dosage based on needs of patient. |
| antithrombin III | Thrombate III | Used in treating patients with hereditary antithrombin III deficiency. Individualize dosage based on needs of patient. |
| eptifibatide | Integrilin | Give IV bolus as soon as possible after diagnosis of acute coronary syndrome, followed by continuous infusion of 2 mcg/kg/min until hospital discharge or CABG surgery. |
| hydroxyurea | Droxia | Antisickling agent. The patient’s CBC count must be monitored every 2 wk. |
| pentoxifylline | Trental | Used in intermittent claudication from chronic occlusive arterial disease and in cerebrovascular insufficiency. Give with meals. Decrease dosage if GI side effects develop. |
| tirofiban | Aggrastat | Used with heparin in the treatment of acute coronary syndrome, including patients who are to be managed medically and those with PTCA. Can be administered in the same IV catheter as heparin. Give for 48-108 hr, including during surgical procedure and after. Medication must be diluted and administered according to the patient’s weight. |
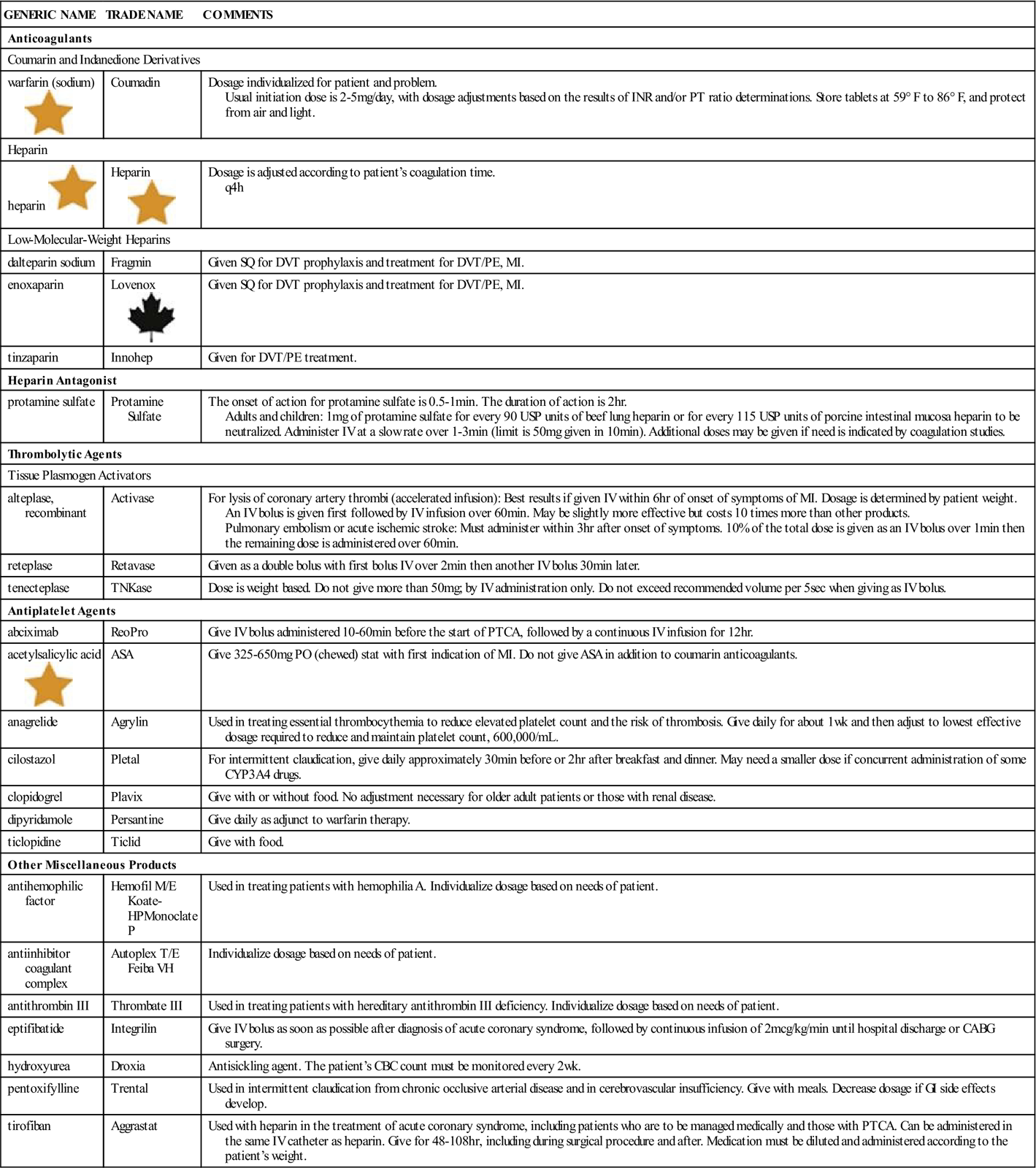
ASA, Acetylsalicylic acid; CABG, coronary artery bypass grafting; CBC, complete blood cell; DVT, deep vein thrombosis; INR, international normalized ratio; IV, intravenous; MI, myocardial infarction; PE, pulmonary embolism; PO, by mouth; PT, prothrombin time; PTCA, percutaneous transluminal coronary angioplasty; SQ, subcutaneous.![]() Indicates “Must-Know Drugs,” or the 35 drugs most prescribers use.
Indicates “Must-Know Drugs,” or the 35 drugs most prescribers use.
n Evaluation
If heparin is given by continuous IV infusion, the coagulation time should usually be determined every 4 hours in the early stages of treatment. Many medical centers have adopted evidenced-based protocols that indicate heparin dosing based on previous aPTT results and when the next aPTT should be drawn.
Watch for signs of overdose of anticoagulants and internal bleeding as therapy progresses. This might include bleeding gums when brushing teeth, blood in the urine, or coughing up blood.
Determine whether the patient understands why he or she is taking the medicine and the symptoms of overdose. Have the patient explain to the nurse if he or she notices signs of bruising or easy bleed-ing. More accurate patient monitoring of antico-agulant response is a Joint Commission National Patient Safety Goal, and many hospitals are adopting new protocols for required patient teaching and clinical monitoring.
n Patient and Family Teaching
Protamine Sulfate
Action
Protamine sulfate is a strongly basic (alkaline) protein that acts as a heparin antagonist to neutralize (reverse) the actions of heparin. However, it may also serve as an anticoagulant when used as the sole medication. In the presence of heparin, it forms a stable salt, which is strongly acidic. This cancels out the anticoagulant activity of both drugs. When protamine sulfate is used with heparin, these results occur almost immediately and may persist for 2 hours or more.
Uses
Protamine sulfate is used to treat heparin overdose. It may also be used after surgical procedures to neutralize the effects of heparin given during extracorporeal circulation on a heart-lung machine.
Adverse Reactions
Adverse reactions to protamine sulfate include bra-dycardia (slow heartbeat), dyspnea (uncomfortable breathing), lassitude (weariness), sudden drop in blood pressure, transitory flushing (red color in the face and neck), and a feeling of warmth. Overdose may produce anticoagulant effects.
 Nursing Implications and Patient Teaching
Nursing Implications and Patient Teaching
n Assessment
Because of the anticoagulant activity of protamine sulfate, overdoses of this drug when used as a heparin antagonist may produce additional anticoagulation.
n Diagnosis
Does the patient have any other problems that might result from excessive anticoagulation? Is the patient taking other medications or using a diet that would interfere with anticoagulation?
n Planning
Protamine sulfate may be inactivated by blood. Thus there may be a rebound effect when a large dose is used to neutralize heparin. This requires an increased dose of protamine sulfate. Hyperheparinemia or bleeding may be seen in some patients 30 minutes to 18 hours after open-heart surgery, even when adequate amounts of protamine sulfate have been given.
n Implementation
Protamine sulfate should be given only by a physician. The nurse would usually assemble the medications but allow the physician to draw up the dose. It should be given slowly by IV injection over 1 to 3 minutes in doses not exceeding 50 mg of protamine sulfate activity (5 mL) during any 10-minute period. It is rare that more than 100 mg is given at a time.
Severe hypotension and anaphylactic-like reactions may be provoked if it is given too rapidly. This drug contains no preservatives, so the unused portion of the medication in the ampule should be discarded.
n Evaluation
Closely monitor the patient for signs of further anticoagulant activity, and have equipment readily available to treat shock.
n Patient and Family Teaching
The family and patient should know that this is a standard drug used to neutralize heparin. See Table 20-1 for information on protamine sulfate and other hematologic products.
Thrombolytic Agents 
Action
Thrombolytics convert plasminogen to the enzyme plasmin, which degrades or breaks down fibrin clots, fibrinogen, and other plasma proteins. These products are used for lysis (dissolving) of thrombi.
Uses
Thrombolytic agents are used in acute myocardial infarction for lysis of thrombi blocking coronary arteries, in acute pulmonary emboli for clot lysis when the patient is hemodynamically unstable, and in acute ischemic stroke and acute arterial occlusion. Use of thrombolytics reduces the extent of cellular damage from blockage.
Adverse Reactions
Bleeding is the most obvious adverse effect. Dysrhythmias, hypotension (low blood pressure), polyneuropathy, cholesterol embolism, pulmonary embolism, and hypersensitivity are all possible effects.
Drug Interactions
Administering these products together with other anticoagulants may increase the potential for bleeding.
 Nursing Implications and Patient Teaching
Nursing Implications and Patient Teaching
n Assessment
These medications are given by the physician in life-threatening situations of vascular block caused by thrombosis. They are most helpful if administered within the first hour after the thrombosis.
Learn as much as possible about the health history of the patient. Through talking to the patient or other primary witnesses, attempt to determine the exact time sequence of events and what happened before the patient was seen. Determine whether any other medications have been taken. For example, because aspirin helps reduce platelet adhesion, patients who are suspected of having a myocardial infarction are urged to chew a 325-mg aspirin (ASA) tablet. Obtain the history of any recent surgery.
n Diagnosis
What other factors in addition to the medical diagnosis are important? Does this patient have risk factors for bleeding, myocardial infarction, stroke, or pulmonary emboli? This patient is probably very frightened and anxious, as well as seriously ill. Accompanying worries about finances, career, and family may arise.
n Planning
These medications come as a powder that requires reconstitution. Are all the equipment and materials the physician will require for infusion present?
n Implementation
Carefully monitor the vital signs of the patient receiving thrombolytic therapy. Report these findings frequently to the physician or other health care provider.
n Evaluation
Observe the patient carefully for bleeding. Bleeding may be superficial, coming from the infusion site. Other more significant bleeding indicates overdose and is shown by hematuria (blood in the urine), hematemesis (blood in the vomitus), signs of abdominal tension, and internal bleeding.
n Patient and Family Teaching
Explain the basis of thrombolytic therapy to the patient and family as necessary. Make sure the physician speaks with them about what is being done.
Antiplatelet Agents
Action
Through a variety of mechanisms, these products act to limit or inhibit platelet aggregation (clumping) and thus reduce thrombus formation.
Uses
ASA reduces the incidence of myocardial infarction–related deaths in men older than 50 years of age. ASA is the drug of choice in ischemic stroke; it plays no role in hemorrhagic stroke.
Clopidogrel (Plavix) is used for myocardial infarction prophylaxis for men and as additional or adjunct therapy with thrombolytics in preventing infarction or stroke. Abciximab (ReoPro), eptifibatide (Integrilin), bivalirudin (Angiomax), and a variety of other specialty products may be used during cardiac catheterization or other cardiovascular procedures.
Adverse Reactions
Bleeding is the most frequently seen adverse event. Diarrhea, nausea, dyspepsia (stomach discomfort after eating), rash, GI pain, neutropenia, purpura (bruising), vomiting, flatulence, pruritus (itching), dizziness, and anorexia (lack of appetite) are also seen.
Drug Interactions
Variable interactions with antacids, cimetidine, digoxin, and theophylline are possible.
 Nursing Implications and Patient Teaching
Nursing Implications and Patient Teaching
n Assessment
These drugs are used in critically ill patients to help limit damage from thrombosis or occlusion. The nurse will be involved in monitoring vital signs and assisting with monitoring the patient’s cardiovascular status.
n Diagnosis
Evaluate for changes in level of consciousness, renal function, and respiration. Be alert for any signs of bleeding.
n Planning
Have all materials available for monitoring the patient’s vital signs and for giving medications.
n Implementation
Assist in recording the medications given and the patient’s response. Assist in the ordering and collection of any blood work required to monitor therapy.
n Evaluation
Changes in vital signs and levels of consciousness provide important feedback about the status of blood circulation.
n Patient and Family Teaching
Assist in calming the patient, explaining the situation to the family, and providing information. Some of these medications may be given orally over time to help maintain a good circulation.