CASE 20

1. Which of the following are considered significant limitations for CT angiography of the coronary arteries? (Choose all that apply.)
D. Radiation
2. What is the finding in the right coronary artery?
B. 50% stenosis
C. 30% stenosis
D. Normal
3. What is the next best step in management assuming the other coronary arteries were normal?
A. Do nothing
C. Diagnostic catheter angiogram
4. What is the gold standard for characterization of coronary plaque?
B. MRI
ANSWERS
CASE 20
References
Sundaram B, Patel S, Agarwal P, et al. Anatomy and terminology for the interpretation and reporting of cardiac MDCT: part 2, CT angiography, cardiac function assessment, and noncoronary and extracardiac findings. AJR Am J Roentgenol. 2009;192(3):584–598.
Sundaram B, Patel S, Bogot N, et al. Anatomy and terminology for the interpretation and reporting of cardiac MDCT: part 1, structured report, coronary calcium screening, and coronary artery anatomy. AJR Am J Roentgenol. 2009;192(3):574–583.
Cross-Reference
Cardiac Imaging: The REQUISITES, ed 3, pp 248–261.
Comment
Imaging
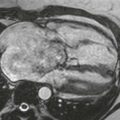
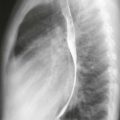
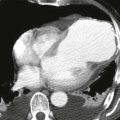
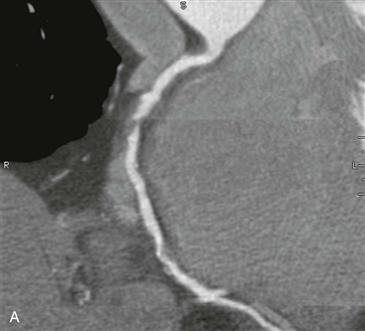
This patient presented to the emergency department with atypical chest pain and was deemed to be at low to intermediate risk for coronary artery disease. The patient was triaged with triple rule-out CT angiography of the thorax to exclude coronary artery disease, pulmonary embolism, and aortic dissection. This examination revealed no pulmonary embolism or aortic dissection. Two multiplanar reformatted images of the right coronary artery showed a focal high-grade stenosis (approximately 80%) composed entirely of noncalcified plaque (Figs. A and B). Subsequently, the patient underwent diagnostic cardiac catheterization, which confirmed right coronary artery stenosis. A successful balloon angioplasty with stent placement was performed with resolution of the patient’s symptoms.
Utility
Millions of people present to the emergency department annually with the complaint of chest pain. Only 20% to 25% of these patients are found to have a coronary etiology of their pain at the time of discharge. CT angiography can be used to triage these patients rapidly and diagnose important extracardiac causes of chest pain. It is ideally used in patients with a low or intermediate pretest probability of disease based on their risk factors and clinical presentation. A positive examination (i.e., coronary stenosis ≥50%) must be confirmed with diagnostic catheterization, whereas a negative examination (i.e., any stenosis <50%) needs no further testing because the lesion is unlikely to be the cause of the patient’s chest pain.