CHAPTER 20. ARTHROCENTESIS OF THE KNEE
Indications165
Contraindications166
Equipment166
Practical procedure166
Post-procedure investigations169
Complications169
The Libellus de Medicinalibus Indorum Herbis (or ‘little book of the medicinal herbs of the Indians’, originally an Aztec herbal manuscript composed in 1552 in Nahuatl which was translated into Latin) described puncturing the swollen joint with the bone of an eagle or a lion. The original book no longer exists but its translation was presented as a gift to Prince Philip (the future Philip II) of Spain. However, after several further owners and via a circuitous route over the centuries it ended up in the Vatican library. In 1990 Pope John Paul II returned it to Mexico.
INTRODUCTION
The aspiration and examination of fluid from the knee is fundamental to the investigation of an acute knee monoarthritis. The technique employed in arthrocentesis may also be employed for therapeutic purposes, although these should be performed by a specialist (rheumatologist or orthopaedic surgeon).
INDICATIONS
THERAPEUTIC
Only to be performed by a specialist:
• Intra-articular steroid or local anaesthetic administration (contraindicated in a suspected or confirmed septic joint).
• Drainage of a tense haemarthrosis.
• Drainage of a septic joint.
CONTRAINDICATIONS
• Lack of consent.
• Coagulopathy (should be corrected before aspiration to reduce the risk of haemarthrosis).
• Skin infection at the intended puncture site.
• Joint prosthesis (discuss the case with an orthopaedic surgeon).
EQUIPMENT
• Sterile gloves.
• Dressing pack.
• Chlorhexidine cleaning solution.
• Skin pen.
• Gauze.
• Orange needle.
• 2 × Green needle.
• 5 mL syringe.
• 20 mL syringe.
• Lidocaine.
• 3 × specimen pots.
• 1 × fluoride oxalate blood Vacutainer® (glucose).
PRACTICAL PROCEDURE
• Explain the procedure to the patient and obtain consent.
• Position the patient on a couch with the knee supported over pillows. This enables the quadriceps muscles to relax and the knee to be supported in a mildly flexed position, thus opening up the knee joint.
• Wash your hands and wear sterile gloves.
• Prepare the equipment on a sterile trolley.
• The procedure is most commonly performed from the lateral approach. Palpate the knee joint, identifying the patella and in particular its most supero-lateral aspect. Mark the point 1cm above and 1cm lateral to the supero-lateral aspect of the patella (Fig. 20.1).
• Fill the 5 mL syringe with lidocaine via a green needle.
• Infiltrate local anaesthetic subcutaneously at the point identified above with an orange needle.
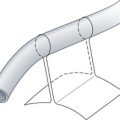
• Now infiltrate local anaesthetic with a green needle into deeper tissues, advancing the needle slowly at a 45 degree angle infero-medially under the patella until you aspirate fluid (Fig. 20.2). You may feel a slight ‘give’ as the needle enters the joint cavity. Allow a few minutes for the anaesthetic to take effect.
 Tip Box
Tip Box
If the patient experiences pain or there is resistance, the needle may be hitting the highly innervated periosteal or cartilaginous surfaces. Simply withdraw the needle slightly and realign the angle or direction of your subsequent approach.
 Tip Box
Tip Box
If you cannot aspirate synovial fl uid, try changing the position of the needle. Gently withdraw the needle and insert at a different angle aiming inferomedially behind the patella. Alternatively, change the position of the patient. Ask them to sit on the edge of a bed with their feet on a stool or on a chair. This opens up the articulating surfaces a little more to gain access to the joint.
• Attach a clean green needle to the 20 mL syringe. Insert the needle at the point 1cm above and 1cm lateral to the supero-lateral aspect of the patella and advance along the same anaesthetized track (directed at a 45 degree angle infero-medially under the patella) whilst aspirating to confirm entry to the synovium.
• Gently aspirate the synovial fluid either until the required volume for investigations is obtained, or to dryness for symptomatic relief.
 Tip Box
Tip Box
Once the needle has entered the joint cavity, resistance to further aspiration or an apparently premature cessation of aspiration may result from turbid synovial fluid containing fibrin strands or debris. Try withdrawing the needle slightly and re-aspirate, or inject a small volume of synovial fluid to clear the needle. Alternatively, a larger-bore needle may be required to aspirate thick exudative effusions.
 Tip Box
Tip Box
Compress the suprapatellar pouch, the patella itself and the medial aspect of the joint with your non-dominant hand whilst aspirating the knee to aid arthrocentesis and thus fully drain the joint effusion.
 Tip Box
Tip Box
Having drained the synovial fluid, take care that when the joint surfaces come into apposition the needle tip does not cause local trauma.
• When enough synovial fluid has been obtained, withdraw the needle and place a small plaster over the puncture site.
• Prescribe adequate analgesia.
POST-PROCEDURE INVESTIGATIONS
• Macroscopic appearances:
— Normal or non-inflammatory states – clear, straw-coloured fluid.
— Haemarthrosis – bloody fluid.
— Septic arthritis – cloudy, turbid fluid.
— Inflammatory arthritis (crystal arthropathy, rheumatoid arthritis) – cloudy, turbid fluid.
• Microbiology:
— Cell count – raised white cells (neutrophils) in septic arthritis and crystal arthropathies.
— Gram stain.
— Microscopy, culture and sensitivity.
— Alcohol- and acid-fast bacilli + Ziehl–Nielson/Auramine staining.
• Biochemistry:
— Protein – high (>4 g/dL) in inflammatory or purulent effusions.
— Glucose (with concurrent serum glucose sample) – comparatively low to serum glucose in inflammatory or purulent effusions.
— LDH – high in inflammatory or purulent effusions.
• Microscopy under polarized light (for crystal arthropathies):
— Gout – negatively bi-refringent needle-like crystals.
— Pseudogout – weekly positive bi-refringent rhomboidal crystals.
COMPLICATIONS
• Bleeding (either superficial or intra-articular).
• Infection (either superficial or intra-articular) – a rare complication when strict aseptic technique is observed, although much increased when overlying infection (a contraindication to arthrocentesis) is present.
• Dry tap.
• Pain.