CASE 2 LAD-Diagonal Bifurcation Lesion
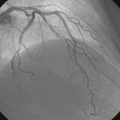
Cardiac catheterization
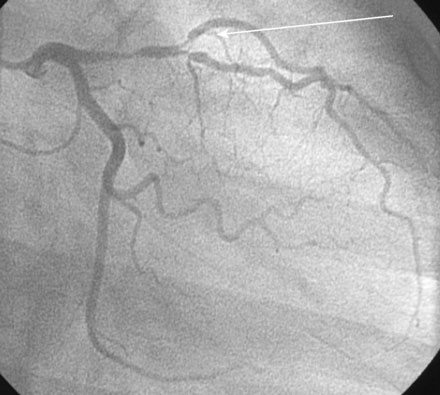
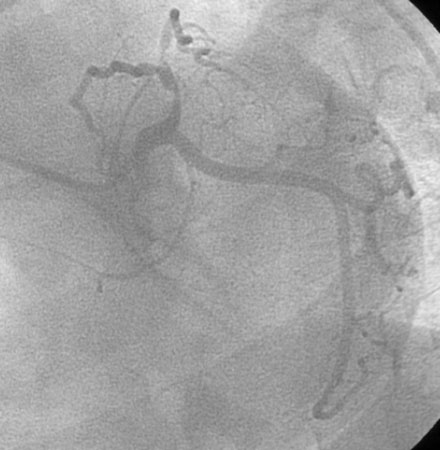
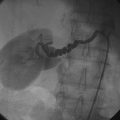
Cardiac catheterization revealed a complex 90% stenosis of the left anterior descending (LAD) artery at the bifurcation of a first diagonal branch (D1). The stenosis extended proximal and distal to the D1 branch; in addition, the D1 branch had an 80% stenosis at the ostium (Figures 2-1, 2-2 and Videos 2-1, 2-2, 2-3). No other significant lesions were observed (Figure 2-3), and left ventricular function was preserved.
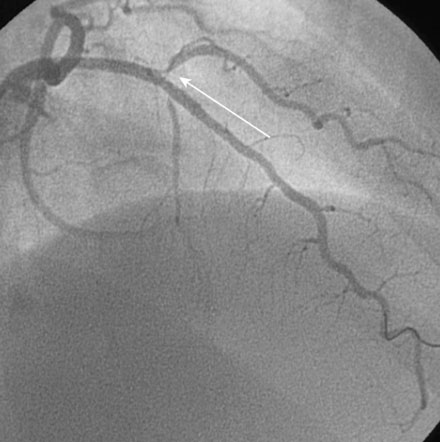
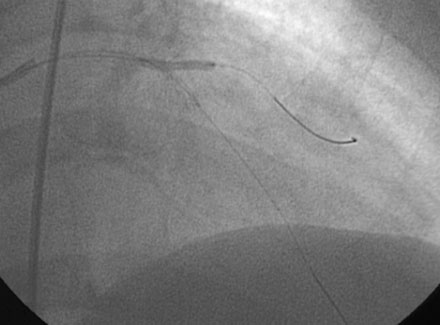
The physician chose to treat the artery percutaneously. Using bivalirudin as the procedural anticoagulant, a 6F Judkins left guide coronary catheter with 4 cm curve (JL4) was used to engage the left coronary artery. A 180 cm long, 0.014” floppy-tipped guidewire was advanced into the LAD and the lesion directly stented using a 2.5 mm diameter, 25 mm long sirolimus-eluting stent. This resulted in an excellent angiographic result in the LAD (Figure 2-4 and Video 2-4). A second floppy-tipped guidewire was positioned in the first diagonal branch, passing through the LAD stent. The diagonal stenosis was first dilated with a 2.5 mm diameter by 15 mm long compliant balloon (Figure 2-5) but this produced a suboptimal result at the ostium (Figure 2-6 and Video 2-5). Thus, a 2.5 mm diameter by 18 mm long sirolimus-eluting stent was positioned at the ostium and deployed (Figure 2-7). The final angiographic result is shown in Figure 2-8 and Video 2-6.
Discussion
Atherosclerotic lesions involve the bifurcation of a major side branch in up to 15% of percutaneous coronary interventions, creating significant challenges to the operator. Compared to nonbifurcation lesions, bifurcation lesions are associated with a higher risk of ischemic complications including periprocedural infarction, primarily due to loss of the side branch. Bifurcation lesions are also associated with a higher risk of stent thrombosis and restenosis, particularly if more than one stent is incorporated into the bifurcation.1,2
Several classification schemes have been described.3 The Medina classification system (Figure 2-9) uses the number 1 to describe the presence of greater than a 50% stenosis in each of the following three segments in this order: proximal main vessel, distal main vessel, and side branch. Thus, a bifurcation lesion consisting of greater than 50% narrowing of the proximal main vessel and distal main vessel, but sparing the side branch, would be described as 1,1,0.
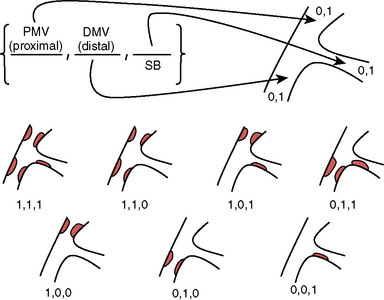
FIGURE 2-9 Medina classification system for coronary bifurcations (from reference 3). PMV = proximal main vessel, DMV = distal main vessel, SB = side branch.
The risk and outcome of an intervention in the setting of a bifurcation stenosis depends on the lesion morphology and the size of the side branch. Disease involving both sides of the bifurcation as well as the ostium of the side branch (Medina Classification 1,1,1) is associated with the highest risk for side branch occlusion, due to redistribution of atherosclerotic plaque (or plaque “shift”).4 The loss of a major side branch may result in serious sequelae including periprocedural myocardial infarction and its associated complications.
A variety of techniques have been proposed to treat bifurcation lesions. Placement of two wires, one in the main artery and a second in the side branch, prior to angioplasty is a standard approach and can help maintain patency after balloon angioplasty. However, in the event of closure after stenting, this wire cannot be used for balloon angioplasty or stenting of the side branch because it lies trapped behind the stent in the main artery. This second wire may maintain patency, however, allowing the operator to identify the location of the side branch ostium and guiding the placement of another guidewire through the stent struts. Debulking techniques using either directional or rotational atherectomy, the use of “kissing” balloons, and a variety of side branch stent configurations (“V,” “Y,” “T,” and “crush stent” configurations) have been developed and advocated by their proponents to prevent loss of the side branch in bifurcation lesions. The optimal treatment of any given bifurcation lesion may incorporate one or more of these techniques; however, recent randomized controlled trials suggest that bifurcation lesions can first be managed with a simple approach of stenting only the main vessel with provisional stenting of the side branch performed only if an unacceptable result is obtained.5,6 When this strategy is adopted, a second stent is necessary in the side branch in only one third of cases.6 The case presented here represented a true bifurcation lesion with disease on both sides of the side branch and significant disease involving the side branch ostium. After stenting the parent vessel, the side branch remained patent but significantly narrowed and balloon angioplasty led to a suboptimal result, leading to placement of the stent in a “V” configuration and an excellent angiographic and long-term clinical result.
1 Al Suwaidi J., Yeh W., Cohen H.A., Detre K.M., Williams D.O., Holmes D.R.Jr. Immediate and one year outcome in patients with coronary bifurcation lesions in the modern era (NHLBI dynamic registry). Am J Cardiol. 2001;87:1139-1144.
2 Yamashita T., Nishida T., Adamian M.G., Briguori C., Vaghetti M., Corvaja N., Albiero R., Finci L., DiMario C., Tobis J.M., Colombo A. Bifurcation lesions: two stents versus one stent: immediate and follow-up results. J Am Coll Cardiol. 2000;35:1145-1151.
3 Louvard Y., Thomas M., Dzavik V., Hildick-Smith D., Galassi A.R., Pan M., Burzotta F., Zelizko M., Dudek D., Ludamn P., Sheiban I., Lassen J.F., Darremont O., Kastrati A., Ludwig J., Iakovou I., Brunel P., Lansky A., Meerkin D., Legrand V., Medina A., Lefevre T. Classification of coronary artery bifurcation lesions and treatments: time for a consensus!. Catheter Cardiovasc Interv. 2008;71:175-183.
4 Aliabadi D., Tillis F.V., Bowers T.R., Benjuly K.H., Safian R.D., Goldstein J.A., Grines C.L., O’Neill W.W. Incidence and angiographic predictors of side branch occlusion following high-pressure intracoronary stenting. Am J Cardiol. 1997;80:994-997.
5 Steigen T.K., Maeng M., Wiseth R., et al. Nordic PCI Study Group Randomized study on simple versus complex stenting of coronary artery bifurcation lesions: the Nordic Bifurcation Study. Circulation. 2006;114:1955-1961.
6 Colombo A., Bramucci E., Sacca S., Violini R., Lettieri C., Zanini R., Sheiban I., Paloscia L., Grube E., Schofer J., Bolognese L., Orlandi M., Niccoli G., Latib A., Airoldi F. Randomized study of the crush technique versus provisional side-branch stenting in true coronary bifurcations. The CACTUS (Coronary Bifurcations: Application of the Crushing Technique Using Sirolimus Eluting Stents) Study. Circulation. 2009;119:71-78.